Native valve infective endocarditis (IE) in patients with normal valves has increased in the last decades. Whether patients with normal valves present a similar prognosis to those with pathologic valves is unresolved. Our aim is to describe epidemiologic and clinical differences between patients with left-sided IE and normal valves and those with native pathologic valves. We analyzed 945 consecutive episodes of IE, 435 of which involved left-sided nonprosthetic IE. They were classified into 2 groups: episodes in normal valves (normal group, n = 173) and episodes in pathologic valves (abnormal group, n = 262). Patients in the normal group were younger, Staphylococcus aureus and Streptococcus bovis were more frequently isolated, and vegetations were more frequently found. Heart failure, septic shock, and the need for surgery or death were more common. Multivariate analysis identified the following as factors independently associated with normal valve IE: age <65 years, S bovis , S aureus , heart failure, and vegetation detection. Factors independently associated with in-hospital events included S aureus , periannular complications, heart failure, and septic shock development. In conclusion, compared with patients with abnormal valve IE, patients with IE on normal valves were younger, had a more virulent microbiological profile, developed heart failure and septic shock more frequently, needed more surgical procedures, and had worse prognosis.
Historically, infective endocarditis (IE) was predominantly a disease of patients with underlying heart conditions, mostly rheumatic valve disease, with oral streptococci being the most frequent causative pathogens. This clinical and microbiological profile has undergone a significant change in the last decades in developed countries. Degenerative valve disease, that is, elderly subjects with valve sclerosis, and mitral valve prolapse are nowadays the most common predisposing conditions in native valve IE ; the proportion of patients with IE without previously known valvular disease has definitively increased in many series, and staphylococci are at present the microorganisms most frequently associated with this disease. The aim of the present study was to describe the differences in the epidemiology, clinical course, echocardiographic findings, microbiological profile, and in-hospital outcome between patients with left-sided IE without underlying heart disease (normal native valves) and those with preexisting native valve disease.
Methods
This work was conducted at 3 tertiary care centers with surgical facilities that have been working together on IE since the beginning of the study. Standardized protocols, uniform data collection, and identical diagnostic and therapeutic criteria were used. From 1996 to 2012, a total of 945 consecutive episodes of IE were prospectively recorded in an on-going multipurpose database, 435 of which involved left-sided nonprosthetic IE and were included in the study. Right-sided IE, episodes in patients who were intravenous drug users, and intracardiac device infections were excluded because their epidemiology, clinical presentation, and prognosis are totally different. Patients with a pacemaker or implantable defibrillator could be included if they had valvular infection and no evidence of lead infection.
For purposes of analysis and comparison we distinguished 2 groups: episodes of IE in normal valves (normal group, n = 173) and episodes in pathologic valves (abnormal group, n = 262). To ensure consecutive enrollment, all patients who underwent echocardiography to rule out IE were clinically followed up until a diagnosis was established. Patients with a final diagnosis of IE were included in the study. Duke criteria were applied until 2002 and modified Duke criteria thereafter. The local ethical committees approved this registry.
All patients underwent a detailed clinical history, physical examination, electrocardiography, blood analysis, urinalysis, a set of 3 blood cultures at admission, 3 additional blood cultures 48 to 72 hours later, and transthoracic and transesophageal echocardiography (TEE). If blood cultures were negative after 72 hours, specific serologic tests were done for Chlamydia , Brucella , Q fever, Legionella , and Mycoplasma .
Nosocomial IE was defined as endocarditis acquired >3 days after hospital admission with no clinical manifestations of endocarditis before admission. Acute-onset IE was applied when the time between the appearance of symptoms and hospital admission was <15 days. Septic shock was defined as the presence of an acute circulatory failure in sepsis, characterized by persistent arterial hypotension (systolic pressure <90 mm Hg) despite adequate volume resuscitation. Heart failure was diagnosed on the basis of guidelines criteria.
The anatomic classification of the underlying morphology of the infected valve was based on echocardiographic findings (echocardiography performed during the present admission and previous echocardiograms when available) and patients’ clinical history. The morphology of noninfected valves was also considered. Rheumatic valve disease was defined as the presence of clinical history of chronic rheumatic heart disease and typical echocardiographic findings such as commissural fusion, calcification and variable thickening of the leaflets, especially at the level of their free edges, and in the case of the mitral valve, thickening, fusion, and shortening of the mitral chordae. In most cases, a characteristic bowing or doming of the mitral valve leaflets in diastole can be seen. Degenerative valve disease was determined when in absence of a history of rheumatic heart disease there was thickening and calcification of the aortic leaflets, mainly in the central part of each cusp, without commissural fusion; thickening and calcification of the mitroaortic continuity; and calcification of the mitral posterior annulus. The mitral leaflet tips are thin and mobile without commissural fusion. Myxomatous mitral valve disease was characterized by thickened redundant leaflets and chordae, with excessive motion and bulging or protrusion of portions of the leaflets into the left atrium in systole, sometimes accompanied by chordal rupture. Congenital lesions such as bicuspid aortic valve were considered as classically defined in the literature. The infected valve was considered normal when in a patient without previously known heart disease there was no commissural fusion and the leaflets and chordae, especially those segments that had not been distorted by the infection, had a normal echocardiographic appearance.
To determine the degree of variability in the classification of the underlying morphology, the observer was subjected to a reliability study (random sample, n = 30), and a kappa index of 0.910 (p <0.001) was obtained.
Perivalvular complications and vegetation measurements have been defined in detail elsewhere.
Empirical antibiotic regimens were chosen for culture-negative cases according to established guidelines. Urgent surgery, defined as surgery done before antibiotic regimen was completed, was performed following the current guideline indications.
Continuous variables are reported as mean and SD. They were compared by a 2-tailed Student t test. Categorical variables are expressed as a frequency and a percentage and were compared with the chi-square test and Fisher’s exact test, when appropriate. Influence of different variables in normal native valve infection was first tested in a univariate analysis (Pearson chi-square test). The prognostic impact of infection on a normal valve in the development of clinical events was also assessed in a univariate analysis. A multivariate logistic regression analysis was performed by means of a backward logistic method to find the variables independently associated with normal native valve infection, considering normal native valve infection as the dependent variable.
Finally, by means of a backward stepwise method, we performed 3 multivariate analyses to determine the impact of the infection of a normal valve on the prognosis of patients with native valve IE. Death, surgery, and the combination of death and surgery were considered dependent variables. The adjusted odds ratios with 95% confidence intervals for each variable have been calculated. When a change in odds ratio >10% was found, the variable was considered clinically relevant. No significant multicollinearity was detected in the models.
All tests were 2-sided, and differences were considered statistically significant at p values <0.05. Statistical analysis was performed with PASW Statistics V 17.0 (SPSS Inc., Chicago, Illinois).
Results
Left-sided native valve endocarditis was diagnosed in 435 cases, 92.9% of which were definite and 7.1% were possible IE episodes. Of these patients, 173 (39.8%) had no underlying heart disease (normal group) and 262 (60.2%) had some sort of chronic valvular disease (abnormal group). A total of 95.4% of patients in the normal group and 91.2% in the abnormal group met definite criteria for IE. The most common predisposing cardiac condition in this latter group was degenerative valve disease ( Figure 1 ). Demographic characteristics, co-morbidities, and clinical presentation comparisons between groups are summarized in Table 1 . Patients with normal valves were younger. Regarding co-morbidity, alcoholism was more frequent in the normal group, whereas chronic anemia was more common in the abnormal group.

| Variable | Valve Before Infective Endocarditis | p | |
|---|---|---|---|
| Normal (n = 173) | Abnormal (n = 262) | ||
| Age (years) | 60 (14) | 64 (15) | 0.003 ∗ |
| Man | 125 (72.3%) | 170 (64.9%) | 0.107 |
| Referred | 73 (42.2%) | 98 (37.4%) | 0.320 |
| Nosocomial acquisition | 32 (18.6%) | 45 (17.3%) | 0.700 |
| Antibiotic prophylaxis | 3 (2.7%) | 14 (8%) | 0.059 |
| Comorbidity | |||
| Diabetes mellitus | 32 (18.5%) | 58 (22.1%) | 0.360 |
| Chronic anemia † | 26 (15%) | 61 (23.4%) | 0.034 ∗ |
| Chronic renal failure | 10 (5.8%) | 27 (10.3%) | 0.095 |
| Malignant neoplasia | 21 (12.1%) | 29 (11.1%) | 0.750 |
| Chronic obstructive pulmonary disease | 13 (7.5%) | 25 (9.6%) | 0.460 |
| Alcoholism | 23 (13.3%) | 16 (6.1%) | 0.011 ∗ |
† Chronic anemia: hemoglobin concentration <10 g/dl known before the onset of symptoms of IE.
The appearance of a new precordial murmur was more common in episodes with normal valves (63.6% vs 44.4%, p <0.001). No other differences were found in clinical presentation at admission. The mean duration of symptoms before diagnosis was similar in both groups (32.8 [38.6] vs 37.3 [55.7] days, p = 0.61).
Table 2 lists the microbiological profile and echocardiographic findings of both groups of patients. Staphylococcus aureus and Streptococcus bovis were more frequently isolated in patients with normal valves.
| Variable | Valve Before Infective Endocarditis | p | |
|---|---|---|---|
| Normal (n = 173) | Abnormal (n = 262) | ||
| Microbiologic profile | |||
| Streptococcus bovis | 15 (8.7%) | 7 (2.7%) | 0.005 ∗ |
| Viridans group streptococci | 27 (15.7%) | 53 (20.2%) | 0.330 |
| Enterococci | 14 (8.1%) | 26 (9.9%) | 0.530 |
| Streptococci (others) | 16 (9.3%) | 29 (11.1%) | 0.550 |
| Staphylococcus aureus | 41 (23.8%) | 40 (15.3%) | 0.025 ∗ |
| Coagulase-negative staphylococci | 13 (7.6%) | 34 (13%) | 0.076 ∗ |
| Gram-negative bacilli | 8 (4.7%) | 11 (4.2%) | 0.820 |
| Fungi | 1 (0.6%) | 3 (1.1%) | 0.480 |
| HACEK | 1 (0.6%) | 2 (0.8%) | 0.650 |
| Anaerobes | 1 (0.6%) | 0 (0%) | 0.401 |
| Polymicrobial | 8 (4.7%) | 13 (5%) | 0.880 |
| Others | 2 (1.2%) | 9 (3.4%) | 0.141 |
| Negative cultures | 25 (14.5%) | 35 (13.4%) | 0.730 |
| Echocardiographic findings | |||
| Location of the vegetations | |||
| Aortic valve | 76 (44%) | 104 (39.7%) | 0.340 |
| Mitral valve | 67 (38.7%) | 116 (44.3%) | 0.340 |
| Both valves infected | 30 (17.3%) | 42 (16%) | 0.340 |
| Vegetations: | |||
| Detection by echocardiography | 162 (93.6%) | 228 (87%) | 0.027 ∗ |
| Size ≥10 mm | 107 (79.3%) | 133 (68.2) | 0.027 ∗ |
| Moderate-severe valve insufficiency | 152 (87.9%) | 210 (80.2%) | 0.035 ∗ |
| Periannular complications: | |||
| Abscess | 29 (16.8%) | 52 (19.8%) | 0.420 |
| Pseudoaneurysm | 29 (16.8%) | 47 (17.9%) | 0.751 |
| Fistula | 5 (2.9%) | 9 (3.4%) | 0.752 |
Vegetations were more frequently found in the normal group and were also larger. The presence of periannular complications was similar in both groups.
During hospitalization, patients with normal valves had higher rates of heart failure and septic shock. The need for surgery was higher in this group, and a trend to higher rates of embolization and mortality was also observed in these patients ( Table 3 ).
| Variable | Valve Before Infective Endocarditis | p | |
|---|---|---|---|
| Normal (n = 173) | Abnormal (n = 262) | ||
| Hospital stay (days) | 40.6 (39.3) | 36.3 (32.1) | 0.260 |
| Heart failure | 116 (67.1%) | 145 (55.3%) | 0.015 ∗ |
| Central nervous system embolism | 45 (26.1%) | 55 (21%) | 0.220 |
| Embolisms (total) | 28 (14.9%) | 26 (9.8%) | 0.097 |
| Acute renal insufficiency | 33 (19.1%) | 48 (18.3%) | 0.840 |
| Atrioventricular block | 6 (3.5%) | 22 (8.4%) | 0.040 ∗ |
| Septic shock | 42 (24.6%) | 43 (16.5%) | 0.041 ∗ |
| Cardiac surgery | 105 (60.7%) | 132 (50.4%) | 0.035 ∗ |
| Death | 53 (30.6%) | 65 (24.8%) | 0.181 |
| Cardiac surgery or death | 132 (76.3%) | 171 (65.3%) | 0.014 ∗ |
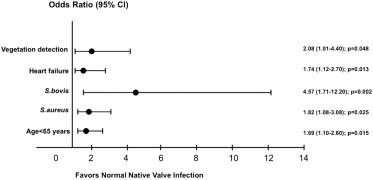
A multivariate analysis to determine the variables that were independently associated with normal native valve IE was performed. We included in the model the variables that were significant in the univariate analysis (age, S aureus , S bovis , vegetation detection, vegetation size, heart failure, septic shock, chronic anemia, and alcoholism). Variables independently associated with IE in patients without underlying heart disease were age<65 years, S aureus , S bovis , heart failure, and vegetation detection ( Figure 2 ).