Transthoracic echocardiography is the current standard for assessing aortic regurgitation (AR). AR severity can also be evaluated by flow measurement in the ascending aorta using cardiac magnetic resonance (CMR); however, the optimal site for flow measurement and the regurgitant fraction (RF) severity grading criteria that best compares with the transthoracic echocardiographic assessment of AR are not clear. The present study aimed to determine the optimal site and RF grading criteria for AR severity using phase-contrast flow measurements and CMR. A prospective observational study was performed of 107 consecutive patients who were undergoing CMR of the thoracic aorta. Using CMR, the AR severity and aortic dimensions were measured at 3 levels in the aorta (the sinotubular junction, mid-ascending aorta, and distal ascending aorta). The results were compared to the transthoracic echocardiographic grade of AR severity using multiple qualitative and quantitative criteria (grade 0, none; I+, mild; II+, mild to moderate; III+, moderate to severe; and IV+, severe). The mean RF values were significantly greater at the sinotubular junction than at the distal ascending aorta (13 ± 13.3% vs 9.4 ± 12.6%, respectively; p <0.001). The RF values that best defined AR severity using phase-contrast CMR were as follows: grade 0 to I+, <8%; grade II+, 8% to 19%; grade III+, 20 to 29%; and grade IV+, 30%) at the sinotubular or mid-ascending aorta. In conclusion, the quantitative RF values of AR severity using phase-contrast flow are best assessed in the proximal ascending aorta and differ from recognized quantitative echocardiographic criteria.
The severity of regurgitation is a predictor of clinical outcome in patients with chronic aortic regurgitation (AR), particularly in the presence of symptoms, if the left ventricle is severely dilated, or if left ventricular systolic function is impaired. Transthoracic echocardiography (TTE) is the imaging modality of choice for the serial assessment of AR severity. This is typically achieved by integrating several 2-dimensional and Doppler parameters to provide an overall severity grade.
Cardiac magnetic resonance (CMR) can also assess the severity of AR. In addition, it is the reference standard to serially evaluate the left ventricular size and function and dimensions of the thoracic aorta. The most commonly used method to assess AR severity using CMR relies on the phase-contrast assessment of anterograde and retrograde flow in the ascending aorta, thereby quantifying a regurgitant volume (RV) and regurgitant fraction (RF). Several previous studies have demonstrated the ability of CMR to quantitatively assess the degree of AR compared to TTE. However, differences exist in the assessment of AR by CMR and quantitative TTE in the published data, which can be a source of confusion. Thus, clinicians remain more comfortable with broad categories of AR severity (e.g., mild, moderate, or severe), which are easily compared to TTE, in contrast to the continuum provided by the RV and RF.
Another issue with previous reports is that the phase-contrast measurements have been performed at 1 position. It has been our observation that the position of the imaging slice for phase-contrast flow measurements influences the absolute measurement of RV using CMR. However, no study has evaluated the levels at which one can best distinguish the AR severity grade by the RF. Also, the size of the ascending aorta can potentially influence its flow patterns. In the present study, we aimed to (1) determine the RF and RV ranges using CMR that best agree with the transthoracic echocardiographic-defined qualitative grade of AR severity according to American Society of Echocardiography guidelines , (2) assess the level in the ascending aorta that best separate AR into grades of severity, and (3) identify the predictors that might contribute to differences in RF as measured using CMR and TTE.
Methods
Consecutive patients with and without AR, who had been referred for CMR evaluation of the thoracic aorta and were scheduled to undergo TTE (both occurred generally within 24 hours of each other), were enrolled in the present observational study from December 2008 to May 2009. Initially, 126 patients underwent CMR evaluation of the thoracic aorta in that period. Of these 126 patients, 19 had a prosthetic aortic valve, had undergone surgical grafting of the ascending aorta, or did not have echocardiography performed and were excluded. Thus, a total of 107 patients were included in the final analysis. The institutional review board approved the study.
All patients underwent CMR on a commercially available 1.5 Tesla scanner (Philips Achieva, 80 mT/m/ms gradient, 8-channel SENSE-XL-Torso coil, Philips Medical Systems, Best, The Netherlands). After the scout images, an axial, single shot, steady-state free precession, nonelectrocardiogram-gated stack of images was performed through the thorax during an end-expiratory breath-hold. steady-state free precession cine images of the ascending aorta were planned from the axial images in the following standardized orientations to allow visualization and facilitate planning of flows from all segments of the thoracic aorta: ascending and descending thoracic aorta, aortic arch, oblique coronal view through the aortic valve, left ventricular outflow tract, and through the aortic valve leaflets. In addition, standard 2-, 3-, 4-chamber and short-axis steady-state free precession cine images were obtained. The parameters used for the steady-state free precession cine images were repetition time 2.5 ms, TE 1.3 ms, flip angle 70°, field of view 300 × 260 mm, matrix 128 × 128, SENSE reduction factor 1.3, 30 phases per cardiac cycle, and a typical breath-hold of 12 seconds.
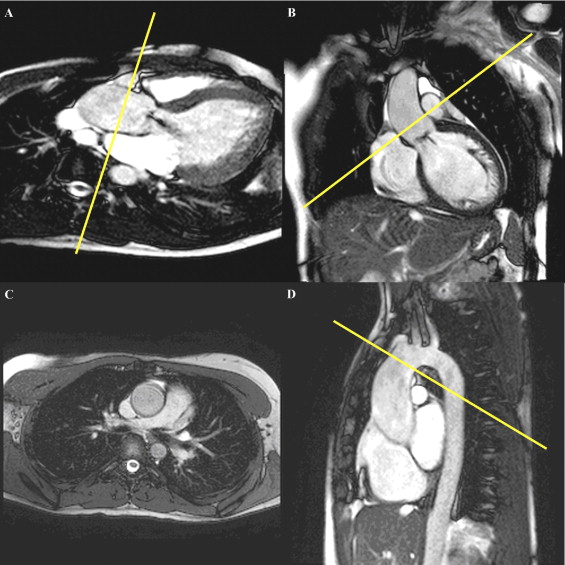
Quantitative through plane flow measurements in the ascending aorta were made using an electrocardiographically gated phase-contrast velocity sequence performed during a breath-hold at end expiration in 3 standardized and prespecified locations: (1) at the level of the sinotubular junction, (2) at the mid-ascending aorta at the level of the right pulmonary artery, and (3) at the distal ascending aorta, 1 cm proximal to the origin of the innominate artery ( Figure 1 ). The imaging planes were planned perpendicular to the aorta. The typical sequence parameters were repetition time 4.8 ms, echo time 2.8 ms, flip angle 12°, field of view 300 × 260 mm, matrix 128 × 98, SENSE reduction factor 2, 30 phases per cardiac cycle, and a typical breath-hold of 12 seconds. An encoding velocity of 200 cm/s was initially used. If aliasing was seen, the encoding velocity was increased by 50 to 100 cm/s until the aliasing was no longer seen.
Each patient underwent TTE by an experienced sonographer according to a standardized protocol using conventional commercially available echocardiographic machines (Phillips IE33, Andover, Massachusetts; GE Vivid 7 Dimension, General Electric, Milwaukee, Wisconsin). Assessment of AR severity was graded according to the American Society of Echocardiography guidelines. The following measurements were made: jet width/left ventricular outflow tract width ratio, AR jet pressure half time, the presence or absence of holodiastolic flow reversal in the proximal descending thoracic aorta, and end-diastolic flow reversal velocity in the proximal descending thoracic aorta. Qualitative grading of AR severity was categorized into the following grades using an integration of the parameters listed (as listed in the study by Zoghbi et al ): 0, no regurgitation; I+, mild; II+, mild to moderate; III+, moderate to severe; and IV+, severe regurgitation. Quantitative measures of RF and RV were available for 18 patients with grade ≥III+ AR.
Two readers (R.G. and R.R.), with >9 months of experience interpreting CMR studies, analyzed the phase-contrast flow data using the commercially available Philips Extended MR Workspace, version 2.6.3 software (Philips Medical Systems). A region of interest was manually traced around the ascending aorta on the magnitude images and propagated in the corresponding phase images in all acquired phases within the cardiac cycle. The anterograde and retrograde aortic flow volumes per RR interval were used to calculate the RF at the 3 levels in the ascending aorta. The maximum and minimum dimension of the ascending aorta was measured at each level. The morphology of the aortic valve was determined from the steady-state free precession cine images through the valve leaflets.
A physician (D.V.) trained in TTE to level 3 American Society of Echocardiography standards, who was unaware of the results of the CMR findings, reviewed and graded the degree of AR. He was also unaware of the previously reported clinical transthoracic echocardiographic reports.
Two physicians with level 3 American Society of Echocardiography training (R.G. and D.V.) independently reviewed 10 transthoracic echocardiographic studies and qualitatively graded AR severity. Similarly 2 physicians with level 3 CMR training (R.R. and R.G.) independently reviewed 15 phase-contrast flow measurements in 15 individual patients to evaluate interobserver variability. All measurements were done >1 month apart, in a blinded manner.
The baseline characteristics are descriptively summarized. The continuous variables are expressed as the mean ± SD and/or as the median and interquartile ranges, as appropriate. The categorical data are presented as the percentage frequency. Differences between groups were compared using the Student t test or analysis of variance (for parametric variables) and Wilcoxon signed rank test (for nonparametric variables) for continuous variables. The correlation between continuous variables was assessed using Spearman’s correlation coefficient. The agreement between ordinal variables was assessed using the κ statistic. Univariate and forward stepwise multivariate logistic regression analyses were performed to test the association between the dependent and multiple independent variables. For multivariate analyses, only those variables with p ≤0.1 were entered into the model. Data assembly and basic statistical comparisons were performed using JMP software, version 7.0 (SAS Institute, Cary, North Carolina), and advanced statistical analysis was performed using the Statistical Package for Social Sciences, version 11 (SPSS, Chicago, Illinois). p Values <0.05 were considered significant.
Results
The baseline observations of the patient population are summarized in Table 1 . The aortic valve data and dimensions of the ascending aorta are summarized in Table 2 . Of note, 43% of the patients had uni-, bi-, or quadricuspid aortic valves. The mean left ventricular end-diastolic and end-systolic diameter on CMR was 5.6 ± 0.9 cm and 3.9 ± 0.7 cm, respectively. The mean left ventricular ejection fraction was 57 ± 6%. In the study, 16 patients with a non-trileaflet aortic valve had eccentric AR, but only 3 patients with a trileaflet valve had an eccentric jet (p <0.001).
| Variable | Value |
|---|---|
| Age (years) | 48 ± 15 |
| Men | 77 (72%) |
| Height (cm) | 176 ± 11 |
| Weight (kg) | 86 ± 18 |
| Body surface area (kg/cm 2 ) | 2.0 ± 0.3 |
| Systolic blood pressure (mm Hg) | 126 ± 18 |
| Diastolic blood pressure (mm Hg) | 73 ± 11 |
| Heart rate (beats/min) | 72 ± 17 |
| Hypertension | 66 (62%) |
| Diabetes mellitus | 9 (8%) |
| Coronary artery disease | 12 (11%) |
| Peripheral artery disease | 3 (3%) |
| Hyperlipidemia | 33 (31%) |
| Diuretics | 18 (17%) |
| Angiotensin-converting enzyme inhibitor/angiotensin 2 receptor blocker | 41 (38%) |
| Calcium channel blocker | 20 (19%) |
| β Blocker | 53 (50%) |
| Variable | Value |
|---|---|
| Aortic valve morphology | |
| Unicuspid | 3 (3%) |
| Bicuspid | 41 (39%) |
| Tricuspid (normal valve) | 61 (57%) |
| Quadricuspid | 1 (1%) |
| Aortic stenosis (>3 cm/s) | 5 (5%) |
| Aortic regurgitation severity (transthoracic echocardiography) | |
| Vena contracta (mm) | 2.3 (0–5.2) |
| Regurgitation/left ventricular outflow tract width ratio (cm) | 0.12 (0–0.42) |
| 0 | 46 (43%) |
| 1+ | 18 (17%) |
| 2+ | 17 (16%) |
| 3+ | 13 (12%) |
| 4+ | 13 (12%) |
| Direction of aortic regurgitation jet | |
| Central | 42 (41%) |
| Eccentric | 19 (18%) |
| Ascending aorta dimensions on cardiac magnetic resonance imaging (cm) | |
| Sinotubular junction | 3.8 (3.2–4.2) |
| Mid-ascending aorta | 3.9 (3.4–4.5) |
| Distal ascending aorta | 3.0 (3.0–3.8) |
The mean CMR-RF measurements were significantly greater at the sinotubular junction than at the distal ascending aorta (13 ± 13.3% vs 9.4 ± 12.6%, p <0.001). The differences in RF between the levels were most prominent in the patients with no AR and mild to moderate AR. The RF measurement in patients with severe (grade IV+) AR was similar, irrespective of the site of measurement in the ascending aorta (p = 0.17; Table 3 ). An overlap in the RF values was found for each AR grade. Similarly, the RV measurements were significantly greater at the sinotubular junction than at the distal ascending aorta (15.9 ± 21.5 vs 10.5 ± 17.4 ml, p <0.001; Table 4 ).
| Final Echocardiographic Grade | RF (%) | p Value ⁎ | ||
|---|---|---|---|---|
| Sinotubular Junction | Mid-Ascending Aorta | Distal Ascending Aorta | ||
| 0+ | 4.5 ± 3.9 | 4.0 ± 3.7 | 2.5 ± 2.8 | <0.001 |
| I+ | 6.6 ± 2.5 | 5.1 ± 2.9 | 3.2 ± 2.8 | 0.001 |
| II+ | 15.2 ± 9.9 | 11.6 ± 10.1 | 7.6 ± 6.9 | <0.001 |
| III+ | 25.1 ± 12 | 23.8 ± 11 | 19.7 ± 11.8 | 0.001 |
| IV+ | 36.9 ± 10 | 36 ± 11.9 | 34.3 ± 11.2 | 0.17 |
⁎ p Value for difference between sinotubular junction and distal ascending aorta RF (Wilcoxon signed rank test).
| Final Echocardiography Grade | RV (ml/s) | p Value ⁎ | ||
|---|---|---|---|---|
| Sinotubular Junction | Mid-Ascending Aorta | Distal Ascending Aorta | ||
| 0+ | 4.0 ± 3.3 | 3.4 ± 2.9 | 2.0 ± 2.0 | <0.001 |
| I+ | 6.3 ± 3.1 | 4.3 ± 2.4 | 2.6 ± 1.7 | <0.001 |
| II+ | 15.4 ± 11.8 | 11.1 ± 11 | 7.2 ± 7.3 | <0.001 |
| III+ | 32.3 ± 24.3 | 28.6 ± 20.9 | 21.7 ± 16.7 | <0.001 |
| IV+ | 55.6 ± 23.7 | 50.9 ± 25.2 | 44.9 ± 22.3 | 0.05 |
⁎ p Value for difference between sinotubular junction and distal ascending aorta RV (Wilcoxon signed rank test).
The correlations between RF and RV by phase-contrast flow measurements at each imaging plane on CMR and quantitative echocardiographic measures (vena contracta width and jet width/left ventricular outflow tract width ratio) are listed in Table 5 . Similarly, the RF and RV by CMR at each imaging plane were compared to a composite qualitative grade determined using TTE ( Figure 2 ). In a subgroup of 18 patients with grade ≥III+ AR, the RF and RV measurements on TTE (51 ± 16 ml and 49 ± 10%, respectively) were greater than those on CMR at the mid-ascending level (42 ± 9 ml and 32 ± 10%, respectively). In this subgroup, the correlations between the TTE-RV and CMR-RV measured at the sinotubular junction and mid-ascending and distal ascending aorta were modest (0.50, 0.49, and 0.45, respectively; all p <0.01). Similarly, the correlation between TTE-RF and CMR-RF measured at the sinotubular junction and mid-ascending and distal ascending aorta was as follows: 0.49, 0.51, and 0.42, respectively (all p <0.01).
| Variable | R 2 | p Value |
|---|---|---|
| Sinotubular junction | ||
| Regurgitant volume by cardiac magnetic resonance | ||
| Vena contracta by transthoracic echocardiography | 0.52 | <0.001 |
| Aortic regurgitation/left ventricular outflow tract width ratio by transthoracic echocardiography | 0.52 | <0.001 |
| Regurgitant fraction by cardiac magnetic resonance | ||
| Vena contracta by transthoracic echocardiography | 0.59 | <0.001 |
| Aortic regurgitation/left ventricular outflow tract width ratio by transthoracic echocardiography | 0.57 | <0.001 |
| Mid-ascending aorta | ||
| Regurgitant volume by cardiac magnetic resonance | ||
| Vena contracta by transthoracic echocardiography | 0.51 | <0.001 |
| Aortic regurgitation/left ventricular outflow tract width ratio by transthoracic echocardiography | 0.51 | <0.001 |
| Regurgitant fraction by cardiac magnetic resonance | ||
| Vena contracta by transthoracic echocardiography | 0.57 | <0.001 |
| Aortic regurgitation/left ventricular outflow tract width ratio by transthoracic echocardiography | 0.55 | <0.001 |
| Distal descending aorta | ||
| Regurgitant volume by cardiac magnetic resonance | ||
| Vena contracta by transthoracic echocardiography | 0.54 | <0.001 |
| Aortic regurgitation/left ventricular outflow tract width ratio by transthoracic echocardiography | 0.54 | <0.001 |
| Regurgitant fraction by cardiac magnetic resonance | ||
| Vena contracta by transthoracic echocardiography | 0.58 | <0.001 |
| Aortic regurgitation/left ventricular outflow tract width ratio by transthoracic echocardiography | 0.57 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


