14 Coarctation of the Aorta
I. CASE
A. Fetal echocardiography findings
1. The fetal echo reveals situs solitus of the atria, levocardia, left aortic arch, heart rate 145 bpm, and a normal cardiothoracic ratio (0.3).
2. The RV is enlarged. The LV has relative hypoplasia but normal length.
3. The aortic valve is bicuspid, with mildly hypoplastic annulus (3.5 mm) but without significant aortic stenosis (velocity 1.5 m/s). There is neither mitral nor aortic valve regurgitation.
4. There is no significant poststenotic dilation of the ascending aorta, but there is mild isthmal hypoplasia (2.5 mm).
5. The RV is moderately dilated, with normal tricuspid and pulmonary artery flow.
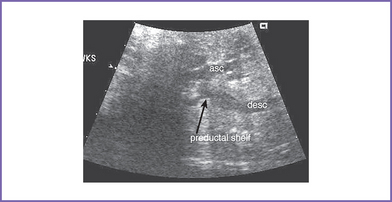
6. Flow in both the aortic and ductal arches is normal and antegrade. The aortic arch, however, is hypoplastic distally between the left common carotid artery and the descending aorta. There appears to be a posterior shelf consistent with coarctation of the aorta (CoA) (Fig. 14-1).
7. There is an unrestricted right-to-left shunt across the foramen ovale.
8. The RV Tei index (myocardial performance index) is mildly increased at 0.50. The LV Tei index is normal.
D. Fetal management and counseling
1. Ultrasound plus amniocentesis with karyotyping for chromosomal anomalies.
c. Fluorescent in situ hybridization (FISH) screen for chromosome 22q11 microdeletion.
2. Follow-up includes serial antenatal fetal echocardiography studies at 4-week intervals.
a. Size and function of the LV (apex forming).
b. Diameters of the mitral and aortic valves and the presence of subaortic stenosis. Assessment of valve morphology might become easier later in gestation.
c. Size of the transverse aortic arch compared to the ductus.
d. Size and direction of flow across the foramen ovale. Right-to-left flow is normal in the fetus.
e. Size and direction of flow through the distal aortic arch.
f. The patency of the ductus arteriosus. Any constriction of the ductus in late gestation could lead to heart failure and fetal death.
g. The flow pattern in the pulmonary veins, especially diastolic a wave reversal as an indirect measure of increased pressure in the LA.
h. Missed ventricular septal defect (VSD), which is common in the context of aortic CoA.
i. Development of heart failure (rare).
F. Neonatal management
a. Following delivery of a baby with a prenatal diagnosis of probable CoA, prostaglandin E1 (PGE1) may be initiated if the coarctation is clearly more severe, with significant arch hypoplasia, or if there is a concern that the left heart size may be borderline, particularly if there is retrograde distal arch flow.
b. Otherwise, many cases of prenatally diagnosed CoA might not be ductus arteriosus dependent and may not require surgical correction in the neonatal period.
c. Lack of blood pressure differences while the ductus arteriosus is still patent is the norm because the ductus arteriosus may be providing critical blood flow to the lower body beyond the level of the coarctation.
d. The hyperoxia test should be performed in either case because it can provide useful physiologic data that can help in appropriately managing the infant.
e. In critical neonatal CoA, the ductus arteriosus often supplies blood flow to the distal arch. The hyperoxia test would in such a state reveal a normal Pao2 (>250 mm Hg) in the preductal area, whereas the postductal area will fail the hyperoxia test as a result of right-to-left shunting through the ductus arteriosus. Occasionally, where there is a discrete coarctation, the baby passes preductal and postductal hyperoxia tests.
f. The two-dimensional echocardiogram shows the site and extent of coarctation. The Doppler examination reveals a disturbed flow distal to the coarctation and signs of delayed emptying in the proximal descending aorta, with continuous flow through the distal arch beginning at the most proximal point of significant arch hypoplasia or obstruction. In the presence of a patent ductus, there is usually no gradient across the coarctation.
g. In borderline situations, or when the infant passes the hyperoxia test and there is still suspicion of coarctation, the ductus could be allowed to close while the vital signs and blood pressures are monitored in the intensive care unit, with follow-up echocardiography to confirm the diagnosis. Ductal constriction can result in a discrete shelf’s evolving at the site of the distal arch where the ductus joins the aorta. This type of coarctation can continue to evolve even weeks to months beyond the neonatal period.
a. The surgical procedure of choice varies from institution to institution.
b. The appropriate surgical procedure also is determined by the type of coarctation, whether there is significant proximal arch hypoplasia or only a discrete contraductal shelf.
c. Transcatheter intervention.
d. Balloon angioplasty or stenting is the treatment of choice for recurrent coarctation, and in some institutions it is used more routinely for discrete native coarctation identified in older infants and children.
G. Follow-up
1. Most patients are hospitalized for 5 to 10 days after surgery for coarctation.
2. Reexamination is necessary every 6 to 12 months because residual obstruction and/or recoarctation occur in 20% to 25% of the patients who had the repair as neonates or young infants.
3. Subacute bacterial endocarditis (SBE) prophylaxis should be continued on indications because of frequently associated bicuspid aortic valve and residual coarctation.
4. Yearly surveillance by clinical examination, echocardiography, and cardiac magnetic resonance imaging (MRI) is necessary. This surveillance monitors persistent systemic hypertension due to residual narrowing proximal to the arch repair and development of an aneurysm of the aorta near the site of repair.
5. Reassessment for subvalvar and valvar aortic stenosis or mitral stenosis should be performed at follow-up, given the common association and their progressive nature, particularly in the first few years of life.
6. Late repair of coarctation is associated with sudden intracranial bleeding from berry aneurysm in the brain.
I. Outcome of this case
1. The baby was delivered at term weighing 2.3 kg. Apgar scores were 8 at 1 minute and 9 at 5 minutes.
2. The baby passed the preductal hyperoxia test with a Pao2 of 275 mm Hg, but the postductal Pao2 was 80 mm Hg, suggesting significant right-to-left shunting through the ductus arteriosus and a critical coarctation.
3. PGE1 infusion was started at 0.0125 μg/kg per minute.
a. A low dose should be used here, given the prenatal diagnosis and because closure, even with a dose as low as 0.005 μg/kg per minute, is extremely unusual in a newborn just delivered.
b. The PDA responded well to PGE1.
4. The aortic valve annulus (4 mm) with antegrade flow and LV size (LV:RV length ratio was 0.8) was considered borderline but apex forming.
5. There were two surgical options: a univentricular repair (Norwood stage 1 with arch reconstruction) or biventricular repair only addressing the transverse arch hypoplasia.
a. The baby had arch reconstruction with pulmonary homograft and division of the patent ductus arteriosus at 1 week of age.
b. He was discharged on PO digoxin and furosemide at 2 weeks of age.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree