The aim of this study was to evaluate the 5-year clinical outcomes of patients who underwent sirolimus-eluting stent implantation for chronic total occlusion (CTO). Among 10,759 patients treated exclusively with sirolimus-eluting stent in the j-Cypher registry, clinical outcomes were compared between 1,210 patients with revascularization for CTO and 9,549 patients with revascularization for non-CTO only. The cumulative 5-year incidence of all-cause death (13.2% vs 14.3%, p = 0.56) and definite stent thrombosis (1.9% vs 1.6%, p = 0.76) was similar between the 2 groups. The adjusted risk for CTO relative to non-CTO for all-cause death and definite stent thrombosis was insignificant (hazard ratio [HR] 0.97, 95% confidence interval [CI] 0.81 to 1.16, and HR 0.99, 95% CI 0.6 to 1.65, respectively). The cumulative incidence of target lesion revascularization was significantly higher in the CTO group (20.7% vs 14.8%, p <0.001). The adjusted risk for target lesion revascularization was significant (HR 1.31, 95% CI 1.13 to 1.52, p <0.001). In the subgroup analysis, the risk for CTO for all-cause death tended to be lower in the subgroup of patients with left ventricular ejection fractions ≤40% (HR 0.68, 95% CI 0.45 to 1.01, p = 0.053), while the risk was significantly higher in the subgroup of patients with end-stage renal disease without hemodialysis (HR 1.66, 95% CI 1.02 to 2.70, p = 0.04). In conclusion, sirolimus-eluting stent implantation for CTO appears to be as safe as that for non-CTO for up to 5 years, except for the modestly elevated risk for target lesion revascularization and the higher risk for all-cause death in patients with end-stage renal disease without hemodialysis.
Despite the remarkable progress in percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) in the drug-eluting stent era, certain issues remain unresolved. First, although the use of drug-eluting stents for CTO, compared to the use of bare-metal stents, has been reported to reduce the risk for target vessel revascularization without compromising safety, the long-term (≥5-year) impact has not been fully elucidated. Second, although the decision to try PCI for CTO requires individualized risk-benefit analysis encompassing clinical, angiographic, and technical considerations, there are few data on long-term mortality in patients with CTO with co-morbidities such as left ventricular systolic dysfunction, end-stage renal disease (ESRD), and so on. To address these issues, we evaluated 5-year clinical outcomes in patients who underwent sirolimus-eluting stent (SES) implantation for CTO lesions, compared to patients who underwent SES implantation for non-CTO lesions, in a large multicenter observational database derived from real-world clinical practice in Japan.
Methods
The j-Cypher registry is a physician-initiated prospective, multicenter observational study in Japan enrolling consecutive patients in whom SES implantation was attempted. Details of the study design and the 5-year main results have been described previously. The relevant review boards of all 37 participating centers approved the study protocol, and written informed consent was obtained from all patients.
From August 2004 to November 2006, 12,824 patients were enrolled in the registry for the first time, and 10,778 patients (84%) were treated exclusively with SES. For the present analysis, 19 patients were excluded because of missing information on the presence of CTO, resulting in a study population of 1,210 patients who underwent PCI for CTO and 9,549 patients who underwent PCI for non-CTO only. The 14,779 lesions in 10,759 patients were divided into CTO lesions (n = 1,348) and non-CTO lesions (n = 13,431) to evaluate lesion characteristics of CTO compared to non-CTO lesions. In the CTO group, 453 patients underwent PCI for 595 non-CTO lesions as well, and 118 patients underwent PCI for multiple CTO lesions. Therefore, the CTO group had a total of 1,943 lesions (1,348 CTO lesions and 595 non=CTO lesions), and the non-CTO group had 12,836 lesions.
Five-year follow-up information was collected through review of hospital charts or contact with patients and/or referring physicians by site investigators or experienced research coordinators in the independent research organization (Research Institute for Production Development, Kyoto, Japan). When death, myocardial infarction, and stent thrombosis were reported, the events were adjudicated by a clinical events committee using the original source documents. The median follow-up intervals were 1,618 days (interquartile range 985 to 1,902) in the CTO group and 1,649 days (interquartile range 1,058 to 1,970) in the non-CTO group.
CTO was defined as complete obstruction of the vessel with Thrombolysis In Myocardial Infarction (TIMI) anterograde flow grade of 0 or 1, with an estimated duration of the occlusion of >1 month. The duration of occlusion was judged by the investigators at each participating center on the basis of the interval from the last episode of myocardial infarction in the same target vessel territory, previous coronary angiography, or changes in electrocardiographic findings. Procedural success was defined as a final diameter stenosis of <50% and a TIMI anterograde flow grade ≥2.
Death was regarded as cardiac in origin unless an obvious noncardiac cause could be identified. Any death during the index hospitalization was regarded as cardiac death. Myocardial infarction was adjudicated according to the definition in the Arterial Revascularization Therapy Study (ARTS). Within 1 week of the index procedure, only Q-wave myocardial infarction was adjudicated as myocardial infarction. Stent thrombosis was defined according to the Academic Research Consortium definition. Academic Research Consortium definite stent thrombosis was used as the end point for stent thrombosis in this study. Target lesion revascularization (TLR) was defined as either PCI or coronary artery bypass grafting surgery because of restenosis or stent thrombosis of the target lesion that included the proximal and distal edge segments and the ostium of the side branches. Stroke during follow-up was defined as ischemic or hemorrhagic stroke requiring hospitalization with symptoms lasting >24 hours.
The left ventricular ejection fraction (LVEF) was measured either by echocardiography or by angiography. The glomerular filtration rate was estimated using the Cockcroft-Gault formula. ESRD was defined as an estimated glomerular filtration rate ≤30 ml/min/1.73 m 2 using the Modification of Diet in Renal Disease (MDRD) study equation modified for Japanese patients.
The recommend antiplatelet regimen was aspirin (≥81 mg/day) indefinitely and thienopyridine (ticlopidine 200 mg/day or clopidogrel 75 mg/day) for ≥3 months. The duration of antiplatelet therapy was left to the discretion of each attending physician. The status of antiplatelet therapy during follow-up was assessed as previously reported, and persistent discontinuation of thienopyridine was defined as withdrawal lasting ≥2 months.
Categorical variables were reported as numbers and percentages and were compared using chi-square tests. Continuous variables are expressed as mean ± SD unless otherwise indicated. Continuous variables were compared using Student’s t test. Cumulative incidences were calculated using the Kaplan-Meier method, and differences were assessed using log-rank tests. We used the Cox proportional-hazard model to estimate hazard ratios (HRs) and their 95% confidence intervals (CIs) for the CTO group compared to the non-CTO group. A multivariate Cox proportional-hazards model was used to adjust the difference of baseline characteristics between the 2 groups. In the multivariate analysis, we simultaneously incorporated the CTO-group versus the non-CTO group together with 22 variables used in the previous report. Patients with missing values for any selected variable were excluded from the multivariate analysis. All analyses were conducted using SPSS version 17.0 (SPSS, Inc., Chicago, Illinois). All reported p values are 2 sided, and p values <0.05 were considered statistically significant.
Results
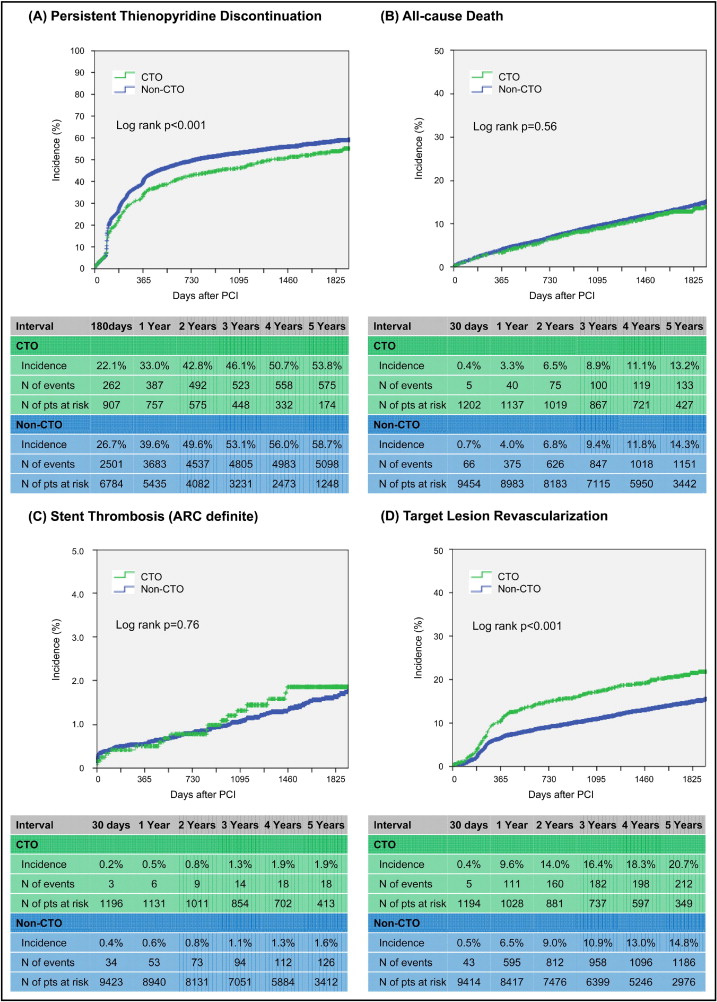
Patients in the CTO group were younger and more often had diabetes mellitus, smoking habits, previous myocardial infarctions, LVEFs ≤40%, and multivessel disease, while patients in the non-CTO group had a significantly higher incidence of acute coronary syndrome at presentation and target of unprotected left main coronary artery ( Table 1 ). The prevalence of hypertension, ESRD without hemodialysis, hemodialysis, and peripheral vascular disease did not differ significantly between the 2 groups. Procedural characteristics were significantly more complex in the CTO group, as reflected by the significantly greater number of vessels treated with a greater number of stents. During follow-up, cumulative incidence of persistent thienopyridine discontinuation at 5 years was significantly lower in the CTO group than in the non-CTO group (53.8% vs 58.7%, p <0.001; Figure 1 ).
| Variable | CTO | Non-CTO | |
|---|---|---|---|
| (n = 1,210) | (n = 9,549) | p Value | |
| Age (years) | 66.0 ± 10.7 | 68.6 ± 10.1 | <0.001 |
| ≥80 years ⁎ | 109 (9.0%) | 1,251 (13%) | <0.001 |
| Men ⁎ | 989 (82%) | 7,116 (75%) | <0.001 |
| Body mass index (kg/m 2 ) | 24.5 ± 3.7 | 23.9 ± 3.3 | <0.001 |
| <25.0 kg/m 2 ⁎ | 717 (59%) | 6,276 (66%) | <0.001 |
| Hypertension ⁎ | 886 (73%) | 7,168 (75%) | 0.16 |
| Diabetes mellitus ⁎ | 531 (44%) | 3,864 (41%) | 0.02 |
| Insulin-treated | 120 (9.9%) | 875 (9.2%) | 0.39 |
| Current smoking ⁎ | 293 (24%) | 1,821 (19%) | <0.001 |
| ESRD | |||
| Without hemodialysis ⁎ | 48 (4.0%) | 474 (5.0%) | 0.13 |
| With hemodialysis | 54 (4.5%) | 538 (5.6%) | 0.09 |
| Acute coronary syndromes ⁎ | 150 (12%) | 2,154 (23%) | <0.001 |
| ST-segment elevation myocardial infarction | 29 (2.4%) | 703 (7.4%) | |
| Non-ST-segment elevation myocardial infarction | 23 (1.9%) | 196 (2.1%) | |
| Unstable angina | 98 (8.1%) | 1,255 (13%) | |
| Previous myocardial infarction ⁎ | 420 (35%) | 2,601 (27%) | <0.001 |
| Previous stroke ⁎ | 131 (11%) | 873 (9.1%) | 0.06 |
| Peripheral vascular disease ⁎ | 154 (13%) | 1,119 (12%) | 0.31 |
| Previous heart failure ⁎ | 209 (17%) | 1,248 (13%) | <0.001 |
| Previous PCI ⁎ | 527 (44%) | 4,645 (49%) | 0.001 |
| Previous coronary artery bypass grafting ⁎ | 104 (8.6%) | 681 (7.1%) | 0.07 |
| Multivessel disease | 734 (61%) | 4,646 (49%) | <0.001 |
| Target of proximal left anterior descending coronary artery ⁎ | 567 (47%) | 4,705 (49%) | 0.11 |
| Target of unprotected left main coronary artery ⁎ | 23 (1.9%) | 396 (4.1%) | <0.001 |
| Target of in-stent restenosis ⁎ | 188 (16%) | 1,516 (16%) | 0.76 |
| Side branch stenting ⁎ | 66 (5.5%) | 399 (4.2%) | 0.04 |
| LVEF (%) | 54.3 ± 14.0 | 58.6 ± 13.2 | <0.001 |
| ≤40% | 182 (17%) | 868 (10%) | <0.001 |
| Number of vessels treated | 1.36 ± 0.59 | 1.20 ± 0.45 | <0.001 |
| Multivessel stenting | 357 (30%) | 1,723 (18%) | <0.001 |
| Number of lesion treated | 1.53 ± 0.78 | 1.34 ± 0.62 | <0.001 |
| Reference vessel diameter <2.5 mm ⁎ | 445 (38%) | 3,137 (33%) | 0.001 |
| Total number of stents | 2.51 ± 1.42 | 1.71 ± 1.03 | <0.001 |
| Total length of stents (mm) | 60.9 ± 36.4 | 37.1 ± 24.3 | <0.001 |
| Total length of stents >28 mm ⁎ | 924 (76%) | 4,448 (47%) | <0.001 |
| Use of intravascular ultrasound ⁎ | 584 (48%) | 4,567 (48%) | 0.77 |
Compared to non-CTO lesions, CTO lesions were located more frequently in the right coronary artery, and were significantly more frequently associated with severe calcification and long lesion length (≥30 mm), resulting in use of greater number of stents ( Table 2 ). Direct stenting, postdilatation after stent implantation, and the use of intravascular ultrasound were more common for non-CTO lesions. The prevalence of in-stent restenotic lesions was not significantly different between the 2 groups. The procedural success rate was significantly higher for the non-CTO lesions (93.4% vs 99.6%, p <0.001).
| Variable | CTO | Non-CTO | |
|---|---|---|---|
| (n = 1,348) | (n = 13,431) | p Value | |
| Lesion location | <0.001 | ||
| Left anterior descending coronary artery | 475 (35%) | 5,650 (42%) | |
| Left circumflex coronary artery | 258 (19%) | 2,866 (21%) | |
| Right coronary artery | 602 (45%) | 4,298 (32%) | |
| Left main coronary artery | 11 (0.8%) | 488 (3.6%) | |
| Saphenous vein graft | 2 (0.1%) | 107 (0.8%) | |
| CTO | 1,348 (100%) | 0 (0.0%) | <0.001 |
| In-stent restenosis | 184 (14%) | 1,711 (13%) | 0.34 |
| Severe calcification | 149 (11%) | 1,162 (8.7%) | 0.003 |
| Bifurcation lesion | 218 (16%) | 2,635 (20%) | 0.002 |
| Side branch stenting | 51 (3.8%) | 428 (3.2%) | 0.24 |
| Lesion length ≥30 mm | 549 (42%) | 1,597 (12%) | <0.001 |
| Procedural reference diameter <2.5 mm | 393 (30%) | 3,803 (29%) | 0.29 |
| American College of Cardiology/American Heart Association type | <0.001 | ||
| A | 1,225 (9.1%) | ||
| B1 | 17 (1.3%) | 3,544 (26%) | |
| B2 | 114 (8.5%) | 5,511 (41%) | |
| C | 1,210 (90%) | 3,094 (23%) | |
| Use of intravascular ultrasound | 557 (41%) | 6,123 (46%) | 0.003 |
| Direct stenting | 25 (1.9%) | 3,385 (25%) | <0.001 |
| Postdilatation | 494 (39%) | 5,988 (45%) | <0.001 |
| Maximum inflation pressure (atm) | 18.2 ± 3.37 | 17.9 ± 3.31 | 0.005 |
| Number of stents used | 1.81 ± 0.91 | 1.28 ± 0.60 | <0.001 |
| Length of stents used (mm) | 44.8 ± 24.3 | 27.8 ± 14.7 | <0.001 |
| Minimal stent size (mm) | 2.75 ± 0.31 | 2.90 ± 0.37 | <0.001 |
| Procedural success | 1,259 (93.4%) | 13,378 (99.6%) | <0.001 |
| Unsuccessful guidewire crossing | 73 (5.4%) | 25 (0.2%) | <0.001 |
| Unsuccessful device deliver | 7 (0.5%) | 10 (0.1%) | <0.001 |
At 30 days, the cumulative incidence of all-cause death (0.4% vs 0.7%), myocardial infarction (0.2% vs 0.4%), and coronary artery bypass grafting (0.2% vs 0.1%) was similar between the CTO and non-CTO groups ( Table 3 ). The cumulative 5-year incidence of all-cause death (13.2% vs 14.3%, p = 0.56) and definite stent thrombosis (1.9% vs 1.6%, p = 0.76) did not differ between the CTO and non-CTO groups ( Table 3 , Figure 1 ). After adjusting for potential confounders, the risk for the CTO group relative to the non-CTO group for all-cause death and definite stent thrombosis remained insignificant (HR 0.97, 95% CI 0.81 to 1.16, p = 0.72, and HR 0.99, 95% CI 0.6 to 1.65, p = 0.97, respectively; Table 4 ). Regarding other clinical end points such as cardiac death, sudden death, myocardial infarction, stroke, coronary artery bypass grafting surgery, and heart failure hospitalization, unadjusted and adjusted outcomes were also similar between the CTO and non-CTO groups ( Tables 3 and 4 ). The cumulative 5-year incidence of TLR (20.7% vs 14.8%, p <0.001) and any coronary revascularization (42.1% vs 36.3%, p <0.001) were significantly higher in the CTO group than in the non-CTO group. The adjusted risks of the CTO group relative to the non-CTO group for TLR and any coronary revascularization were modest but significant (HR 1.31, 95% CI 1.13 to 1.52, p <0.001, and HR 1.17, 95% CI 1.06 to 1.3, p = 0.003, respectively; Table 4 ). It is noteworthy that 12 of 18 stent thromboses (66.7%) and 101 of 212 episodes of TLR (47.6%) occurred beyond 1 year in the CTO group.
| Variable | Events, Incidence (%) | p Value | |
|---|---|---|---|
| CTO (n = 1,210) | Non-CTO (n = 9,549) | ||
| 30 days | |||
| All-cause death | 5 (0.4%) | 66 (0.7%) | |
| Cardiac death | 5 (0.4%) | 64 (0.7%) | |
| Sudden death | 0 (0.0%) | 7 (0.1%) | |
| Myocardial infarction | 3 (0.2%) | 35 (0.4%) | |
| Stroke | 3 (0.2%) | 36 (0.4%) | |
| Definite/probable stent thrombosis | 3 (0.2%) | 47 (0.5%) | |
| Definite stent thrombosis | 3 (0.2%) | 34 (0.4%) | |
| TLR | 5 (0.4%) | 43 (0.5%) | |
| Coronary artery bypass grafting surgery | 2 (0.2%) | 8 (0.1%) | |
| Any revascularization | 45 (3.7%) | 227 (2.4%) | |
| Heart failure hospitalization | 2 (0.2%) | 36 (0.4%) | |
| 1 year | |||
| All-cause death | 40 (3.3%) | 375 (4.0%) | |
| Cardiac death | 26 (2.2%) | 217 (2.3%) | |
| Sudden death | 11 (0.9%) | 62 (0.7%) | |
| Myocardial infarction | 16 (1.4%) | 89 (0.9%) | |
| Stroke | 25 (2.1%) | 169 (1.8%) | |
| Definite/probable stent thrombosis | 6 (0.5%) | 68 (0.7%) | |
| Definite stent thrombosis | 6 (0.5%) | 53 (0.6%) | |
| TLR | 111 (9.6%) | 595 (6.5%) | |
| Coronary artery bypass grafting surgery | 14 (1.2%) | 79 (0.9%) | |
| Any revascularization | 286 (24.4%) | 1,754 (19.0%) | |
| Heart failure hospitalization | 42 (3.6%) | 291 (3.1%) | |
| 5 years | |||
| All-cause death | 133 (13.2%) | 1,151 (14.3%) | 0.56 |
| Cardiac death | 69 (6.7%) | 531 (6.7%) | 0.7 |
| Sudden death | 27 (2.7%) | 183 (2.4%) | 0.47 |
| Myocardial infarction | 42 (4.2%) | 273 (3.6%) | 0.35 |
| Stroke | 67 (7.1%) | 442 (5.7%) | 0.16 |
| Definite/probable stent thrombosis | 20 (2.0%) | 151 (1.9%) | 0.98 |
| Definite stent thrombosis | 18 (1.9%) | 126 (1.6%) | 0.76 |
| TLR | 212 (20.7%) | 1,186 (14.8%) | <0.001 |
| Coronary artery bypass grafting surgery | 25 (2.5%) | 208 (2.8%) | 0.81 |
| Any revascularization | 448 (42.1%) | 2,989 (36.3%) | <0.001 |
| Heart failure hospitalization | 91 (9.2%) | 686 (8.8%) | 0.35 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


