1. How common is cocaine use in the United States?
Cocaine is the second most commonly used illicit drug in the United States, with only marijuana being used more often. Between 1994 and 1998, the number of new cocaine users per year increased by 82%. In 2005, there were approximately 450,000 cocaine-related emergency department visits in the United States. In 2007, there were 2.1 million cocaine users age 12 or older, comprising 0.8% of the population. Users are more likely to be young, between 18 and 20 years of age. Males are more likely to be users than females by a 2:1 ratio. Cocaine-associated chest pain accounts for approximately 16% of all cocaine-related admissions, leading to the evaluation of approximately 64,000 patients annually. Of these, approximately 57% are admitted to the hospital for further evaluation.
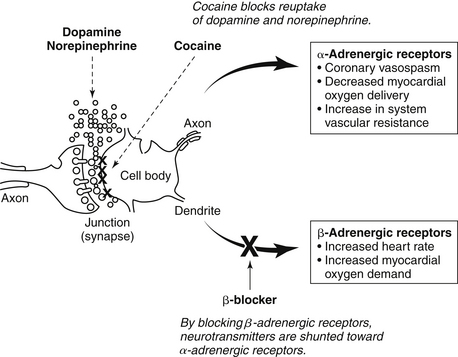
2. What are the pharmacologic effects of cocaine?
Cocaine is a powerful sympathomimetic that acts by directly stimulating central sympathetic outflow and blocking presynaptic uptake of norepinephrine and dopamine (Fig. 49-1). This augmentation in postsynaptic catecholamines increases heart rate, mean arterial pressure, and left-ventricular contractility through stimulation of both α- and β-adrenergic receptors. Through enhanced α-adrenergic receptor activation, increased endothelin production, and diminished nitric oxide generation, cocaine initiates coronary artery vasoconstriction. Cocaine may also enhance platelet aggregation and thrombus formation through heightened production of adenosine diphosphate, thromboxane A2, and tissue plasminogen activator inhibitors, as well as reductions in protein C and antithrombin III. Cocaine causes toxic effects on cardiac muscle that arise primarily from Ca2+ overload during excessive β-adrenergic stimulation. Cocaine is well absorbed through all body mucous membranes and can be administered by nasal, sublingual, intramuscular, intravenous, and respiratory routes. The onset of action varies from 3 seconds to 5 minutes, depending on the administration route.
3. What are the typical symptoms after cocaine ingestion?
Cardiopulmonary complaints are the most commonly reported symptoms in patients after cocaine use, occurring in 56% of cases. Chest pain is the most common symptom and is typically described as a pressure sensation. Other common symptoms include dyspnea, anxiety, palpitations, syncope, dizziness, and nausea. The onset of symptoms usually occurs soon after ingestion, with two-thirds of patients presenting within 3 hours.
4. What are the consequences of cocaine use?
The cardiac and systemic effects of cocaine are complex. Cocaine-induced increase in sympathomimetic activity results in increased myocardial contractility, heart rate, blood pressure, and increased myocardial oxygen demand, while simultaneously decreasing myocardial oxygen supply due to vasoconstriction leading to hypertensive crises, acute myocardial infarction (AMI), aortic dissection, and stroke. Premature coronary atherosclerosis has been seen in young cocaine abusers, with obstructive coronary artery disease (CAD) seen in 35% to 40% of patients who undergo angiography for cocaine-associated chest pain. Cocaine may depress left ventricular function in the absence of acute coronary ischemia because of its direct negative inotropic effect on cardiac muscle, therefore leading to myocarditis and cardiomyopathy. Cocaine exhibits properties of a class I antiarrhythmic agent by Na-channel blockade. It also prolongs the duration of the QT interval by inhibiting myocyte repolarization that occurs by the efflux of potassium. Cocaine also increases intracellular calcium with resultant afterdepolarizations, reduces vagal activity, and increases myocyte irritability by inducing ischemia. Ischemia due to vasospasm and fatal ventricular arrhythmias due to ischemia are presumed to be important mechanisms of sudden death in these patients.
5. How often does AMI occur after cocaine ingestion?
Reported rates of AMI vary widely (1% to 31%); the variance in the incidence of AMI in studies likely relates to the difference in patient populations, AMI diagnostic criteria, and the use of newer, more sensitive troponin assays that can detect smaller levels of myocardial necrosis in patients that were previously classified as unstable angina. AMI occurs within minutes to days after cocaine exposure, independent of dose, length of use, or route of administration. However, the time during which individuals are at higher risk for developing AMI is within the first hour of cocaine use.
6. What else should be considered in the differential diagnosis after cocaine use?
Because patients who present to the emergency department after cocaine use are commonly hypertensive and tachycardic, aortic dissection needs to be considered in the differential diagnosis. Information concerning cocaine-induced aortic dissection is limited, but one study of 38 consecutive cases of aortic dissection demonstrated that a surprisingly high number (14, or 37%) were associated with cocaine use. However, among 921 patients in the International Registry of Aortic Dissection (IRAD), only 0.5% of aortic dissection cases were associated with cocaine use. In addition, an acute pulmonary syndrome, “crack lung,”
Only gold members can continue reading.
Log In or
Register to continue
Related

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree