Systemic anticoagulation decreases the risk of radial artery occlusion (RAO) after transradial catheterization and standard occlusive hemostasis. We compared the efficacy and safety of provisional heparin use only when the technique of patent hemostasis was not achievable to standard a priori heparin administration after radial sheath introduction. Patients referred for coronary angiography were randomized in 2 groups. In the a priori group, 200 patients received intravenous heparin (50 IU/kg) immediately after sheath insertion. In the provisional group, 200 patients did not receive heparin during the procedure. After sheath removal, hemostasis was obtained using a TR band (Terumo corporation, Tokyo, Japan) with a plethysmography-guided patent hemostasis technique. In the provisional group, no heparin was given if radial artery patency could be obtained and maintained. If radial patency was not achieved, a bolus of heparin (50 IU/kg) was given. Radial artery patency was evaluated at 24 hours (early RAO) and 30 days after the procedure (late RAO) by plethysmography. Patent hemostasis was obtained in 67% in the a priori group and 74% in the provisional group (p = 0.10). Incidence of RAO remained similar in the 2 groups at the early (7.5% vs 7.0%, p = 0.84) and late (4.5% vs 5.0%, p = 0.83) evaluations. Women, patients with diabetes, patients having not received heparin, and patients without radial artery patency during hemostasis had more RAO. By multivariate analysis, patent radial artery during hemostasis (odds ratio [OR] 0.03, 95% confidence interval [CI] 0.004 to 0.28, p = 0.002) and diabetes (OR 11, 95% CI 3 to 38,p <0.0001) were independent predictors of late RAO, whereas heparin was not (OR 0.45 95% CI 0.13 to 1.54, p = 0.20). In conclusion, our results suggest that maintenance of radial artery patency during hemostasis is the most important parameter to decrease the risk of RAO. In selected cases, provisional use of heparin appears feasible and safe when patent hemostasis is maintained.
Systemic anticoagulation decreases the risk of radial artery occlusion (RAO) after transradial catheterization and standard occlusive hemostasis It is currently unknown whether it would be feasible and safe to use a strategy of provisional heparin administration in case of transradial catheterization and patent hemostasis technique. The Provisional Heparin Therapy on Radial Artery Occlusion after Transradial Coronary Angiography and Patent Hemostasis (PHARAOH) study ( NCT01489917 ) compared a strategy of provisional heparin administration only if patent hemostasis was not achievable to standard a priori heparin administration in patients undergoing transradial diagnostic coronary angiography.
Methods
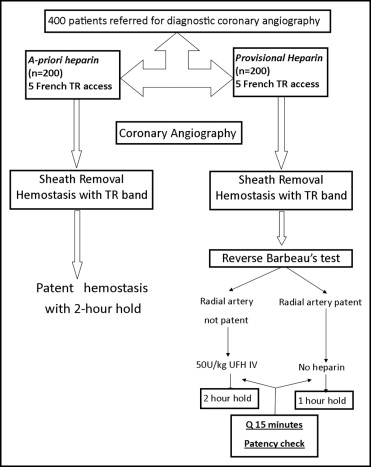
In this prospective randomized study, we enrolled 428 patients referred for elective diagnostic cardiac catheterization. Twenty-eight patients were excluded because of abnormal oxymetry test results bilaterally on preprocedural evaluation. Four hundred patients underwent diagnostic coronary angiography followed by left ventriculography using right transradial access with 5Fr sheaths. Patients were randomized into 2 groups before catheterization. The a priori group included 200 patients who underwent transradial catheterization using a standard heparin administration after radial sheath insertion. The provisional group included 200 patients who underwent transradial catheterization without heparin. The protocol was approved by the institutional review board. All patients provided written informed consent.
In the a priori group, transradial access was obtained with a 20-gauge Teflon-sheathed needle using a counterpuncture technique. A 5Fr introducer sheath (Terumo corporation, Tokyo, Japan) was inserted into the radial artery. A vasodilator cocktail was administered intra-arterially consisting of nitroglycerin 200 μg and diltiazem 5 mg immediately after cannulation of the radial artery. Unfractionated heparin 50 U/kg or a maximum of 5,000 U was administered intravenously after sheath insertion. The 5Fr diagnostic catheters were used to perform coronary arteriography and left ventriculography. The sheath was removed at the end of the procedure, and a TR band (Terumo Medical) was applied. As previously described, the least necessary pressure was applied at the radial artery puncture site to achieve patent hemostasis. After application of the TR band, it was inflated, the introducer was removed, the band was deflated until some pulsatile bleeding was seen at the site, and then the band was reinflated using 1 to 2 ml of air to achieve hemostasis. The band was left in place for 2 hours and not adjusted further unless a patient complained of symptoms or bleeding occurred.
In the provisional group, transradial access and coronary angiography and ventriculography were performed similarly to the a priori group. After sheath removal, the TR band was placed and positioned similarly to the other group. However, in these cases, patency was evaluated at the time of application of the TR band and monitored every 15 minutes afterward until the band was removed and hemostasis completed. After TR band placement, if maintenance of radial artery patency was obtained, no heparin was administered and the TR band was left in place for 1 hour. If radial artery patency was not maintained, a bolus of unfractionated heparin 50 U/kg or a maximum of 5,000 U was administered and the band was left in place for 2 hours. The design of the study is shown in Figure 1 .
Radial artery patency was evaluated using a plethysmographic monitor to detect perfusion in the index finger as previously described. The plethysmographic monitor was placed on the index finger and the radial and ulnar arteries were occluded manually at the level of the wrist joint. After the plethysmographic signal disappeared, the radial artery was released and the ulnar artery was compressed to interrupt ulnar flow. Return of the plethysmographic signal indicated radial artery patency. Absence of return of the plethysmographic signal was a sign of occlusive radial artery hold.
All patients underwent radial artery patency evaluation at 24 hours (early RAO) and 30 days (late RAO) after the procedure. All patients with suspected RAO by plethysmography underwent confirmation with duplex ultrasonography.
Categorical variables were expressed as number and percentage and continuous variable as mean ± SD. Numeric variables were compared using Student’s t test and categorical variables were analyzed using chi-square analysis. Multivariable analysis was performed using logistic regression in the entire cohort of patients to identify predictors of delayed RAO. Age, gender, body surface area, diabetes mellitus, patency during hemostasis, and heparinization were entered in the analysis. Based on our previous experience and recent data evaluating acute and late RAOs, we assumed that a sample size of ≥400 patients would be adequate to detect a 20% difference between the 2 groups with a power of 80% at the 0.05 level. Statistical analysis was performed using SPSS 15.0 (SPSS, Inc., Chicago, Illinois). A p value <0.05 was considered statistically significant.
Results
Demographic and procedural data are listed in Table 1 . There were no statistically significant differences between the 2 groups. After radial sheath removal, patent hemostasis was feasible in 134 patients (67%) in the a priori group and in 149 patients (74%) in the provisional group (p = 0.10). Therefore, in the provisional group heparin was required in 26% of cases. All procedures lasted <20 minutes. As shown in Figure 2 , early RAO occurred in 15 patients (7.5%) in the a priori group compared to 14 patients (7.0%) in the provisional group (p = 0.84). Late RAO occurred in 9 patients (4.5%) in the a priori group compared to 10 patients (5.0%) in the provisional group (p = 0.83). In the a priori group, 1 patient developed RAO despite patent hemostasis at the outset. In contrast, in the provisional group, no patient with patency maintained during hemostasis developed RAO. In the entire study population, RAO at 30 days occurred more frequently in women (6.5% in women vs 3% in men, p = 0.006), patients with diabetes (2% in nondiabetics vs 7.5% in diabetics, p = 0.001), patients having not received heparin (6% in those who did not receive heparin vs 3.9% in those who received heparin, p = 0.0001), and patients without radial artery patency during hemostasis (9% in those without patency vs 0.5% in those with patency, p = 0.0001). Age, height, weight, history of hypertension, and procedure duration had no significant interaction with RAO. By multivariate analysis, patent radial artery (odds ratio [OR] 0.03, 95% confidence interval [CI] 0.004 to 0.28, p = 0.002) and diabetes (OR 11, 95% CI 3 to 38, p <0.0001) were independent predictors of late RAO, whereas heparin was not (OR 0.45, 95% CI 0.13 to 1.54, p = 0.20).
| Variables | Heparin | p Value | |
|---|---|---|---|
| A Priori | Provisional | ||
| (n = 200) | (n = 200) | ||
| Age (years) | 63 ± 12 | 64 ± 12 | 0.21 |
| Men | 64% | 61% | 0.27 |
| Weight (kg) | 92 ± 23 | 90 ± 22 | 0.48 |
| Diabetes mellitus | 29% | 23% | 0.13 |
| Hypertension treatment | 83% | 84% | 0.50 |
| Aspirin pretreatment | 97 (43%) | 92 (41%) | 0.34 |
| Clopidogrel pretreatment | 24 (12%) | 30 (15%) | 0.23 |
| Patients with heparin | 100% | 26% | 0.0001 |
| Procedure duration (minutes) | 9.8 ± 2.7 | 9.6 ± 2.7 | 0.54 |
| Total nursing time (minutes) | 15 ± 0.3 | 22 ± 0.2 | 0.0008 |
| Initial radial artery patency | 67% | 74% | 0.10 |
| Early radial artery occlusion | 7.5% | 7.0% | 0.84 |
| Late radial artery occlusion | 4.5% | 5.0% | 0.83 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


