Mitral valve prolapse may involve 1 leaflet or 2 leaflets, yet management guidelines do not differentiate posterior leaflet (PML) from bileaflet (BML) prolapse. We hypothesized that patients with BML have a prolonged natural history with more severe atrial and ventricular enlargement but less severe mitral regurgitation (MR) compared to patients with PML. Patients with mitral valve prolapse undergoing mitral repair were identified and preoperative characteristics were recorded. Patients with predominant PML prolapse (n = 304) versus BML prolapse (n = 131) were identified based on preoperative echocardiographic and intraoperative findings. Timing of operation was based on standard guidelines. Despite being equally symptomatic, patients with BML differed significantly from those with PML in being younger (54 vs 60 years, p <0.0001), more likely to be women (51% vs 24%, p <0.0001), and having a larger valve (37 vs 32 mm, p <0.0001). Despite similar cardiac function and dimensions, patients with BML had less severe MR (24% vs 13% with <4+ MR, p = 0.01) and less severe pulmonary hypertension (14% vs 31%, p <0.0001) at time of operation. In conclusion, patients with BML often meet indications for mitral valve repair with similar cardiac enlargement but less MR than patients with PML prolapse. Patients with BML prolapse may benefit from timing mitral repair based more on symptomatic 3+ MR or cardiac enlargement and less on presence of severe MR.
Current American College of Cardiology/American Heart Association management guidelines for mitral valve prolapse (MVP) do not differentiate posterior leaflet (PML) from bileaflet (BML) prolapse. Given the significantly different pathologies between these 2 forms of MVP, the optimal timing and nature of cardiac dysfunction may be different between these 2 groups. Following guidelines for operation that do not account for these disease-specific differences may result in delayed operation and irreversible cardiac dysfunction. The objective of this study was to compare characteristics of patients with BML to those with PML presenting for MV repair. We assessed 2 hypotheses: (1) that BML and PML patient populations have different demographic characteristics and (2) that patients with BML present with more severe atrial and ventricular enlargement but less severe mitral regurgitation (MR) compared to patients with PML prolapse.
Methods
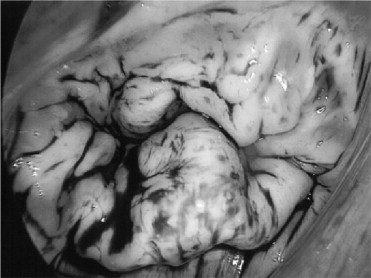
After institutional review board approval, all patients with BML or PML prolapse undergoing MV repair for MVP at Duke University Medical Center by a single surgeon from 1996 through 2009 were identified from a prospectively maintained database. Preoperative characteristics including demographics, symptoms, co-morbidities, echocardiographic data, and cardiac catheterization results were noted. Intraoperative findings including valve structure and characteristics and annular size were recorded. Patients with predominant PML prolapse ( Figure 1 ) versus BML prolapse ( Figure 2 ) were identified based on preoperative echocardiographic and intraoperative findings. Timing of operation was based on American College of Cardiology/American Heart Association guidelines for presence of severe MR or left ventricular ejection fraction <60% based on echocardiogram or left ventriculogram. The remaining patients with less than severe MR and ejection fraction >60% were referred for symptomatic 3+ MR or rapid increase in left ventricular end-systolic diameter to near 4.0 cm on serial echocardiogram at rest. Statistical analysis was performed with StatsDirect Ltd. (Cheshire, United Kingdom). Generalized linear regression, chi-square test, Fisher’s exact test, and Mann–Whitney test were used to compare characteristics between patients with PML and those with BML. Continuous variables were expressed as mean ± SD. Data not distributed normally were presented as median (25th to 75th percentiles). Statistical significance was defined as a probability value <0.05.

Results
Three hundred four patients with PML prolapse and 131 patients with BML prolapse were identified. Preoperative patient characteristics are presented in Table 1 . Patients with PML prolapse were older (60 ± 13 vs 54 ± 13 years, p <0.0001), more often men (75% vs 49%, p <0.0001), and more often nonwhite (12% vs 5%, p = 0.046). Other co-morbidities were similar between the 2 groups aside from a higher rate of cerebrovascular disease in patients with BML. Heart failure symptoms at referral for surgery were similar between groups.
| Variable | Posterior Prolapse | Bileaflet Prolapse | p Value |
|---|---|---|---|
| (n = 304) | (n = 131) | ||
| New York Heart Association class | 0.52 | ||
| I | 22 (7%) | 9 (7%) | |
| II | 104 (34%) | 46 (35%) | |
| III | 127 (42%) | 61 (47%) | |
| IV | 51 (17%) | 15 (11%) | |
| Hypertension | 159 (82%) | 59 (75%) | 0.17 |
| Chronic atrial fibrillation | 34 (11%) | 17 (13%) | 0.59 |
| Current smoker | 76 (28%) | 32 (26%) | 0.63 |
| Renal failure | 2 (1%) | 0 (0%) | 1 |
| Cerebrovascular disease | 14 (5%) | 18 (14%) | 0.0008 |
| Peripheral vascular disease | 4 (1%) | 4 (3%) | 0.25 |
| Lung disease | 21 (7%) | 5 (4%) | 0.21 |
| Diabetes mellitus | 14 (5%) | 4 (3%) | 0.46 |
| Infective endocarditis (active) | 6 (2%) | 3 (2%) | 1 |
| Cancer (in previous 5 years) | 29 (10%) | 12 (9%) | 0.9 |
| Connective tissue disorder | 17 (6%) | 12 (9%) | 0.17 |
| Previous cardiac surgery | 8 (3%) | 6 (5%) | 0.37 |
| Coronary artery disease | 37 (12%) | 9 (7%) | 0.10 |
Patients with BML had less severe pulmonary hypertension compared to patients with PML ( Table 2 ). In addition, patients with BML had less severe MR at presentation ( Table 2 ). Other cardiac dimensions and hemodynamics including left atrial diameter and tricuspid regurgitation were similar between the 2 groups ( Table 2 ). Percentage of patients meeting American College of Cardiology/American Heart Association guidelines at time of mitral repair was the same (98% vs 98%, p = 1). Of 89 patients operated on for less than severe MR, 67 had an ejection fraction <60%, 13 had 3+ MR and symptoms, and 9 were operated on for a rapid increase in left ventricular end-systolic diameter to <4.0 cm. There was no significant difference in duration of heart murmur (20 ± 5 vs 13 ± 5 years, p = 0.07) or duration of symptoms (4 ± 1 vs 6 ± 2 years, p = 0.20) for patients with PML versus those with BML.
| Variable | Posterior Prolapse | Bileaflet Prolapse | p Value |
|---|---|---|---|
| (n = 304) | (n = 131) | ||
| Ejection fraction (%) | 55 ± 10 | 54 ± 8 | 0.16 |
| Right atrial pressure (mm Hg) | 7 ± 4 | 8 ± 8 | 0.68 |
| Left atrial diameter (cm) | 4.8 ± 0.9 | 4.8 ± 0.8 | 0.74 |
| Pulmonary artery systolic pressure (mm Hg) | 40 ± 16 | 33 ± 11 | <0.0001 |
| Left ventricular end-systolic diameter (cm) | 3.6 ± 0.7 | 3.8 ± 0.8 | 0.28 |
| Mitral regurgitation grade (continuous) | 3.9 ± 0.4 | 3.7 ± 0.5 | 0.008 |
| Mitral regurgitation grade <4+ | 54 (18%) | 35 (27%) | 0.03 |
| Mitral regurgitation grade (categorical) | 0.03 | ||
| 1 | 2 (1%) | 1 (1%) | |
| 2 | 3 (1%) | 6 (5%) | |
| 3 | 49 (16%) | 28 (21%) | |
| 4 | 250 (82%) | 96 (73%) | |
| Tricuspid regurgitation grade >2+ | 19 (6%) | 9 (7%) | 0.81 |
| Tricuspid regurgitation grade | 0.79 | ||
| 0 | 215 (74%) | 102 (78%) | |
| 1 | 56 (19%) | 19 (15%) | |
| 2 | 1 (0.3%) | 1 (0.8%) | |
| 3 | 13 (4%) | 6 (5%) | |
| 4 | 6 (2%) | 3 (2%) |
Operative characteristics are presented in Table 3 . Patients with BML had larger annular rings and longer cardiopulmonary bypass and aortic cross-clamp times ( Table 3 ). Twenty-three percent of patients had concomitant procedures performed. Most frequent concurrent procedures were the maze procedure (70 of 435, 16%) and coronary artery bypass grafting (25 of 435, 6%). Most procedures (359 of 435, 83%) were performed as a right minithoracotomy.
| Variable | Posterior Prolapse | Bileaflet Prolapse | p Value |
|---|---|---|---|
| (n = 304) | (n = 131) | ||
| Ring size (mm) | 32 ± 4 | 37 ± 3 | <0.0001 |
| Aortic cross-clamp time (min) | 122 ± 48 | 101 ± 60 | 0.0008 |
| Cardiopulmonary bypass time (min) | 199 ± 48 | 186 ± 48 | 0.01 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


