The optimal revascularization strategy in patients with complex coronary artery disease and non–ST-segment elevation acute coronary syndromes is undetermined. In this multicenter, prospective registry, 4,566 patients with non–ST-segment elevation myocardial infarctions, unstable angina, and multivessel coronary disease, including left main disease, were enrolled. After angiography, 3,033 patients were selected for stenting (10.3% received drug-eluting stents) and 1,533 for coronary artery bypass grafting. Propensity scores were used for baseline characteristic matching and result adjustment. Patients selected for percutaneous coronary intervention (PCI) were younger (mean age 64.4 ± 10 vs 65.2 ± 9 years, p = 0.03) and more frequently presented with non–ST-segment elevation myocardial infarctions (32.0% vs 14.5%, p = 0.01), cardiogenic shock (1.5% vs 0.7%, p <0.01), and history of PCI (13.1% vs 5.5%, p <0.01) or coronary artery bypass grafting (10.6% vs 4.6%, p <0.01). European System for Cardiac Operative Risk Evaluation scores were higher in PCI patients (5.4 ± 2 vs 5.2 ± 2, p <0.01). Patients referred for coronary artery bypass grafting more often presented with triple-vessel disease and left main disease (82.2% vs 33.8% and 13.7% vs 2.4%, respectively, p <0.01). After adjustment, 929 well-matched pairs were chosen. Early mortality was lower after PCI before matching (2.1% vs 3.1%, p <0.01), whereas after balancing, there was no difference (2.5% vs 2.8%, p = 0.62). Three-year survival was in favor of PCI compared with surgery before (87.5% vs 82.8%, hazard ratio 1.44, 95% confidence interval 1.2 to 1.7, p <0.01) and after (86.4% vs 82.3%, hazard ratio 1.33, 95% confidence interval 1.05 to 1.7, p = 0.01). Stenting was associated with improved outcomes in the following subgroups: patients aged >65 years, women, patients with unstable angina, those with European System for Cardiac Operative Risk Evaluation scores >5, those with Thrombolysis In Myocardial Infarction (TIMI) risk scores >4, those receiving drug-eluting stents, and those with 2-vessel disease. In conclusion, in patients presenting with non–ST-segment elevation acute coronary syndromes and complex coronary artery disease, immediate stenting was associated with lower mortality risk in the long term compared with surgical revascularization, especially in subgroups at high clinical risk.
Highlights
- •
The optimal revascularization strategy in patients with non–ST-segment elevation acute coronary syndromes and multivessel coronary artery disease is unknown.
- •
In a large, hypothesis-generating, prospective registry, the investigators evaluated 3-year outcomes in this cohort of patients assigned to immediate stenting or coronary artery bypass grafting.
- •
At 3-year follow-up, after adjustment for patients’ baseline characteristics, immediate stenting compared with surgical revascularization was associated with higher survival probability (87.5 vs 82.8%, HR 1.44, 95% CI 1.2 to 1.7, p <0.01).
- •
This benefit was highlighted in subpopulations at high clinical risk.
Within the past decade, aging of the population and the coexistence of multiple co-morbidities have increased the risk of patients presenting with acute coronary syndromes (ACS). Furthermore, a steady decrease in the incidence of ST-segment elevation ACS and an increase in that of non–ST-segment elevation ACS (NSTE-ACS) have been observed, the latter of which has been shown to be associated with a poorer long-term prognosis. This is related to the complexity of coronary artery disease in patients with NSTE-ACS, with nearly half of patients presenting with multivessel coronary artery disease (MVD). The optimal revascularization strategy in this group of patients is undetermined. Because of clinical presentation, in most patients, an early or a delayed invasive strategy is preferred in American and European guidelines, but the method of revascularization is not specified. Because of high surgical risk, immediate stenting of the culprit lesion and delayed complete percutaneous revascularization are becoming common practice. In contrast, on the basis of anatomic criteria, coronary artery bypass grafting (CABG) should be the standard of care. Very few studies have addressed thus far the problem of the optimal revascularization strategy in patients presenting with MVD and NSTE-ACS. A hypothesis of a positive outcome can be derived from some previous studies comparing bare-metal stenting and CABG, in which most patients presented with NSTE-ACS. Therefore, we aimed to compare early and long-term outcomes after immediate stenting versus referral for surgical revascularization after urgent coronary angiography in this challenging cohort of patients.
Methods
In this multicenter, prospective registry, 4,566 consecutive patients hospitalized with NSTE-ACS and MVD were enrolled from 2006 to 2009. All patients underwent urgent cardiac catheterization in 6 interventional cardiology departments of American Heart of Poland, without cardiac surgery on site. Surgical revascularizations were carried out at 3 cardiac surgery reference centers (the Silesian Center for Heart Diseases in Zabrze, Voivodiship Hospital in Opole, and the Upper Silesian Heart Center of the Medical University of Silesia in Katowice).
Adult patients (>21 years of age) with the whole risk spectrum of NSTE-ACS, defined as unstable angina and non–ST-segment elevation myocardial infarction (NSTEMI), were included. Furthermore, the following angiographic criteria had to be met: ≥2 lesions with >70% diameter stenosis confirmed by on-line quantitative coronary angiography in native coronary arteries with the involvement of both the right and left coronary arteries (left anterior descending or circumflex). Patients with coexistence of both protected and unprotected left main disease (>50% diameter stenosis) were also enrolled. We excluded patients with ST-segment elevation myocardial infarction and stable angina on admission, the presence of only single-vessel disease, coexistence of significant valvular disease, designation for hybrid revascularization (percutaneous coronary intervention [PCI] plus CABG) or plain balloon angioplasty.
After immediate coronary angiography (<48 hours after symptom onset), the decision as to whether the patient should undergo bypass surgery or multistage stenting was based on anatomic suitability for PCI, estimation of surgical and clinical risk, or patient preference. All decisions regarding referral for CABG were based on consensus between the surgeon and interventionalist on the basis of teleconferencing and on-line Digital Imaging and Communications in Medicine data transmission using TeleDICOM software (Distributed Systems Research Group, Kraków, Poland). Interventional centers did not have on-site surgical backup at that time, but they were located within ≤1-hour emergency transportation to a reference cardiac surgery department. Group assignment and analysis were based on intention to treat.
In the percutaneous arm, multistage revascularization was the preferred strategy. Initial stenting of the culprit lesion was performed in all patients except those in cardiogenic shock. Second-stage and, if necessary, third-stage procedures on the remaining lesions were planned within 3 to 4 weeks, with the intention of attaining complete revascularization. In patients with high-risk NSTE-ACS stenting was performed ad hoc, otherwise the coronary angiography procedure was delayed (up to 24 hours). In patients selected for stenting, a clopidogrel loading dose (600 mg) was administered during or immediately after the intervention. During the procedure, patients received unfractionated heparin 100 IU/kg intravenously, which was corrected to maintain an activated clotting time >300 seconds. Use of glycoprotein IIb/IIIa receptor inhibitors was at the operator’s discretion. All patients were advised to continue taking aspirin indefinitely and clopidogrel for ≥1 year after the procedure. Direct stenting was the preferred technique, except for critical and calcified lesions, which were predilated with a small balloon (2.0 to 2.5 mm). Provisional stenting of a side branch was the favored strategy for bifurcation revascularization, followed by kissing balloon postdilation. Intra-aortic balloon pumping was applied in patients with complex lesions and significantly depressed left ventricular function (left ventricular ejection fraction <30%) or cardiogenic shock. The use of intravascular ultrasound and drug-eluting stents (DES) was at the discretion of the operator.
Patients were transferred to the nearest cardiac surgery department with emergency medical services. There were no reported deaths or serious adverse events related to delays caused by transportation to the cardiac surgery department. Surgical procedures were performed using standard anesthetic techniques, through a median sternotomy, with standard cardiopulmonary bypass and moderate systemic hypothermia. Arterial revascularization with left internal thoracic artery to left anterior descending coronary artery was the preferred strategy. Dual-antiplatelet therapy was endorsed for 1 year after surgery and aspirin indefinitely.
Long-term survival at 3 years was the primary end point of this study. Early (30-day) mortality was considered the secondary end point. Because of the observational nature of this study, no initial hypotheses were generated. European System for Cardiac Operative Risk Evaluation (EuroSCORE) and Thrombolysis In Myocardial Infarction (TIMI) risk scores were calculated using previously described criteria. Definitions of low- and high-risk NSTE-ACS were based on European Society of Cardiology guidelines on myocardial revascularization. Chronic kidney disease was defined as a glomerular filtration rate <60 ml/min according to Modification of Diet in Renal Disease score. Hypertension was defined as self-reported treatment for high blood pressure with 1 of 6 common classes of antihypertensive medications or systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg. Current smoking and family history of heart attack were ascertained by questionnaire. Presence of diabetes mellitus was based on self-reported physician diagnosis, use of insulin or an oral hypoglycemic agent, or a fasting glucose value ≥126 mg/dl at baseline examination. Presence of dyslipidemia was based on self-reported physician diagnosis, use of hypolipidemic agents, or abnormal concentration of lipids or lipoproteins in the blood. Obesity was defined as body mass index >30 kg/m 2 .
Clinical data from all patients were prospectively recorded on dedicated case report forms and submitted to the computerized Polish Registry of Acute Coronary Syndromes (PL-ACS). Data recording was audited by institutional quality assurance and the PL-ACS by the National Health Fund. All included centers were current and possessed quality assurance ISO-9001 certificates and were additionally audited by National Health Fund. Follow-up data on all-cause mortality were obtained annually from the National Health System registry and the Central Registry of Citizens, guaranteeing complete data collection.
PCI procedures were carried out by experienced interventional cardiology teams at high-volume centers (>1,000 PCIs per year at 1 center, with 300 interventions per operator) without cardiac surgery backup on site but within 60 minutes by emergency transportation. All interventionists underwent special training in left main and multivessel stenting, on the basis of a previously published protocol.
Normally distributed parametric data are expressed as a mean ± SD. Nonparametric data are presented as absolute numbers and percentages. Chi-square tests were used for comparisons of nonparametric data, and Student’s t tests were used for normally distributed parametric data. Survival and event-free survival curves were estimated using Kaplan-Meier analysis with a log-rank test for comparison of curves. A p value ≤0.05 was considered statistically significant. Because of the nonrandomized nature of the study, propensity score–matching analysis was used to adjust for differences in patients’ baseline characteristics. The logistic regression model predicting PCI and CABG assignment was used. Matching was performed by randomly selecting a PCI patient and looking for the CABG patient with the nearest logit-transformed propensity score. The standardized difference was calculated for all baseline covariates. Model discrimination was assessed with C statistics. Using estimated rates of survival in patients who underwent PCI and in those who underwent CABG, we calculated risk ratios at specific time points and used bootstrap methods to obtain 95% confidence intervals. Analysis of PCI versus CABG was by intention to treat. The comparison of CABG with PCI was performed in the overall population and in prospectively defined subgroups and is presented as hazard ratios and 95% confidence intervals.
Results
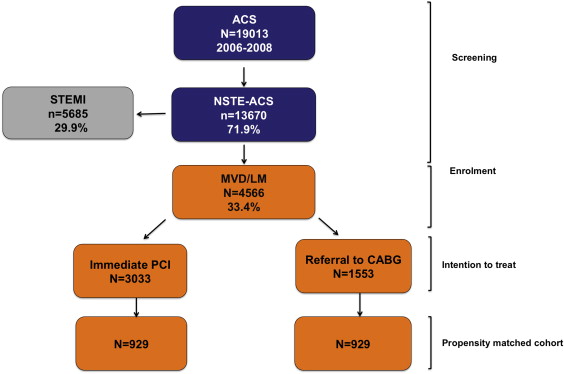
The study flowchart is presented in Figure 1 . From January 2006 until December 2009, 19,013 patients were screened, diagnosed, and treated for ACS at 6 centers of American Heart of Poland. After coronary angiography, 4,566 patients (27.9%) were enrolled and 3,033 qualified for stenting, whereas 1,533 were referred for surgical revascularization. The study population’s baseline characteristics are listed in Table 1 . Patients selected for PCI presented twice as often with NSTEMI, cardiogenic shock, and history of PCI or CABG. The EuroSCORE and TIMI risk score were higher on average by 10% in PCI patients. Patients selected for CABG presented more often with triple-vessel (by 3 times) and left main disease (by 4 times) compared with those who underwent stenting. Otherwise, the proximal left anterior descending coronary artery was revascularized twice as often with stenting. The propensity score used to identify a matched CABG cohort showed very good discriminative power (C statistic 0.82). After matching, 929 pairs were selected, in which bias was reduced in all variables and standardized difference was <5% and not significant in all covariates ( Table 2 ). The population characteristics after balancing were similar as in crude analysis, but with more patients with unstable angina (80%). Furthermore, patients with 2-vessel disease in the PCI group were excluded, and the cohort consisted mostly of those with 3-vessel disease (70%). The occurrence of left main disease was similar to that in the general population (5%). The mean time from admission to PCI was 6.6 ± 3.2 hours. Percutaneous revascularization was performed by using femoral access in all patients, and techniques described in the “Methods” section. DES were used in 313 patients (10.2%), glycoprotein IIb/IIIa inhibitors were used in 40 (3.5%), and intra-aortic balloon pumping was used in 27 (1.3%). Multistage PCI was performed in all patients except those in cardiogenic shock (0.9%), in whom complete revascularization was performed ad hoc.
| Variable | PCI n = 3033 | CABG n = 1553 | p |
|---|---|---|---|
| Age (years) | 64.4 ± 10 | 65.2 ± 9.3 | 0.01 |
| Men | 70.1% | 72.2% | 0.14 |
| Hypertension | 82.3% | 83.5% | 0.33 |
| Dyslipidemia | 60.2% | 69.5% | <0.01 |
| Diabetes mellitus | 27.5% | 26.3% | 0.39 |
| Congestive heart failure | 1.1% | 1.4% | 0.37 |
| Chronic kidney disease | 5.1% | 4.7% | 0.51 |
| Peripheral arteries disease | 6.8% | 6.4% | 0.62 |
| Obesity | 22.9% | 29.6% | <0.01 |
| Current smoker | 40.3% | 45.0% | <0.01 |
| Previous myocardial infarction | 30.1% | 30.6% | 0.72 |
| Previous CABG | 10.6% | 4.3% | <0.01 |
| Previous PCI | 13.1% | 5.5% | <0.01 |
| NSTEMI | 32.0% | 14.5% | <0.01 |
| Unstable angina | 68.0% | 85.5% | <0.01 |
| Ejection fraction (%) | 51.8 ± 10.3 | 51.8 ± 10.9 | 0.84 |
| Euroscore (additive) | 5.36 ± 2.3 | 5.16 ± 2.0 | <0.01 |
| TIMI risk score | 3.87 ± 1.0 | 3.79 ± 1.0 | 0.01 |
| Killip class: | |||
| 1 | 94.0% | 95.4% | 0.06 |
| 2 | 4.2% | 3.9% | 0.56 |
| 3 | 0.9% | 0.6% | 0.38 |
| 4 | 0.9% | 0.1% | <0.01 |
| Cardiac arrest | 1.5% | 0.7% | 0.02 |
| Angiographic and lesion characteristics: | |||
| Left Main Coronary Artery | 2.4% | 13.7% | <0.01 |
| LAD proximal | 21.5% | 11.1% | <0.01 |
| LAD- medial and distal | 16.0% | 4.4% | <0.01 |
| LCx | 26.4% | 4.6% | <0.01 |
| RCA | 30.4% | 9.0% | <0.01 |
| Two vessel coronary artery disease | 66.2% | 17.8% | <0.01 |
| Three vessel coronary artery disease | 33.8% | 82.2% | <0.01 |
| In-stent restenosis | 4.3% | 3.2% | 0.21 |
| Saphenous vein graft or LIMA | 2.4% | 0.6% | <0.01 |
| Variable | PCI (n = 929) | CABG (n = 929) | p | Standardized Difference |
|---|---|---|---|---|
| Age (years) | 65.3 ± 9.9 | 65.2 ± 9.9 | 0.92 | 0.44% |
| Men | 71.7% | 70.3% | 0.51 | 3.08% |
| Hypertension | 84.3% | 83.7% | 0.75 | 1.47% |
| Hypercholesterolemia | 66.0% | 64.7% | 0.56 | 2.71% |
| Diabetes mellitus | 28.8% | 28.4% | 0.84 | 0.95% |
| Obesity | 27.0% | 25.7% | 0.53 | 2.93% |
| Congestive heart failure | 1.1% | 1.4% | 0.53 | −2.9% |
| Chronic kidney disease | 5.8% | 5.2% | 0.54 | 2.8% |
| Peripheral arteries disease | 7.9% | 6.4% | 0.21 | 5.8% |
| Current smoker | 43.3% | 40.9% | 0.30 | 4.80% |
| Previous myocardial infarction | 30.1% | 30.4% | 0.92 | −0.47% |
| Previous CABG | 5.7% | 5.2% | 0.61 | 2.37% |
| Previous PCI | 7.8% | 8.1% | 0.80 | −1.20% |
| NSTEMI | 20.0% | 20.2% | 0.91 | −0.54% |
| Unstable angina | 80.0% | 79.8% | 0.91 | 0.54% |
| Ejection fraction (%) | 51.8 ± 10.2 | 51.6 ± 11.2 | 0.80 | 1.58% |
| Euroscore (additive) | 5.2 ± 2.1 | 5.3 ± 2.0 | 0.82 | −1.04% |
| TIMI score | 3.8 ± 1.0 | 3.8 ± 1.0 | 0.37 | −4.20% |
| Killip class: | ||||
| 1 | 95.7% | 94.7% | 0.33 | 4.54% |
| 2 | 3.3% | 4.2% | 0.33 | −4.53% |
| 3 | 0.6% | 1.0% | 0.44 | −3.63% |
| 4 | 0.3% | 0.1% | 0.32 | 4.81% |
| Cardiac arrest | 1.4% | 0.9% | 0.35 | 4.41% |
| Angiographic and lesion characteristics: | ||||
| Left main coronary artery | 5.7% | 5.1% | 0.54 | 2.86% |
| Proximal LAD involvement | 15.5% | 15.3% | 0.90 | 0.60% |
| Two vessel coronary disease | 30.6% | 28.3% | 0.29 | 4.96% |
| Three vessel coronary disease | 69.4% | 71.7% | 0.29 | −4.96% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


