The impact of lesion calcium on long-term outcomes after drug-eluting stent implantation has not been adequately addressed. In 10,595 patients (16,803 lesions) who were exclusively treated with sirolimus-eluting stents in the j-Cypher registry, 5-year outcomes were compared between patients with ≥1 lesion with moderate or severe calcification (the calcium group) and those with noncalcified lesions only (the noncalcium group). Analyses were stratified by hemodialysis (HD) status (non-HD stratum [calcium n = 3,191, noncalcium n = 6,824] and HD stratum [calcium n = 415, noncalcium n = 165]). Adjusted risk in the calcium group for death and target lesion revascularization was significant in the non-HD stratum (hazard ratio [HR] 1.34, 95% confidence interval [CI] 1.18 to 1.52, p <0.0001, and HR 1.2, 95% CI 1.07 to 1.36, p = 0.003) and the HD stratum (HR 1.4, 95% CI 1.06 to 1.86, p = 0.02, and HR 2.25, 95% CI 1.51 to 3.36, p <0.0001). Risk for definite stent thrombosis tended to be higher in the calcium group in the HD stratum (HR 5.05, 95% CI 0.66 to 38.9, p = 0.12) but not in then non-HD stratum (HR 1.16, 95% CI 0.81 to 1.67, p = 0.41). The use of rotational atherectomy in patients with severe calcification did not have a significant impact on the cumulative incidence of target lesion revascularization in the non-HD stratum (17.7% [n = 268] with vs 18.2% [n = 588] without rotational atherectomy, p = 0.68) and the HD stratum (54.7% [n = 115] with vs 51.9% [n = 118] without rotational atherectomy, p = 0.19). In conclusion, regardless of HD status, patients with calcified lesions have increased long-term risk for death and target lesion revascularization after sirolimus-eluting stent implantation.
Drug-eluting stents are often used to treat complex lesions. Stenting in complex calcified lesions is frequently associated with inadequate stent expansion, incomplete stent apposition, and stent fracture, for which rotational atherectomy (RA) is often required. Although stent implantation procedures are more demanding in calcified lesions, the impact of lesion calcium on clinical outcomes after drug-eluting stent implantation has not been adequately evaluated. The impact of lesion calcium on clinical outcomes after drug-eluting stent implantation might be different according to the presence or absence of hemodialysis (HD). However, previous studies included relatively small numbers of patients with calcified lesions and very small numbers of patients on HD. Also, the effect of RA on long-term clinical outcomes in patients with calcified lesions has not been thoroughly evaluated. Therefore, we compared long-term clinical outcomes after sirolimus-eluting stent (SES) implantation between patients with and those without calcified coronary lesions stratified by the presence or absence of HD on the basis of a large-scale Japanese database in real-world clinical practice.
Methods
The study design and patient enrollment for the j-Cypher registry have been previously described in detail. In brief, the j-Cypher registry is a physician-initiated prospective multicenter observational study of consecutive patients who underwent SES implantation in Japan. The relevant review boards at all 37 participating centers approved the study protocol ( Supplementary Appendix A ). Written informed consent was obtained from all patients. Collection of 5-year follow-up information was conducted mainly through review of hospital charts by the site investigators or experienced research coordinators in the independent research organization (Research Institute for Production Development, Kyoto, Japan; Supplementary Appendix B ).
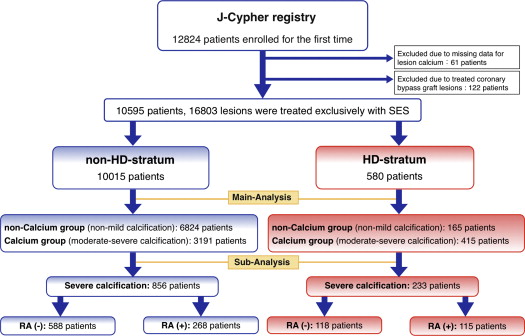
The present post hoc subanalysis of the j-Cypher registry was intended to compare 5-year clinical outcomes between patients with and those without calcified coronary lesions stratified by the presence or absence of HD. Among 12,824 patients enrolled in the registry from August 2004 to November 2006, 10,778 patients were treated exclusively with SES. After excluding 61 patients with missing data for lesion calcium and 122 patients with treated lesions in the saphenous vein or arterial grafts, the study population for the present analysis consisted of 10,595 patients (580 patients on HD and 10,015 patients not on HD). Patients with ≥1 lesion with moderate or severe calcification were classified as the calcium group (HD stratum 415 patients, non-HD stratum 3,191 patients), and patients who only had lesions with no or mild calcification were classified as the noncalcium group (HD stratum 165 patients, non-HD stratum 6,824 patients). The influence of RA on clinical outcomes was assessed in a subgroup of 1,089 patients with severe calcification ( Figure 1 ).
Coronary calcification was defined as obvious density within the arterial wall and at lesion sites that was readily apparent as an x-ray-absorbing mass. The severity of calcification was classified as absent, mild, moderate (density noted only during the cardiac cycle before contrast injection), or severe (density noted without cardiac motion before contrast injection and generally involving both sides of the arterial wall). Angiographic analyses including evaluation of calcification were not conducted in a central core laboratory but were reported by the site investigators.
The major outcome measures for the present analysis were all-cause death, target lesion revascularization, and definite stent thrombosis. Target lesion revascularization and stent thrombosis were assessed on a per patient basis. In the calcium group, target lesion revascularization and stent thrombosis events that occurred in noncalcified lesions were also adjudicated as the end point events. Target lesion revascularization was further subdivided into early (within the first year after SES implantation) and late (beyond 1 year) target lesion revascularization according to our previous reports.
Death was regarded as cardiac in origin unless obvious noncardiac causes could be identified. Stent thrombosis was defined according to the Academic Research Consortium definition. We defined target lesion revascularization as repeated intervention (percutaneous coronary intervention or coronary artery bypass grafting surgery) for significant lesions within the stented segment or within 5 mm of the stent borders. Death, myocardial infarction, and stent thrombosis events were adjudicated using the original source documents by a clinical event committee ( Supplementary Appendix C ). Adjudication of target lesion revascularization events was left to the judgment by the site investigators.
Categorical variables are presented as counts and/or percentages and were compared using chi-square tests. All continuous variables are expressed as mean ± SD unless otherwise indicated. Mean values between the 2 groups were compared using Student’s t tests. Cumulative incidences of events were estimated using the Kaplan-Meier method, and curves of the 2 groups were compared using the log-rank test. A landmark analysis was conducted to evaluate the cumulative incidence of late target lesion revascularization occurring beyond 1 year. Eligible patients for the landmark analysis were those patients who completed the 1-year follow-up without target lesion revascularization.
Adjusted risk in the calcium group relative to the noncalcium group for major outcome measures was evaluated by using a multivariate Cox proportional-hazards model. Consistent with our previous reports, we selected the 23 independent variables listed in Tables 1 and 2 . The continuous variables were dichotomized by clinically meaningful reference values or median values. We first selected variables with p values <0.05 in the univariate Cox models, and we confirmed that proportional-hazards assumptions were acceptable on the plots of log (time) versus log [log (survival)] stratified by the variables. We then included them simultaneously in the multivariate models and obtained the adjusted hazard ratios (HRs) and their 95% confidence intervals (CIs). Patients with missing values for any selected variable were excluded from the multivariate analysis. A physician (KN) and an independent statistician (IM) analyzed all data using SPSS version 20J for Windows (SPSS Japan Inc., Tokyo, Japan). All reported p values were 2 sided, and p values <0.05 were regarded as statistically significant.
| Variable | Non-HD | HD | ||||
|---|---|---|---|---|---|---|
| Noncalcium (n = 6,824) | Calcium (n = 3,191) | p Value | Noncalcium (n = 165) | Calcium (n = 415) | p Value | |
| Age (yrs) | 68 ± 10 | 70 ± 10 | <0.0001 | 65 ± 11 | 66 ± 10 | 0.44 |
| Age ≥80 yrs ∗ | 748 (11%) | 543 (17%) | <0.0001 | 13 (7.9%) | 39 (9.4%) | 0.56 |
| Men ∗ | 5,268 (77%) | 2,279 (71%) | <0.0001 | 121 (73%) | 316 (76%) | 0.48 |
| Body mass index (kg/m 2 ) | 24.2 ± 3.2 | 23.8 ± 3.5 | <0.0001 | 22.4 ± 3.5 | 22.0 ± 3.5 | 0.23 |
| Body mass index <25 kg/m 2 ∗ | 4,292 (63%) | 2,119 (66%) | 0.001 | 127 (77%) | 341 (82%) | 0.15 |
| Hypertension ∗ | 4,960 (73%) | 2,469 (77%) | <0.0001 | 138 (84%) | 363 (88%) | 0.23 |
| Diabetes mellitus ∗ | 2,613 (38%) | 1,357 (43%) | <0.0001 | 106 (64%) | 241 (58%) | 0.17 |
| Insulin treated | 480 (7%) | 330 (10%) | <0.0001 | 55 (33%) | 107 (26%) | 0.07 |
| Current smoking ∗ | 1,417 (21%) | 589 (19%) | 0.007 | 29 (18%) | 62 (15%) | 0.43 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 62.6 ± 19.2 | 59.4 ± 20.5 | <0.0001 | 6.3 ± 5.3 | 6.1 ± 6.0 | 0.64 |
| Estimated glomerular filtration rate <30 ml/min/1.73 m 2 without HD ∗ | 291 (4.3%) | 220 (6.9%) | <0.0001 | |||
| HD duration (yrs) | 4.3 ± 4.9 | 6.9 ± 6.0 | <0.0001 | |||
| Acute coronary syndromes ∗ | 1,459 (21%) | 696 (21%) | 0.63 | 35 (21%) | 84 (20%) | 0.79 |
| ST-segment elevation myocardial infarction | 528 (7.7%) | 181 (5.7%) | <0.0001 | 7 (4.2%) | 12 (2.9%) | 0.41 |
| Non-ST-segment elevation myocardial infarction | 139 (2.0%) | 70 (2.2%) | 0.61 | 0 (0%) | 6 (1.4%) | 0.12 |
| Unstable angina | 792 (12%) | 445 (14%) | 0.001 | 28 (17%) | 66 (16%) | 0.75 |
| Previous myocardial infarction ∗ | 1,924 (28%) | 898 (28%) | 0.96 | 34 (21%) | 95 (23%) | 0.55 |
| Previous stroke ∗ | 584 (8.6%) | 330 (10%) | 0.004 | 14 (8.5%) | 60 (15%) | 0.052 |
| Peripheral vascular disease ∗ | 683 (10%) | 410 (13%) | <0.0001 | 37 (22%) | 107 (26%) | 0.40 |
| Previous heart failure ∗ | 727 (11%) | 512 (16%) | <0.0001 | 49 (30%) | 133 (32%) | 0.58 |
| Previous percutaneous coronary intervention ∗ | 3,387 (50%) | 1,394 (44%) | <0.0001 | 81 (49%) | 208 (50%) | 0.82 |
| Previous coronary artery bypass grafting ∗ | 313 (4.6%) | 286 (9%) | <0.0001 | 9 (5.5%) | 54 (13%) | 0.008 |
| Multivessel coronary disease | 2,933 (43%) | 1,961 (62%) | <0.0001 | 72 (44%) | 268 (65%) | <0.0001 |
| Ejection fraction (%) | 59 ± 13 | 57 ± 14 | <0.0001 | 55 ± 14 | 53 ± 14 | 0.12 |
| Number of vessels treated | 1.2 ± 0.4 | 1.3 ± 0.6 | <0.0001 | 1.1 ± 0.4 | 1.2 ± 0.5 | 0.004 |
| Treated multivessel coronary stenting | 1,088 (16%) | 857 (27%) | <0.0001 | 18 (11%) | 90 (22%) | 0.003 |
| Number of coronary lesions treated | 1.3 ± 0.6 | 1.5 ± 0.8 | <0.0001 | 1.3 ± 0.6 | 1.4 ± 0.7 | 0.03 |
| Total stents per patient | 1.7 ± 1.0 | 2.1 ± 1.3 | <0.0001 | 1.7 ± 1.1 | 1.9 ± 1.2 | 0.01 |
| Total length of stents per patient | 36.7 ± 24.0 | 46.7 ± 31.2 | <0.0001 | 36.8 ± 28.6 | 42.5 ± 28.7 | 0.03 |
| Total length of stents >28 mm ∗ | 3,577 (52%) | 2,154 (68%) | <0.0001 | 78 (48%) | 259 (62%) | 0.001 |
| European System for Cardiac Operative Risk Evaluation score | 4.0 ± 2.8 | 4.9 ± 3.1 | <0.0001 | 6.2 ± 2.9 | 6.6 ± 3.4 | 0.10 |
∗ Variables used for multivariate analyses evaluating adjusted outcomes.
| Variable | Non-HD | HD | ||||
|---|---|---|---|---|---|---|
| Noncalcium (n = 11,272) | Calcium (n = 4,631) | p Value | Noncalcium (n = 285) | Calcium (n = 615) | p Value | |
| Coronary lesion location | <0.0001 | 0.24 | ||||
| Left anterior descending ∗ | 4,431 (39%) | 2,233 (48%) | 91 (32%) | 224 (36%) | ||
| Left circumflex | 2,697 (24%) | 781 (17%) | 63 (22%) | 111 (18%) | ||
| Right | 3,831 (34%) | 1,406 (30%) | 119 (42%) | 243 (40%) | ||
| Left main ∗ | 313 (2.8%) | 211 (4.6%) | 12 (4.2%) | 37 (6%) | ||
| In-stent restenosis ∗ | 1,501 (13%) | 395 (8.5%) | <0.0001 | 40 (14%) | 69 (11%) | 0.23 |
| Chronic total occlusion ∗ | 853 (7.6%) | 551 (12%) | <0.0001 | 21 (7.4%) | 39 (6.3%) | 0.57 |
| Bifurcation lesion | 2,144 (19%) | 979 (21%) | 0.002 | 47 (17%) | 107 (17%) | 0.74 |
| Side branch stenting ∗ | 344 (3.1%) | 194 (4.2%) | <0.0001 | 8 (2.8%) | 30 (4.9%) | 0.15 |
| Reference vessel diameter pre <2.5 mm ∗ | 3,161 (28%) | 1,443 (32%) | <0.0001 | 64 (23%) | 144 (24%) | 0.73 |
| Use of intravascular ultrasound ∗ | 4,839 (43%) | 2,277 (49%) | <0.0001 | 111 (39%) | 282 (46%) | 0.052 |
| Direct stenting | 3,018 (27%) | 710 (15%) | <0.0001 | 62 (22%) | 64 (10%) | <0.0001 |
| Postdilatation | 4,657 (41%) | 2,289 (50%) | <0.0001 | 137 (48%) | 332 (54%) | 0.10 |
| Use of RA | 29 (0.3%) | 491 (11%) | <0.0001 | 4 (1.4%) | 174 (28%) | <0.0001 |
| Maximum inflation pressure (atm) | 17.7 ± 3.3 | 18.4 ± 3.3 | <0.0001 | 18.8 ± 3.2 | 19.4 ± 3.5 | 0.009 |
| Number of stents used per lesion | 1.3 ± 0.6 | 1.4 ± 0.7 | <0.0001 | 1.3 ± 0.6 | 1.4 ± 0.7 | 0.04 |
| Length of stents used per lesion (mm) | 28.2 ± 15.3 | 32.4 ± 18.5 | <0.0001 | 28.4 ± 17.6 | 30.5 ± 18.5 | 0.11 |
| Minimal stent size (mm) | 2.89 ± 0.37 | 2.85 ± 0.35 | <0.0001 | 2.93 ± 0.38 | 2.94 ± 0.38 | 0.67 |
∗ Variables used for multivariate analyses evaluating adjusted outcomes.
Results
In the non-HD stratum, baseline patient, lesion, and procedural characteristics were markedly different between the calcium and noncalcium groups. Patients in the calcium group were older; had lower body mass indexes; more often had co-morbidities such as hypertension, diabetes, renal failure, previous stroke, peripheral vascular disease, previous heart failure, and multivessel coronary artery disease; less often had ST-segment elevation myocardial infarction; and more often were current smokers than patients in the noncalcium group ( Table 1 ). Lesions in the calcium group included more left anterior descending coronary artery lesions and more complex lesions such as chronic total occlusion, bifurcation lesions, long lesions, and small-vessel disease than lesions in the noncalcium group. Lesions in the calcium group were more often treated with adjunctive use of RA, with the use of intravascular ultrasound, with postdilatation at higher maximum inflation pressure, and with longer total stent length than lesions in the noncalcium group ( Table 2 ). In contrast, the baseline characteristics of patients in the HD stratum were similar between the calcium and noncalcium groups, although HD duration was longer and multivessel coronary artery disease was more prevalent in the calcium group ( Table 1 ). Lesion characteristics in the HD stratum were also similar between the calcium and noncalcium groups. The differences in the procedural characteristics between the calcium and noncalcium groups in the HD stratum were generally common to those in the non-HD stratum ( Table 2 ).
In the non-HD stratum, the cumulative incidence of all-cause death was significantly higher in the calcium group than in the noncalcium group ( Table 3 , Figure 2 ). After adjusting confounders, the higher risk in the calcium group relative to the noncalcium group for all-cause death remained significant (HR 1.34, 95% CI 1.18 to 1.52, p <0.0001). The cumulative incidence of target lesion revascularization was significantly higher in the calcium group than in the noncalcium group ( Table 3 , Figure 3 ). After adjusting confounders, the higher risk in the calcium group relative to the noncalcium group for target lesion revascularization remained significant (HR 1.2, 95% CI 1.07 to 1.36, p = 0.003).The cumulative incidence of early target lesion revascularization within the first year was significantly higher in the calcium group than in the noncalcium group, and the cumulative incidence of late target lesion revascularization beyond 1-year was similar between the calcium and noncalcium groups ( Table 3 , Figure 4 ). The cumulative incidence of definite stent thrombosis was similar between the calcium and noncalcium groups ( Table 3 , Figure 5 ). After adjusting confounders, the risk in the calcium group relative to the noncalcium group for definite stent thrombosis remained insignificant (HR 1.16, 95% CI 0.81 to 1.67, p = 0.41).



