In patients with acute ST-elevation myocardial infarction (STEMI), a strategy of prehospital reduced dose fibrinolytic administration coupled with urgent percutaneous coronary intervention (PCI), termed FAST-PCI strategy, has been found to be superior to primary PCI (PPCI) alone. A coordinated STEMI system of care that includes FAST-PCI should offer better outcomes than a system in which prehospital diagnosis of STEMI is followed by PPCI alone. The aim of this study was to compare the in-hospital outcomes for patients treated with the FAST-PCI approach with outcomes for patients treated with the PPCI approach in a common system. The in-hospital data for 253 STEMI patients (March 2003–December 2009) treated with a FAST-PCI protocol were compared with 124 patients (January 2010–August 2011) treated with PPCI strategy alone. In-hospital mortality was the primary comparator. Stroke, major bleeding, and reinfarction during index hospitalization were also compared. The in-hospital mortality was significantly lower with FAST-PCI than with PPCI (2.77% vs 10.48%, p = 0.0017). Rates of stroke, reinfarction, and major bleeding were similar in the 2 groups. There was a lower frequency of pre-PCI Thrombolysis In Myocardial Infarction 0 flow (no patency) seen in patients treated with FAST-PCI compared with the PPCI patients (26.7% vs 62.7%, p <0.0001). Earlier infarct artery patency in the FAST-PCI group had a favorable impact on the incidence of cardiogenic shock on hospital arrival (3.1% vs 20.9%, p <0.0001). In conclusion, compared with a PPCI strategy in a common STEMI system of care, the FAST-PCI strategy was associated with earlier infarct artery patency and lower incidence of cardiogenic shock, as well as with reduced in-hospital mortality.
The mainstay of ST-elevation myocardial infarction (STEMI) treatment has been immediate reperfusion of the culprit artery to limit or prevent myocardial damage. The faster that reperfusion can be accomplished the better because ischemic time is directly proportional to both infarct size and mortality. Despite many advances in management strategies, a uniform system of care for STEMI patients that routinely accomplishes rapid reperfusion does not exist in many areas of the United States. A possible effective solution may be offered by the combination of reduced dose fibrinolytic therapy administered on the scene to eligible STEMI patients before transport to the hospital, followed by immediate percutaneous coronary intervention (PCI) on hospital arrival. This has been termed fibrinolytic acceleration of STEMI treatment combined with urgent PCI (FAST-PCI) approach. In a pooled analysis of almost 3,000 patients treated with either FAST-PCI or primary PCI alone (PPCI), patients treated with the FAST-PCI approach had >40% reduction in 30-day mortality without any bleeding penalty. The purpose of this study was to investigate changes in adverse outcomes of STEMI patients during a pause in the FAST-PCI strategy at our institution due to fibrinolytic unavailability and the consequent shift to a solely PPCI approach.
Methods
The protocol we have followed for more than 6 years using prehospital administration of a reduced-dose fibrinolytic agent followed by urgent PCI has been described previously. Patients with STEMI were identified before transport to our STEMI center hospital. They were given a regimen of reduced-dose reteplase (10 U intravenously), aspirin (325 mg orally), clopidogrel (600 mg orally), and heparin (60 U/kg, up to 4,000 U intravenously). Glycoprotein IIb/IIIa inhibitors were used according to local practice or at the discretion of the treating physician ( Figure 1 ).
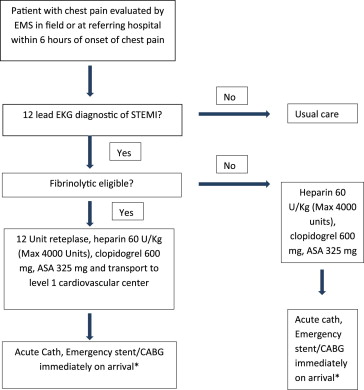
At the end of 2009, the manufacturer suspended delivery of the fibrinolytic we used (reteplase), causing our center to shift to a PPCI approach. Under this PPCI strategy, patients with STEMI were still identified in the field, either at the scene or in local referral hospitals. Adjunctive agents including aspirin, clopidogrel, and heparin, but without a fibrinolytic, could be administered and patient transport initiated, all in a similar manner as when the FAST-PCI protocol was in place. Urgent PCI on hospital arrival was also performed in a similar manner and by the same operators as under the FAST-PCI protocol.
From October 1, 2003, to December 31, 2009, 253 patients were identified in the field or at STEMI-referring hospitals by paramedics, nurses, or physicians and treated according to the FAST-PCI approach. After January 1, 2010, a pause in the FAST-PCI protocol due to fibrinolytic unavailability made PPCI the standard approach again for STEMI patients. From January 1, 2010, to August 31, 2011, 124 STEMI patients were treated according to a PPCI strategy. We examined data on STEMI patients treated under the previous FAST-PCI or the subsequent PPCI protocols. Total ischemic time was defined as the time from onset of symptoms to first intracoronary therapy (first balloon inflation or thrombus aspiration). Door-to-balloon time was defined as the time from patient’s arrival in the emergency department to first intracoronary balloon inflation. In-hospital clinical data for the 2 groups were compared. The primary end point comparison for this analysis was all-cause in-hospital mortality. Secondary end points were other in-hospital adverse outcomes such as reinfarction, major bleeding, and stroke. Reinfarction was defined as new significant Q waves in 2 contiguous leads different from those affected by initial MI, re-elevation of creatinine kinase-MB to higher levels than normal (or by another 50%, if already higher than normal), and re-elevation of CK-MB to >3 or >5 times upper limits of normal after angioplasty or surgery, respectively. Major bleeding was defined as bleeding resulting in substantial hemodynamic instability requiring intervention. Bleeding requiring blood transfusion but not associated with hemodynamic compromise was considered moderate and not severe. Development of a new neurologic deficit not present on initial screening examination or diagnosed by a neurologist or new intracranial bleeding diagnosed by computed tomography or magnetic resonance imaging were the criteria for stroke. Categorical variables were expressed as number and percentage of patients; statistical differences were analyzed using chi-square and Fisher exact tests. All continuous variables were expressed using mean and SD. Student t test was used to assess differences. A p value <.05 was considered statistically significant.
Results
Table 1 shows the patient demographics, clinical features, and angiographic details for the 2 groups. The groups were comparable, although a higher percentage of the PPCI group had a history of previous PCI. Notably, PPCI patients had a higher frequency of Killip Class IV (shock) at hospital arrival compared with FAST-PCI patients, and they had a higher frequency of occluded arteries (pre-PCI Thrombolysis In Myocardial Infarction [TIMI] 0 flow grade) on initial angiography. Approximately one-third of patients in both groups received glycoprotein IIb/IIIa inhibitors. A higher proportion of PPCI patients had 3-vessel coronary disease compared with FAST-PCI patients.
| Variable | FAST-PCI (n = 253) | PPCI (n = 124) | p Value |
|---|---|---|---|
| Age (yrs) | 58.1 ± 12.1 | 58.3 ± 11.6 | 0.878 |
| Men | 185 (73%) | 90 (73%) | 0.911 |
| Previous PCI | 30/253 (11.8%) | 29/124 (23.5%) | 0.003 |
| Previous myocardial infarction | 38/252 (15.1%) | 15/123 (12.1%) | 0.460 |
| Previous coronary bypass | 5/253 (1.9%) | 2/123 (1.6%) | 0.813 |
| Hypertension | 162/253 (64%) | 75/123 (60.9%) | 0.564 |
| Diabetes mellitus | 78/252 (30.9%) | 32/124 (26%) | 0.324 |
| Smoker | 170/250 (68%) | 75/121 (61.9%) | 0.251 |
| Hyperlipidemia | 122/251 (48.6%) | 55/124 (44.3%) | 0.479 |
| Creatinine | 1.0 ± 0.2 | 1.1 ± 0.6 | 0.017 |
| Killip class IV at presentation (shock) | 8/253 (3.1%) | 26/124 (20.9%) | <0.0001 |
| Ischemic time (min) | 173.5 ± 81.9 | 193.8 ± 99.1 | 0.07 |
| Door-to-balloon (min) | 26.9 ± 12.2 | 44.7 ± 34.2 | <0.0001 |
| TIMI 0 flow at presentation | 65/243 (26.7%) | 74/118 (62.7%) | <0.0001 |
| TIMI 3 flow at presentation | 109/243 (44.8%) | 26/118 (22%) | <0.0001 |
| 3-vessel coronary disease | 29/253 (11.4%) | 29/124 (23.3%) | 0.002 |
| Peak creatine kinase (IU/L) | 1,826.5 ± 1,946.1 | 2,220.2 ± 2,401.8 | 0.09 |
| Culprit vessel LAD | 85/239 (35.5%) | 58/121 (47.9%) | 0.023 |
| Glycoprotein IIb/IIIa inhibitors used | 88/253 (34.7%) | 43/124 (34.6%) | 0.983 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


