Although opening an occluded infarct-related artery >24 hours after myocardial infarction in stable patients in the Occluded Artery Trial (OAT) did not reduce events over 7 years, there was a suggestion that the effect of treatment might differ by patient age. Baseline characteristics and outcomes by treatment with percutaneous coronary intervention (PCI) versus optimal medical therapy alone were compared by prespecified stratification at age 65 years. A p value <0.01 was prespecified as significant for OAT secondary analyses. The primary outcome was death, myocardial infarction, or New York Heart Association class IV heart failure. Patients aged >65 years (n = 641) were more likely to be female, to be nonsmokers, and to have hypertension, lower estimated glomerular filtration rates, and multivessel disease compared to younger patients (aged ≤65 years, n = 1,560) (p <0.001). There was no significant observed interaction between treatment assignment and age for the primary outcome after adjustment (p = 0.10), and there was no difference between PCI and optimal medical therapy observed in either age group. At 7-year follow-up, younger patients tended to have angina more often compared to the older group (hazard ratio 1.21, 99% confidence interval 1.00 to 1.46, p = 0.01). The 7-year composite primary outcome was more common in older patients (p <0.001), and age remained significant after covariate adjustment (hazard ratio 1.42, 99% confidence interval 1.09 to 1.84). The rate of early PCI complications was low in the 2 age groups. The trend toward a differential effect of PCI in the young versus the old for the primary outcome was likely driven by measured and unmeasured confounders and by chance. PCI reduces angina to a similar degree in the young and old. In conclusion, there is no indication for routine PCI to open a persistently occluded infarct-related artery in stable patients after myocardial infarction, regardless of age.
The Occluded Artery Trial (OAT) randomized stable patients with persistent occlusions of the infarct-related artery (IRA) >24 hours after myocardial infarction (MI) to optimal medical therapy with percutaneous coronary intervention (PCI) versus optimal medical therapy alone. Although in the overall OAT population, there was no clinical benefit of PCI on a composite outcome of death, MI, or New York Heart Association class IV heart failure after a mean follow-up period of 3 years, PCI reduced angina early in follow-up and, in a prespecified substudy, modestly reduced adverse remodeling at 1 year. There was also a trend observed (p = 0.03) toward an interaction between treatment and age >65 years on the primary outcome measure at 5 years, raising the possibility of a differential effect of PCI in older patients. We therefore set out to compare treatment and outcomes in detail in the 2 prespecified age groups.
Methods
The study design of OAT has been described previously. Patients with MI who underwent coronary angiography with persistent IRA occlusion >24 hours (3 to 28 calendar days, with symptom onset on day 1) were eligible if they had left ventricular ejection fractions ≤50% or proximal occlusions of major epicardial vessels. Exclusion criteria were New York Heart Association class III or IV heart failure, shock, a serum creatinine level >2.5 mg/dl, left main or 3-vessel coronary artery disease in need of surgical revascularization, rest angina, and high-grade ischemia on stress testing, which was required if the infarct zone was not akinetic or dyskinetic. Patients were randomly assigned to PCI with stent deployment and optimal medical therapy or optimal medical therapy alone. Follow-up during extended follow-up was conducted for up to 9 years by the participating sites or centrally for some patients. Event rates were presented at 7 years because of few events and unstable event rates in subsequent years. The mean follow-up duration for this analysis was 6.0 years.
The primary end point was a composite of death, reinfarction, or New York Heart Association class IV heart failure requiring hospitalization or treatment in a short-stay unit. Secondary end points included the separate components of the primary end point as well as symptoms and other clinical events. All study end point events were adjudicated by an independent events committee blinded to treatment assignment. The age stratification point, originally prespecified at 70 years, was changed to 65 years before the completion of enrollment because of a lower than anticipated number of participants aged >70 years. On the basis of the revised prespecified stratification, older patients (aged >65 years) enrolled in OAT were compared to younger patients (aged ≤65 years) with respect to baseline characteristics and outcomes by treatment assignment. Angina was assessed at baseline, 4 months, and yearly follow-up contacts.
Estimates of the cumulative event rates were calculated using the Kaplan-Meier product-limit method, and treatments were compared to the use of log-rank tests of the 7-year curves. Hazard ratios (HRs) and 99% confidence intervals (CIs) were calculated using Cox proportional-hazards regression models. Adjusted analyses incorporated variables from the risk model for the primary outcome. Data for patients lost to follow-up were censored as of the time of the last contact. Categorical variables were compared using chi-square tests, and continuous variables were compared using Student’s t tests. To control for type I error, p values ≤0.01 were prespecified by the study protocol as showing evidence of differences in secondary analyses. Analyses were performed according to the intention-to-treat principle. Statistical analyses were performed using SAS version 9.2 for Windows (SAS Institute Inc., Cary, North Carolina).
Results
Of the 2,201 randomized OAT subjects, 641 were aged >65 years, a prespecified subgroup, and 1,560 were aged ≤65 years, with an age range of 24 to 89 years. There were 37 patients aged >80 years. When comparing the OAT with the OAT Registry, there was no difference in mean age (58 ± 10 years). Among older randomized patients, 309 were assigned to PCI, and 332 were assigned to optimal medical therapy. Older patients were more likely to be female (35.3% vs 16.5%) and to have previous cerebrovascular disease (6.7% vs 2.5%), baseline heart failure (39.2% vs 28.6%), multivessel disease (22.1% vs 15.4%) and lower estimated glomerular filtration rates (70.4 vs 84.8 ml/min/1.73 m 2 ) (all p values <0.001; Table 1 ). They were also less likely to have family histories of coronary artery disease (30.1% vs 44.2%, p <0.001) and to be current smokers (18.1% vs 47.6%, p <0.001). The distribution of previous MI, previous coronary revascularization, and time from qualifying MI was similar between older and younger patients.
| Clinical characteristic | Age (years) | p Value | |
|---|---|---|---|
| ≤65 | >65 | ||
| (n = 1,560) | (n = 641) | ||
| Age (years) | 53.1 ± 7.6 | 72.0 ± 4.6 | <0.001 |
| Men | 83.5% | 64.7% | <0.001 |
| White | 79.2% | 82.4% | 0.09 |
| Body mass index (kg/m 2 ) | 28.8 ± 5.2 | 27.8 ± 4.5 | <0.001 |
| Diabetes mellitus | 20.3% | 21.5% | 0.50 |
| Previous angina pectoris | 21.3% | 25.4% | 0.03 |
| Previous MI | 10.9% | 12.0% | 0.45 |
| Previous cerebrovascular disease | 2.5% | 6.7% | <0.001 |
| Previous peripheral vascular disease | 3.3% | 5.0% | 0.05 |
| Previous hypertension | 44.7% | 58.3% | <0.001 |
| Previous hypercholesterolemia | 53.9% | 47.0% | 0.003 |
| Family history of coronary heart disease | 44.2% | 30.1% | <0.001 |
| Previous heart failure | 1.9% | 3.6% | 0.02 |
| Heart failure at baseline | 28.6% | 39.2% | <0.001 |
| Rales | 4.7% | 10.0% | <0.001 |
| New Q waves | 69.2% | 61.8% | <0.001 |
| Current smoker | 47.6% | 18.1% | <0.001 |
| Previous PCI | 5.0% | 4.2% | 0.43 |
| Previous coronary bypass surgery | 0.4% | 0.3% | 0.65 |
| Left ventricular ejection fraction (%) | 48.0 ± 10.8 | 47.0 ± 11.8 | 0.05 |
| Left ventricular ejection fraction <40% | 19.1% | 24.1% | 0.009 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 84.8 ± 20.6 | 70.4 ± 20.2 | <0.001 |
| ST-segment elevation | 66.3% | 66.2% | 0.97 |
| Coronary collateral vessels | 89.8% | 85.1% | 0.002 |
| Multivessel disease | 15.4% | 22.1% | <0.001 |
| Systolic blood pressure (mm Hg) | 119 ± 17 | 124 ± 19 | <0.001 |
Presenting features, ST-segment elevation electrocardiographic findings, and previous MI, as well as rates of previous PCI and coronary artery bypass grafting surgery were similar by patient age ( Table 1 ). Similar to the overall OAT population, among older patients, the right coronary artery was the most common IRA (45.6%), followed by the left anterior descending (40.6%) and then the left circumflex (13.9%) coronary arteries. The left anterior descending artery was more often the IRA in older than younger patients (40.6% vs 34.2%, p = 0.005). Older patients in the 2 treatment groups had a lower likelihood of angiographically visible collateral vessels and Q waves and were more likely to have multivessel disease; however, there were no significant differences in these characteristics between treatment groups within each age group. Left ventricular dysfunction was slightly more common among the elderly.
Compliance with guideline recommended medical treatment was excellent in the overall trial and in the elderly cohort ( Table 2 ). Compared to younger trial participants, the elderly group, however, had lower rates of aspirin and β blocker use (p <0.001). Only 75% of patients aged >65 years were treated with lipid-lowering agents. Older patients were more likely to be taking diuretics and antiarrhythmic agents (p <0.001) compared to the younger cohort ( Table 2 ).
| Medication | Age (years) | p Value | |
|---|---|---|---|
| ≤65 | >65 | ||
| (n = 1,560) | (n = 641) | ||
| Aspirin | 96.7% | 93.0% | <0.001 |
| Thienopyridine | 60.4% | 60.4% | 0.99 |
| β blockers | 89.0% | 84.9% | 0.008 |
| Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers | 79.6% | 82.7% | 0.09 |
| Lipid-lowering agents | 83.7% | 75.2% | <0.001 |
| Long acting nitrates | 20.3% | 28.2% | <0.001 |
| Calcium channel blockers | 5.3% | 7.2% | 0.09 |
| Warfarin | 8.7% | 12.3% | 0.01 |
| Oral hypoglycemic agents | 13.1% | 14.7% | 0.32 |
| Insulin | 6.7% | 5.0% | 0.13 |
| Diuretics | 12.6% | 27.1% | <0.001 |
| Antiarrhythmic agents | 2.4% | 7.3% | <0.001 |
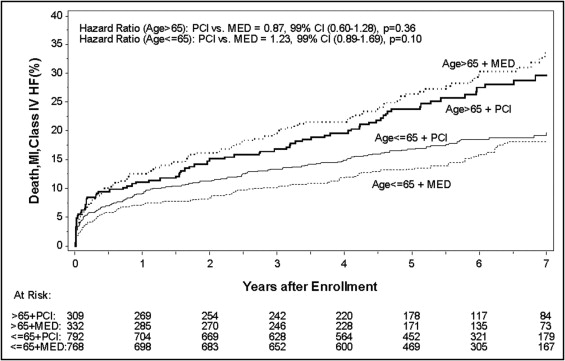
Observed event rates were significantly higher among those aged >65 years for the overall primary outcome (p <0.001) compared to younger trial participants irrespective of treatment assignment ( Figure 1 ) . The previously observed trend toward an age-treatment interaction on the primary outcome (p = 0.03) at 4-year follow-up was weaker after adjustment at 5-year (p = 0.06) and 7-year (p = 0.10) follow-up, and no significant age-treatment interactions were observed for any of the components of the primary outcome ( Table 3 ).
| Variable | Primary Outcome | Death | Fatal and Nonfatal MI | Class IV Heart Failure |
|---|---|---|---|---|
| Younger MED (n = 768) | 18.1% | 11.1% | 7.3% | 3.6% |
| Younger PCI (n = 792) | 19.2% | 10.8% | 8.3% | 3.7% |
| Older MED (n = 332) | 33.5% | 26.8% | 7.0% | 9.4% |
| Older PCI (n = 309) | 29.6% | 23.8% | 6.2% | 9.0% |
| Younger PCI vs MED, HR (99% CI) | 1.23 (0.89–1.69), p = 0.10 | 1.07 (0.71–1.63), p = 0.67 | 1.38 (0.83–2.30), p = 0.10 | 0.98 (0.49–1.98), p = 0.95 |
| Older PCI vs MED, HR (99% CI) | 0.87 (0.60–1.28), p = 0.36 | 0.91 (0.60–1.39), p = 0.58 | 0.81 (0.35–1.91), p = 0.53 | 0.99 (0.48–2.04), p = 0.96 |
| Unadjusted age-treatment interaction p value | 0.08 | 0.50 | 0.16 | 0.99 |
| Adjusted ⁎ age-treatment interaction p value | 0.10 | 0.47 | 0.17 | 0.88 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


