We evaluated the clinical efficacy and cost of a cardiac imaging strategy versus a traditional exercise tolerance test (ETT) strategy for the investigation of suspected stable coronary artery disease (CAD). We retrospectively collected data of consecutive patients seen in rapid access chest pain clinics at 2 UK hospitals for a period of 12 months. Hospital A investigated patients by performing ETT. Hospital B investigated patients using cardiac imaging test; 483 patients from hospital A and 295 from hospital B were included. In hospital A, 209 patients (43.3%) had contraindication to ETT. Of those who had ETT, 151 (55.1%) had negative ETT, 68 (24.8%) had equivocal ETT, and 55 (20.1%) had positive ETT, of which 53 (96.4%) had invasive coronary angiography (ICA), and of these 23 (43.4%) had obstructive CAD. In hospital B, 26 patients (8.8%) with low pretest probability had calcium score and 3 (11.5%) were positive leading to computed tomography coronary angiography; 98 patients (33.2%) with intermediate pretest probability had computed tomography coronary angiography and 5 (5.1%) were positive; 77 patients (26.1%) had stress echocardiogram and 6 (7.8%) were positive; and 57 patients (19.3%) had myocardial perfusion scintigraphy and 11 (19.3%) were positive. Hospital A performed 127 ICA (26.3% of population) and 52 (40.9%) had obstructive CAD. Hospital B performed 63 ICA (21.4% of population) and 32 (50.8%) had obstructive CAD. The average cost per patient in hospital A was £566.6 ± 490.0 ($875 ± 758) and in hospital B was £487.9 ± 469.6 ($750 ± 725) (p <0.001). In conclusion, our results suggest that a cardiac imaging pathway leads to fewer ICA and a higher yield of obstructive CAD at lower cost per patient.
There is a significant difference between the UK National Institute of Health and Care Excellence (NICE) and the European Society of Cardiology (ESC) guidelines on stable coronary artery disease (CAD), which advocate cardiac imaging tests, as the initial investigations and the American Societies of Cardiology (ASC) guideline, which advocate the use of the exercise tolerance test (ETT) as the initial investigation, where possible. NICE guidelines provide a risk score (RS) to assess the pretest probability (PTP) for CAD derived from the Duke Clinical Score. They recommend the use of calcium score for patients with low PTP and computed tomography coronary angiography (CTCA) if the calcium score is positive and functional tests for patients with moderate PTP. Our previous studies demonstrated that the NICE PTP RS overestimates the incidence of CAD, which NICE anticipated in their guideline. Hence, we have extended the use of CTCA to patients with intermediate PTP RS and functional imaging tests to patients with high PTP RS. This modified NICE model is similar to the ESC guidelines, which recommends the use of CTCA in patients with low-to-intermediate PTP of 15% to 50% and functional imaging testing for patients with PTP 15% to 85%, using the modified Diamond-Forrester RS. In this study, we compare the clinical efficacy and cost of the traditional ASC ETT first diagnostic pathway with the NICE/ESC cardiac imaging first diagnostic pathway for the investigation of patients with suspected stable CAD.
Methods
We retrospectively collected data from January to December 2013 of consecutive patients seen in rapid access chest pain clinics at 2 UK district general hospital within the same trust, hospital A and hospital B. Patients with suspected stable CAD were included. Patients with noncardiac chest pain and those with known CAD were excluded. Suspected stable CAD was defined as atypical or typical cardiac chest pain.
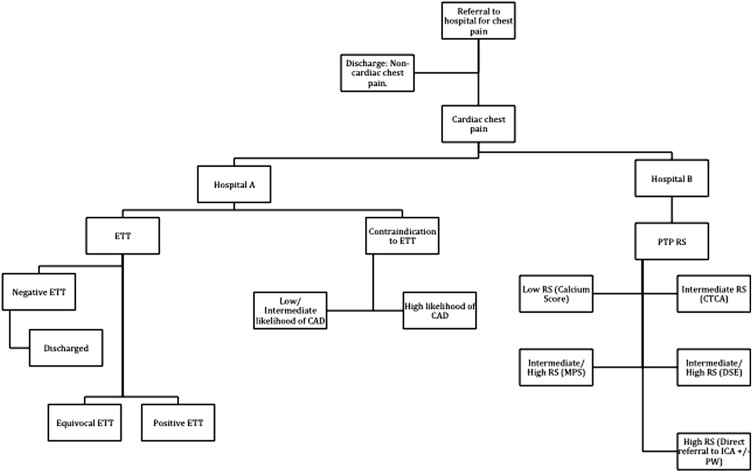
Hospital A investigated patients by performing ETT in all patients in the first instance except those who were not able to exercise or had an abnormal baseline electrocardiogram. Patients not suitable for ETT were clinically judged by a cardiologist to be either low-intermediate likelihood of CAD or high likelihood of CAD. Hospital B investigated patients using a modified NICE guideline, whereby expanding the use of CTCA to patients with intermediate RS and the functional imaging tests to patients with high RS ( Figure 1 ). Patients with equivocal or positive noninvasive investigations underwent subsequent investigations. The 2014 to 2015 NHS tariff was used for cost analysis: ETT £170 ($262), coronary calcium score £97 ($149), CT coronary angiogram £164 ($252), dobutamine stress echocardiogram (DSE) £288 ($443), myocardial perfusion scintigraphy (MPS) £373 ($575), and diagnostic invasive coronary angiogram £1241 ($1,911).
Information including patient demographics, baseline cardiac history, CAD risk factors, and symptoms were obtained. Typical chest pain was defined as: (1) constricting discomfort in the front of the chest, in the neck, shoulders, jaw, or arms; (2) precipitated by physical exertion; and (3) relieved by rest or glyceryl trinitrate within 5 minutes. Atypical chest pain was classed as 2 factors defining typical chest pain. Nonanginal chest pain was classed as 1 (or zero) factor defining typical chest pain.
Bruce protocol was used for ETT. A specialist nurse and a cardiac physiologist performed the ETT, and the results were reviewed by a consultant cardiologist. Contraindications for ETT were abnormal baseline resting electrocardiogram (including minor ST-segment abnormalities and right and left bundle branch block morphology), uncontrolled hypertension, and inability to exercise. Beta blockers were discontinued before the investigation. Positive ETT was defined as ≥1-mm ST-segment depression in 2 consecutive leads. Equivocal ETT was defined as symptoms of chest pain without ST-segment depression.
Cardiac CT patients were beta blocked by the referring clinician (atenolol 50 mg) and/or intravenously with metoprolol (5 to 30 mg), aiming to achieve a heart rate of <60 bpm. Noncontrast calcium score scan was performed first (kvp = 120). This was followed by the injection of 80 ml of contrast (5 ml/s) into a large vein for the CTCA. Hospital A used a Phillips, Netherlands, 256-slice Brilliance iCT scanner and hospital B used a General Electric, USA, 64-slice LightSpeed VCT XTe scanner. Both hospitals used prospective gating to lower the radiation dose. Significant CAD on CTCA was defined as >50% diameter stenosis.
Dobutamine stress echocardiograms were scanned using a Philips IE33 echocardiography machine. The images were acquired by a senior sonographer and reported by a consultant cardiologist. Intravenous dobutamine was administered through a syringe pump starting with 10 μg/kg/min and increased in increments up to a maximum of 40 μg/kg/min. Boluses of atropine up to a maximum of 1 mg were added if the target heart rate of 85% of maximum predicted was not achieved. Sonovue contrast was used at the discretion of the cardiologist. A 16-segment model was used, new regional wall motion abnormality in 2 adjacent segments, of which only 1 can be an apical segment, was defined as a positive test.
Myocardial perfusion scintigraphy studies were performed under standard protocols with a single-photon emission computed tomography-CT with technetium radiotracer. Images were acquired at rest and after stress, which was induced with dipyridamole (0.56 mg/kg over 4 minutes), followed by injection of the radiotracer. All images were reviewed jointly by a radiologist and a cardiologist. A 17-segment model was used; new perfusion defect in 2 adjacent segments was defined as a positive test.
Invasive coronary angiogram studies were performed in cardiac catheterization laboratory by a consultant interventional cardiologist, who made the clinical judgment whether there was obstructive coronary artery stenosis based on anatomical findings. Pressure wire study was performed for equivocal stenosis.
Statistical analyses were performed using SPSS, version 18.0 (SPSS, Inc., Chicago, Illinois). Variables were tested for normality using the Kolmogorov-Smirnov test. Values are expressed as either mean ± SD or percentages, as appropriate. The chi-square test or Fisher’s exact test was used as appropriate to test group differences of proportions.
Results
Hospital A saw 718 patients for a 12-month period, 483 patients were included in the study after applying exclusion criteria ( Table 1 ). The mean age was 60.2 ± 12.3 years, and 264 (54.7%) were men. From these patients, 274 (56.7%) had ETT as first-line investigation and 209 (43.3%) patients had a contraindication to ETT. The average cost per patient in hospital A, calculated based on the NHS tariff, was £566.6 ± 490.0 ($875 ± 758).
| Total Population | Discharged Without Investigation | Inclusive population | CI to ETT | ETT | Age (years) | Male/Female | Average Cost (£) |
|---|---|---|---|---|---|---|---|
| 718 | 235 | 483 | 209 | 274 | 60.2 ±12.3 | 264/219 | 566.6 ±490.0 |
From those who had ETT in hospital A, 151 (55.1%) had negative ETT, 68 (24.8%) had equivocal ETT, and 55 (20.1%) had positive ETT ( Table 2 ). Those with negative ETT did not have any further investigation for CAD. Of the 68 who had equivocal ETT, 65 (95.6%) subsequently had noninvasive investigations (34 CTCA, 6 DSE, and 34 MPS) but only 8 (12.3%) went on to have invasive coronary angiography (ICA), of which 3 (37.5%) had obstructive CAD. Of the 55 patients with positive ETT, 5 (9.1%) had subsequent noninvasive investigation (4 CTCA and 1 MPS) and 53 (96.4%) had ICA, of which 23 (43.4%) had obstructive CAD. From the 209 patients (43.3%) with contraindication to ETT, 156 were classified as low-intermediate likelihood of CAD, of which 149 patients (95.5%) had noninvasive investigations (25 CTCA, 11 DSE, and 113 MPS) and 17 (10.9%) went on to have ICA, from which 6 (35.3%) had obstructive CAD; 53 patients were classified as high likelihood of CAD, of which 9 (17.0%) had noninvasive investigations (2 CTCA, 4 DSE, and 3 MPS) and 49 patients (92.5%) were directly referred for ICA, of which 20 (40.8%) had obstructive CAD.
| Number | Male/Female | Subsequent non-invasive | Had ICA | +ve ICA | Average Cost (£) | |
|---|---|---|---|---|---|---|
| Negative ETT | 151 | 82/69 | 0 | 0 | – | 170 ±0 |
| Equivocal ETT | 68 | 40/28 | 65 | 8 | 3 | 560.5 ±351.5 |
| Positive ETT | 55 | 38/17 | 5 | 53 | 23 | 1384.6 ±190.3 |
| Low/Intermediate Likelihood of CAD | 156 | 73/ 83 | 149 | 17 | 6 | 452.0 ±341.4 |
| High Likelihood of CAD | 53 | 31/22 | 9 | 49 | 20 | 1196 ±269.9 |
Subgroup analysis of patients in hospital A who had noninvasive investigations showed that a total of 65 CTCA were performed, of which 15 (23.1%) had significant stenosis leading to 13 ICA (86.7%) with 4 (30.8%) demonstrating obstructive CAD. The other 2 patients with positive CTCA were investigated with functional tests, and these were negative. A total of 142 MPS were performed, of which 7 (4.9%) were positive and went on to have ICA with 4 (57.1%) showing obstructive CAD.
Hospital B saw 419 patients for a 12-month period, 295 were included in the study after applying exclusion criteria ( Table 3 ). The mean age was 57.5 ± 11.0 years, and 141 (47.8%) were men. The mean PTP RS based on NICE RS was 62.4 ± 24.3%. The average cost per patient in hospital B, based on the NHS Tariff, was £487.9 ± 469.6 ($750 ± 725). From the 295 patients seen in hospital B, 26 (8.8%) with low PTP (mean PTP; 15.1 ± 6.4%) had coronary calcium score in the first instance, 3 (11.5%) of these were positive (>0 calcium score) leading to CTCA, of which 1 demonstrated a moderate stenosis, leading to subsequent noninvasive functional test ( Table 4 ); 98 patients (33.2%) with intermediate PTP (mean PTP; 56.1 ± 16.5%) had CTCA, of which 5 (5.1%) had significant CAD, from which 3 (60%) had subsequent noninvasive functional test and 2 had ICA, of which 1 was found to have obstructive CAD; 77 patients (26.1%) had DSE (mean PTP; 65.1 ± 20.8%), of which all 6 (7.8%) with positive DSE had ICA with 5 (83.3%) having obstructive CAD; 57 patients (19.3%) had MPS (mean PTP; 68.6 ± 19.9%), of which all 11 (19.3%) with a positive MPS had ICA with 7 (63.6%) found to have obstructive CAD.



