Advancing age is associated with downregulation of fibrinolysis in normal subjects. This is reflected by high concentrations of plasminogen activator inhibitor-1 (PAI-1) in the blood, which has been implicated in the increasing cardiovascular morbidity and mortality with age. We sought to delineate the relation of PAI-1 to several factors, including age, gender, and ethnicity in patients with type 2 diabetes mellitus (DM) and stable coronary artery disease enrolled in the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial. A total of 2,321 patients with DM and stable coronary artery disease in the BARI 2D trial were grouped by age (<50, 50 to 59, 60 to 69, and ≥70 years). Tissue-type plasminogen activator antigen, PAI-1 antigen and activity, fibrinogen, and D-dimer were quantified at baseline. The PAI-1 antigen (p <0.001) and its activity (p <0.001) and their ratios to tissue-type plasminogen activator (p <0.001) were all paradoxically lower with advancing age. In contrast, D-dimer (p <0.0001) was elevated. The fibrinogen level was greatest in the oldest age group (p = 0.01). The level of tissue-type plasminogen activator antigen did not vary with age. These age-related differences were observed primarily in men and non-Hispanic white and Asian/other participants. In conclusion, PAI-1 is inversely related to age in patients with DM and stable coronary artery disease and is associated with elevation of D-dimer, reflecting augmented fibrinolysis. The unexpected profibrinolytic state seen with advancing age and DM might reflect a protective phenomenon resulting from enhanced survival of some older patients with DM that endowed the older patients with longevity sufficient to enable them to participate in the BARI 2D trial. Targeting the factors that led to the downregulation of PAI-1 in older patients with type 2 DM might offer an attractive strategy for reducing cardiovascular risk.
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial enrolled patients with type 2 diabetes mellitus (DM) and stable coronary artery disease (CAD). It was designed to determine (1) the efficacy of initial elective coronary revascularization combined with aggressive medical therapy compared to initial, aggressive medical therapy alone with deferred revascularization as needed, and (2) the efficacy of a strategy of providing more insulin (endogenous or exogenous) compared with a strategy of increasing sensitivity to insulin (reducing insulin resistance) in the management of hyperglycemia with a target hemoglobin A1c level of <7.0% for each strategy. In the present study, we sought to delineate the relation of plasminogen activator inhibitor type 1 (PAI-1) to several factors, including age, gender, and ethnicity in patients with DM and stable CAD enrolled in the BARI 2D trial.
Methods
The BARI 2D study was designed to identify the optimal long-term treatment of patients with type 2 DM and documented stable CAD, coupled with uniform glycemic control and intensive risk factor modification. Patients were eligible for enrollment in BARI 2D if they had type 2 DM and angiographically documented CAD in at least one artery for which revascularization was not imminently required for the control of symptoms. The design of the BARI 2D trial has been previously published in detail. The institutional review boards at each participating institution approved the study. Each study participant provided written, informed consent before enrollment.
Between January 1, 2001 and March 31, 2005, 2,321 patients with type 2 DM were enrolled in 49 medical centers. In a 2 × 2 factorial design, the patients were randomized to facilitate testing of 2 hypotheses. The first randomization addressed the hypothesis that coronary revascularization added to aggressive medical therapy would be superior to aggressive medical therapy alone for the treatment of patients with DM and chronic CAD. The second randomization addressed the hypothesis that insulin sensitization would be superior to insulin provision in patients in whom a targeted hemoglobin A1c of <7% was reached. The exclusion criteria included coronary revascularization within 12 months, class III or IV heart failure, renal insufficiency (creatinine >2.0), uncontrolled DM, severe peripheral arterial occlusive disease, liver disease, alcohol abuse, and corticosteroid therapy. The primary end point was the 5-year mortality. A major secondary combined end point was death, myocardial infarction, and stroke. All patients entered into the BARI 2D trial were identified after clinically indicated noninvasive screening and coronary angiography.
At recruitment, fasting blood samples were collected without vacuum into 3.2% sodium citrate solution from an antecubital vein with a 2-syringe technique. Within 15 minutes of collection, the plasma was separated by centrifugation at 3,000 g at 4°C for 10 minutes to remove all platelets, thus eliminating a source of contamination of the samples with PAI-1 liberated from platelets artifactually in vitro. The plasma samples were then maintained at −70°C until assay. The tissue-type plasminogen activator (t-PA) antigen and PAI-1 antigen levels were determined with commercially available enzyme-linked immunoassay kits (Trinity Biochech PLC, Bray, Wicklow, Ireland). PAI-1 activity was assessed using a modified chromogenic substrate enzymatic assay developed by Chmielewska and Wiman as previously described. Fibrinogen was measured by the Claus method. D-dimer was measured immunoturbidimetrically with STA-Liatest D-Dimer reagents (Diagnostica Stago, Parsippany, New Jersey) on a STA Compact (Roche Professional Diagnostics, Basle, Switzerland).
The age of the participants at baseline was stratified into 4 categories, and the baseline demographic, clinical, and fibrinolysis system measurements were determined for each. Differences between the age groups were compared with the Pearson chi-square test for categorical variables and either the Kruskal-Wallis or F test for continuous variables. The Jonckheere-Terpstra test was used to detect ordering of the differences in the fibrinolysis system measurements observed among the incremental age groups. Spearman correlations were used to assess the relations between the fibrinolytic system measurements. Linear regression analysis was used to model the relation between the fibrinolytic system analytes and age. In the models of PAI-1 and D-dimer, the dependent variable (fibrinolysis measurement) was transformed to the natural log to normalize the distribution. The independent variable, age, was divided into 10-year continuous increments. Multivariate linear models were adjusted by baseline variables when differences among the age groups were observed. These variables included gender, race, body mass index, history of myocardial infarction, history of stroke, history of hypertension, previous percutaneous coronary intervention, previous coronary artery bypass grafting, triglycerides, hemoglobin A1c, high-density lipoprotein, history of cigarette smoking, DM duration, and baseline use of insulin, sulfonylurea, thiazolidinediones, and biguanide. The effect of gender and race on the age relation with the fibrinolytic system measures was assessed by adding appropriate interaction terms to the linear models. A p value of ≤0.05 was used to determine statistical significance.
Results
The demographic and clinical data for the 2,321 enrolled patients with DM stratified into 4 age categories (<50; 50–59; 60–69, and ≥70 years) are listed in Table 1 . Nearly 1/3 of the cohort consisted of women, and female gender was significantly more prevalent in the oldest age group. Two-thirds of the cohort were white, and this ethnicity was more common in the older patient subsets. The black and Hispanic participants tended to be younger.
| Variable | Total (n = 2321) | Age Group (years) | p Value | |||
|---|---|---|---|---|---|---|
| <50 (n = 195) | 50–59 (n = 727) | 60–69 (n = 897) | ≥70 (n = 502) | |||
| Women | 29.6% | 31.3% | 28.7% | 27.0% | 34.7% | 0.02 |
| Ethnicity | <0.001 | |||||
| Black non-Hispanic | 16.9% | 25.1% | 18.7% | 14.6% | 15.3% | |
| Hispanic | 12.7% | 18.5% | 15.3% | 11.0% | 9.6% | |
| White non-Hispanic | 65.6% | 49.2% | 60.7% | 70.1% | 70.9% | |
| Asian/other non-Hispanic | 4.8% | 7.2% | 5.4% | 4.2% | 4.2% | |
| Exercise regularly | 25.7 | 23.1 | 22.0 | 26.9 | 29.9 | 0.01 |
| Body mass index (kg/m 2 ) | <0.001 | |||||
| Mean | 31.7 | 33.3 | 32.4 | 31.4 | 30.7 | |
| Median | 31 | 32 | 32 | 31 | 30 | |
| Fasting insulin (μIU/ml) | 0.22 | |||||
| Mean | 14.1 | 14.1 | 15.0 | 13.6 | 13.9 | |
| Median | 10 | 10 | 10 | 10 | 9 | |
| Hemoglobin A1c (%) | <0.001 | |||||
| Mean | 7.66 | 8.18 | 7.97 | 7.60 | 7.13 | |
| Median | 7 | 8 | 8 | 7 | 7 | |
| Diabetes mellitus duration (years) | <0.001 | |||||
| Mean | 10.4 | 6.9 | 8.9 | 11.2 | 12.7 | |
| Median | 9 | 5 | 7 | 10 | 10 | |
| Lipid values (mg/dl) | ||||||
| Total cholesterol | 170 ± 41 | 181 ± 49 | 175 ± 42 | 167 ± 41 | 161.7 ± 34.3 | <0.001 |
| Low-density lipoprotein | 96 ± 33 | 104 ± 37 | 100 ± 34 | 94.5 ± 33.5 | 91.6 ± 29.3 | <0.001 |
| High-density lipoprotein | 38 ± 10 | 36 ± 9 | 38 ± 10 | 38.6 ± 10.6 | 39.0 ± 10.6 | <0.001 |
| Triglyceride | <0.001 | |||||
| Mean | 181 | 216.4 | 194.5 | 173.7 | 158.4 | |
| Median | 149 | 179 | 160 | 144 | 139 | |
| Smoker (%) | 66.8% | 68.7% | 70.0% | 66.9% | 61.2% | 0.01 |
| Insulin use (%) | 27.8% | 23.1% | 30.0% | 28.2% | 25.9% | 0.18 |
| Thiazolidinedione use (%) | 18.8% | 18.5% | 19.8% | 20.1% | 14.9% | 0.09 |
| Sulfonylurea use (%) | 53.6% | 48.2% | 52.1% | 55.2% | 55.0% | 0.24 |
| Biguanide use (%) | 54.1% | 57.4% | 57.4% | 54.4% | 47.2% | 0.003 |
| Treated hypertension (%) | 82.4% | 74.7% | 80.2% | 85.0% | 4.0% | 0.002 |
| History of myocardial infarction (%) | 31.9% | 37.8% | 34.1% | 29.8% | 30.2% | 0.07 |
| Previous stroke, TIA (%) | 9.8% | 3.6% | 7.2% | 11.7% | 12.7% | <0.001 |
| Previous CABG (%) | 6.4% | 2.6% | 6.1% | 6.8% | 7.8% | 0.08 |
| Previous PCI | 19.6% | 20.5% | 19.5% | 19.3% | 19.9% | 0.98 |
The older BARI 2D patients had a more favorable cardiovascular risk profile compared with that in their younger counterparts. They had a significantly lower body mass index, lower total and low-density lipoprotein cholesterol, and higher high-density lipoprotein cholesterol. The older patients had significantly lower hemoglobin A1c values. Despite the cultural changes that have occurred during the past several decades, the younger BARI 2D participants had experienced significantly greater exposure to nicotine. Although the older patients tended to have a lower prevalence of myocardial infarction as judged from their history, they tended to have had more frequent exposure to coronary bypass surgery. Nearly equal percentages of older compared with younger patients had undergone revascularization with percutaneous coronary intervention. In contrast to the trend for myocardial infarction, the older participants had experienced more frequent cerebrovascular events (transient ischemic attack/cardiovascular accident), which might be explained in part by the greater prevalence of hypertension.
The fasting insulin concentrations were similar across the age groups. Similarly, the use of insulin, thiazolidinediones, and sulfonylurea did not vary by age. In contrast, the use of a biguanide was more common in the younger patients.
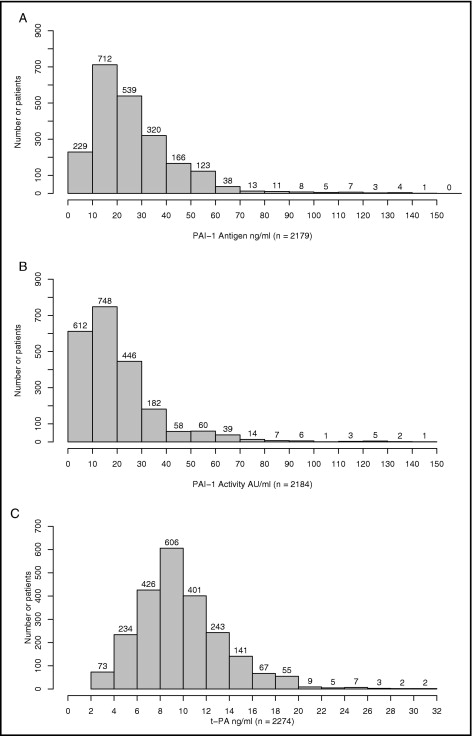
The total antigen content and activity of PAI-1 varied considerably across the entire cohort. The PAI-1 values ranged from undetectable to as high as 142 AU/ml for activity and 150 ng/ml for the total antigen measurement. A distinct rightward skew of the data was noted for both measurements ( Figure 1 ). In contrast, the distribution of t-PA antigen was normal ( Figure 1 ). Both PAI-1 measures correlated inversely with age ( Table 2 ). A stepwise decrement in these measurements was apparent for age <50 years compared to each subsequent decade ( Figure 2 ). In contrast, the t-PA antigen content did not vary with age. Thus, the ratio of PAI-I to t-PA antigen was significantly lower in patients of advanced age.
| Variable | Age Group (years) | p Value ⁎ | |||
|---|---|---|---|---|---|
| <50 (n = 195) | 50–59 (n = 727) | 60–69 (n = 897) | ≥70 (n = 502) | ||
| Plasminogen activator inhibitor-1 antigen (ng/ml) | 33.1 [27] | 29.5 [25] | 25.7 [22] | 24.6 [20] | <0.001 |
| Plasminogen activator inhibitor-1 activity (AU/ml) | 26.1 [21] | 23.6 [19] | 19.2 [15] | 16.9 [13] | <0.001 |
| Tissue-type plasminogen activator (ng/ml) | 10.4 [10] | 10.1 [10] | 10.0 [10] | 10.2 [10] | 0.46 |
| Plasminogen activator inhibitor-1/tissue-type plasminogen activator ratio | 3.5 [3] | 3.0 [3] | 2.7 [2] | 2.5 [2] | <0.001 |
| Fibrinogen (mg/dl) | 362.7 [344] | 367.1 [360] | 359.9 [350] | 377.5 [367] | 0.12 |
| Fibrin D-dimer (μg/ml) | 0.4 [0] | 0.4 [0] | 0.5 [0] | 0.8 [0] | <0.001 |
⁎ For ordered differences; Jonckheere-Terpstra test was used to determine whether differences in analytes among age groups were ordered.
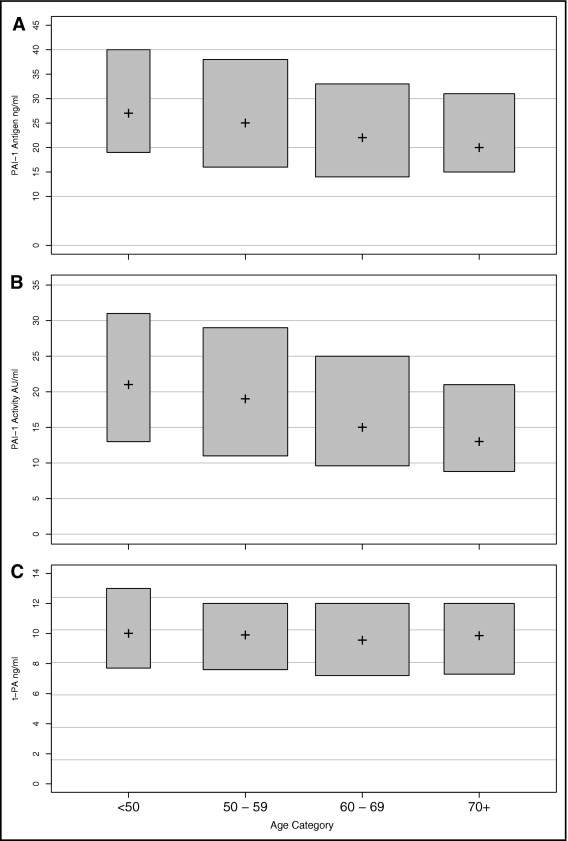
The concentrations of fibrinogen varied within a sixfold range, from 128 to 784 mg/dl, across the cohort ( Figure 3 ). The distribution of fibrinogen, however, similar to that of t-PA, was gaussian. The fibrinogen level was greatest in the oldest age group (p <0.01) compared with that in the younger age quartiles. The age-related trend of fibrinogen values, however, did not reach statistical significance (p = 0.12; Table 2 ). The distribution of D-dimer was skewed rightward, with the vast majority of participants having very low values. D-dimer increased significantly with older age ( Table 2 ).
On univariate analysis, PAI-1 antigen, PAI-1 activity, and the PAI-1 antigen/t-PA ratio were all significantly and inversely associated with age ( Table 3 ). After controlling for baseline differences among the age groups, age remained significantly associated with each of these variables. In contrast, t-PA was significantly and directly associated with increasing age. The concentrations of triglycerides correlated directly with PAI-1 activity (r s = 0.32, p <0.001), PAI-1 antigen content (r s = 0.31, p <0.001), and t-PA (r s = 0.26, p <0.001).
| Variable ⁎ | Univariate | Multivariate † | ||||||
|---|---|---|---|---|---|---|---|---|
| n | Change/10-yr Age Increment | p Value | R 2 | n | Change/10-yr Age Increment | p Value | R 2 | |
| Log (PAI-1 antigen) | 2,179 | −0.09 | <0.001 | 0.015 | 2,083 | −0.04 | 0.02 | 0.21 |
| Log (PAI-1 activity) | 2,184 | −0.15 | <0.001 | 0.034 | 2,088 | −0.09 | <0.001 | 0.24 |
| t-PA (ng/ml) | 2,274 | −0.06 | 0.55 | 0.00 | 2,179 | 0.26 | 0.006 | 0.21 |
| Log (PAI-1 antigen/t-PA ratio) | 2,171 | −0.09 | <0.001 | 0.021 | 2,075 | −0.06 | <0.001 | 0.10 |
| Log (D-dimer) | 2,260 | 0.31 | <0.001 | 0.086 | 2,169 | 0.31 | <0.001 | 0.15 |
⁎ Each line represents a separate model of the fibrinolytic system measurement and age.
† Multivariate model included gender, race, BMI, history of MI, history of hypertension, history of stroke, previous PCI, previous CABG, DM duration, hemoglobin A1c, triglycerides, HDL, history of cigarette smoking, and baseline use of insulin, sulfonylurea, thiazolidinedione, and biguanide.
An additional assessment was performed to determine whether the association of age with these variables differed as a function of gender. For each 10-year increment in age for men, log (PAI-1 antigen) was lower by 0.05 (p <0.006). In women, it was lower by 0.01 (p = NS). Log (PAI-1 activity) was lower by 0.05 in women (p = 0.07) and 0.10 for men (p <0.001) for every 10-year increase in age. The observed gender differences in the PAI-1 antigen and PAI-1 activity relations with age were not statistically significant (p <0.16). No age and gender interaction (p <0.49) was found for the PAI-1 antigen/t-PA ratio or for t-PA (p <0.23).
The age association with the fibrinolytic system measurements was also evaluated with respect to race/ethnicity ( Table 4 ). The differences in the age association with PAI-1 among the racial/ethnic groups was not statistically significant (p = 0.16). In non-Hispanic blacks, PAI-1 did not vary with age. For the other non-Hispanic groups (whites and Asians/others), it did vary significantly with age. The age–PAI-1 relation was similar in Hispanic and white participants; however, it did not reach statistical significance in Hispanics. Similar relations with respect to the PAI-1 antigen/t-PA ratio and PAI-1 activity were observed.



