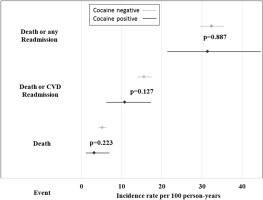
Although cocaine is a well-recognized risk factor for coronary disease, detailed information is lacking regarding related behavioral and clinical features of cocaine-associated ST-segment elevation myocardial infarction (STEMI), particularly in socioeconomically disadvantaged urban settings. Nor are systematic or extended follow-up data available on outcomes for cocaine-associated STEMI in the contemporary era of percutaneous coronary intervention. We leveraged a prospective STEMI registry from a large health system serving an inner-city community to characterize the clinical features, acute management, and middle-term outcomes of cocaine-related versus cocaine-unrelated STEMI. Of the 1,003 patients included, 60% were black or Hispanic. Compared with cocaine-unrelated STEMI, cocaine-related STEMI (n = 58) was associated with younger age, male gender, lower socioeconomic score, current smoking, high alcohol consumption, and human immunodeficiency virus seropositivity but less commonly with diabetes or hypertension. Cocaine users less often received drug-eluting stents or β blockers at discharge. During median follow-up of 2.7 years, rates of death, death or any rehospitalization, and death or cardiovascular rehospitalization did not differ significantly between cocaine users and nonusers but were especially high for death or any hospitalization in the 2 groups (31.4 vs 32.4 per 100 person-years, p = 0.887). Adjusted hazard ratios for outcomes were likewise not significantly different. In conclusion, in this low-income community, cocaine use occurred in a substantial fraction of STEMI cases, who were younger than their nonuser counterparts but had more prevalent high-risk habits and exhibited similarly high rates of adverse outcomes. These data suggest that programs targeting cocaine abuse and related behaviors could contribute importantly to disease prevention in disadvantaged communities.
Graphical abstract
Cocaine accounts for >⅕ of the nearly 2.5 million annual visits to emergency departments for drug misuse or abuse in the United States. Acute and chronic ingestion of cocaine is closely linked to onset of acute coronary syndromes. Various pharmacologic effects of cocaine underlie this association, including vasoconstriction, proatherogenic and prothrombotic effects, β-adrenergic stimulation, and direct myocardial depression. Much of the early work characterizing the cardiovascular complications of cocaine use was performed in people presenting to emergency departments with chest pain. More recent reports have described the acute features and inhospital outcomes of cocaine-related acute coronary syndromes who underwent percutaneous coronary intervention (PCI). But information is lacking on related social or behavioral characteristics, such as broad-based measures of socioeconomic status or alcohol use, or clinical conditions, such as human immunodeficiency virus (HIV) infection, particularly in minority inner-city populations. Furthermore, scant data are available regarding post-discharge outcomes for acute myocardial infarction. Some studies have reported high cocaine-associated rates of in-stent thrombosis during short-term follow-up after PCI, but long-term readmissions, cardiovascular events, and mortality have to our knowledge not been assessed. We parlayed data from an inner city health system’s registry of ST-segment elevation myocardial infarction (STEMI) to address these gaps by focusing on 2 specific objectives: (1) to characterize the distinguishing sociobehavioral, clinical, and acute care features of cocaine users and nonusers presenting with STEMI and (2) to assess the impact of a history of cocaine use on middle-term outcomes after STEMI in this low-income population.
Methods
The Montefiore ST-Segment Elevation Myocardial Infarction registry is a prospective cohort initiated in May 2008 comprising all patients considered for primary revascularization of STEMI at the Montefiore Medical Center’s (MMC) 2 main hospitals, Moses and Weiler. Only patients presenting with new-onset STEMI in the ambulatory setting were included; inpatients who developed STEMI during hospitalization were ineligible. The registry was originally formed with the intent of evaluating hyperglycemia management strategies in the acute STEMI setting. After 2009, the registry was expanded to collect information on all STEMIs. Trained physician and nurse abstractors collected clinical, laboratory, and procedural information on all patients referred for cardiac catheterization for STEMI during hospitalization. The study was approved by the Institutional Review Board of the Albert Einstein College of Medicine and, for the purpose of collecting rehospitalization data, the North Bronx Health Network (NBHN). The current report includes patients through December 2013.
Eligible patients were those with symptoms of coronary ischemia lasting ≥20 minutes, demonstrating ST-segment elevation of ≥2 mm (women ≥1.5 mm) in V2-V3 or ≥1 mm in ≥2 other contiguous leads, or new left bundle branch block, and elevation in circulating cardiac troponin T (TnT) or creatine kinase-MB mass >99th percentile of the upper reference limit. In the absence of appropriate cardiac biomarker measurement, clinical symptoms, diagnostic electrocardiographic changes, and angiographic findings consistent with acute atherothrombosis or segmental wall motion abnormalities on cardiac imaging were used as criteria for inclusion.
Exclusion criteria comprised history of chronic renal replacement therapy, acute diabetic ketoacidosis, and pregnancy. In addition, cardiogenic shock was excluded in 2008 and 2009 but not thereafter. Of all patients entered in the registry by nurse abstractors (n = 1,039), review of hospital records by 3 cardiologists (VS, JS, and JRK) resulted in exclusion of 33 ineligible patients, along with 3 who refused consent, leaving a sample of 1,003 for analysis.
Information collected by nurse abstractors on clinical, laboratory, and imaging data was supplemented using Looking Glass Clinical Analytics (LGCA) (Streamline Health, Atlanta, Georgia). LGCA is an interactive software application in use across the Montefiore Health System, which integrates clinical and administrative data to allow evaluation of health care quality. Where missing data on clinical characteristics was not directly queriable by LGCA, trained physician abstractors (SGS, NK, and VA) undertook direct review of electronic medical records. Cardiac catheterization data were obtained from an electronic database containing standardized angiographic and procedural information reported to New York State. Mortality data were obtained by linkage to the National Death Index. LGCA was also used to capture rehospitalizations at MMC after the index STEMI hospitalization. Because NBHN is a common source of STEMI referrals to MMC (n = 83 patients in the registry), we supplemented information on rehospitalizations by cross-linking to NBHN electronic medical records.
“Cocaine-associated STEMI” was defined by history of cocaine use within 4 weeks of presentation or by a positive cocaine urine test. When the urine test was positive, we considered the patient to be an “active cocaine user,” regardless of history. In the presence of a positive history, the history trumped the urine cocaine test result. The MMC laboratory tests for cocaine metabolite in the urine with the EMTII PLUS d.a.u. Cocaine metabolite assay (GMI, Inc., Ramsey, Minnesota). The assay measures benzoylecgonine, the major metabolite of cocaine, which can be detected within 4 hours of cocaine use and can remain detectable in concentrations >100 ng/ml for as long as 48 hours. The cutoff for “positive urine toxicology” was the recommended value of 300 ng/ml. We defined “cocaine use as negative” based on history of no cocaine or drug use, in conjunction with lack of urine testing or a negative result thereof.
The primary outcome measures were death, death and rehospitalization for any cause, and death and rehospitalization for CVD, ascertained through 2013. Rehospitalization was defined as any hospital admission lasting ≥24 hours. Rehospitalizations were limited to MMC and NBHN, which together account for a majority of health care delivery for the Bronx, New York, and its vicinity. CVD rehospitalizations were defined by discharge diagnosis, using International Classification of Diseases, Ninth Revision , or Current Procedural Terminology , Fourth Edition , codes consistent with coronary heart disease (angina pectoris, myocardial infarction, PCI, or coronary artery bypass grafting), heart failure, stroke, atrial fibrillation or flutter, or ventricular tachycardia or fibrillation. For coronary heart disease, heart failure, stroke, and cardiac dysrhythmias, these needed to be in the primary position. Comprehensive nationwide information on deaths was available from the National Death Index through 2013.
Race and ethnicity were defined by self-report. Summary socioeconomic score was calculated according to previously reported methods. Hypertension was defined by history or treatment with antihypertensive medication. Diabetes was defined by history or use of antidiabetic medication. Dyslipidemia was defined by history or use of lipid-lowering therapy. Current smoking was defined as self-reported smoking of at least 1 cigarette in the past month. Heavy alcohol use was defined as >14 drinks a week for men and >7 drinks a week for women or history of alcohol abuse. Previous CVD was defined as history of coronary heart disease, stroke, or heart failure. HIV seropositivity was based on a positive HIV test by Western blot or detectable circulating viral RNA copies on querying of MMC laboratory test results back to 1997 (earliest available). Left ventricular ejection fraction was obtained from ventriculography when available (n = 767) or echocardiography otherwise (n = 219). Critical coronary artery narrowing was defined by the presence of a ≥70% stenosis in at least 1 vessel in the distribution of the left anterior descending, left circumflex or right coronary artery, or of a ≥50% stenosis in the left main coronary artery. Door-to-balloon time was recorded by cardiac catheterization nursing staff as the period from first medical contact to balloon inflation and provided for nontransfer patients who underwent PCI within 24 hours of first medical contact (n = 622).
Categorical variables are expressed as counts (%) and continuous variables as medians (interquartile range). Follow-up time was defined as time to the event of interest or through December 2013, whichever occurred earlier. Average incidence rates were calculated as the number of events divided by follow-up time in cocaine users and nonusers, and differences computed with Poisson 95% confidence intervals. Cox models were used to compare time to events post-STEMI for cocaine users and nonusers after adjusting for relevant covariates. We considered for adjustment covariates previously documented as risk factors for outcomes after STEMI, including sociodemographic variables, cardiovascular risk factors, STEMI-associated variables, acute care variables, and discharge medications. From candidate covariates, those associated with outcome at p <0.25 were initially selected. To construct a parsimonious model, only covariates whose inclusion altered the hazard ratio by ≥10% were retained. The proportional hazards assumption was tested by Schoenfeld residuals, which revealed no violations. Analyses were performed with SAS, v. 9.4. (Cary, North Carolina). Two-tailed p <0.05 defined statistical significance.
Results
Baseline clinical, laboratory, and imaging characteristics of the study cohort, both overall and by cocaine-use status, are presented in Table 1 . The study cohort was middle-aged to older, mostly men and of black or Hispanic race-ethnicity, and exhibited a low summary socioeconomic score. Traditional CVD risk factors were common, a substantial proportion of patients had previous CVD, and a small minority was known to be infected with HIV. ST-segment elevation was more frequently inferior or anterior than lateral in location; a substantial minority of patients presented in cardiogenic shock. A subset of patients did not undergo cardiac catheterization within 24 hours; reasons included death before catheterization, patient refusal, medical contraindications (sepsis, acute hemorrhage, advanced renal insufficiency with patient unwillingness to receive dialysis), and serious or terminal medical illness (cardiac arrest with anoxic brain injury, advanced dementia, end-stage cancer).
| Variable | Entire cohort (n=1003) | Cocaine positive (n=58) | Cocaine negative (n=945) | p value |
|---|---|---|---|---|
| Age (years) | 59 (50, 69) | 51 (44, 57) | 60 (51, 70) | <.001 |
| Women | 327 (33%) | 12 (21%) | 315 (33%) | 0.040 |
| Race-ethnicity | 0.100 | |||
| Non-Hispanic white | 210 (21%) | 8 (14%) | 202 (21%) | |
| Non-Hispanic black | 197 (20%) | 16 (28%) | 181 (19%) | |
| Hispanic | 404 (40%) | 28 (48%) | 376 (40%) | |
| Other | 192 (19%) | 6 (10%) | 186 (20%) | |
| Summary socioeconomic score | -2.2 (-5.3, -0.7) | -3.6 (-6.5, -1.1) | -2.1 (-5.3, -0.7) | 0.007 |
| Body mass index (kg/m 2 ) | 28.2 (25.1, 31.5) | 29 (25.7, 33.3) | 28.1 (25, 31.5) | 0.233 |
| Systolic blood pressure (mm Hg) | 136 (117, 155) | 135 (116, 150) | 137 (117, 156) | 0.517 |
| Diastolic blood pressure (mm Hg) | 80 (68, 93) | 79 (68, 91) | 80 (68, 93) | 0.643 |
| Heart rate (beats per minute) | 79 (68, 90) | 79 (66, 88) | 79 (69, 90) | 0.589 |
| Hypertension | 663 (66%) | 27 (47%) | 636 (67%) | 0.001 |
| Diabetes mellitus | 357 (36%) | 13 (22%) | 344 (36%) | 0.030 |
| Dyslipidemia | 533 (53%) | 28 (48%) | 505 (53%) | 0.444 |
| Current smoking | 390 (39%) | 45 (78%) | 345 (37%) | <.001 |
| Heavy alcohol use | 106 (11%) | 16 (28%) | 90 (10%) | <.001 |
| Family history of CHD | 313 (32%) | 20 (36%) | 293 (31%) | 0.483 |
| Prior CVD | 206 (21%) | 12 (21%) | 194 (21%) | 0.977 |
| HIV infection | 26 (3%) | 6 (10%) | 20 (2%) | 0.001 |
| Infarct location on ECG | 0.366 | |||
| Anterior | 494 (49%) | 24 (41%) | 470 (50%) | |
| Inferior | 451 (45%) | 29 (50%) | 422 (45%) | |
| Lateral | 39 (4%) | 4 (7%) | 35 (4%) | |
| LBBB | 19 (2%) | 1 (2%) | 18 (2%) | |
| Non-sinus rhythm | 39 (4%) | 3 (5%) | 36 (4%) | 0.489 |
| Killip class | 0.159 | |||
| I | 846 (84%) | 49 (85%) | 797 (84%) | |
| II | 43 (4%) | 3 (5%) | 40 (4%) | |
| III | 31 (3%) | 4 (7%) | 27 (3%) | |
| IV | 83 (8%) | 2 (4%) | 81 (9%) | |
| TIMI STEMI score | 3 (2, 5) | 2 (1, 3) | 3 (2, 5) | 0.001 |
| Initial hemoglobin A1c (%) | 6.0 (5.7, 7.8) | 6.0 (5.6, 7.8) | 6.0 (5.7, 7.8) | 0.621 |
| Peak creatine kinase (u/l) | 1485 (655, 3024) | 1640 (692, 2495) | 1459 (655, 3042) | 0.894 |
| Peak creatine kinase-MB (u/l) | 122 (47, 221) | 145 (69, 254) | 121 (47, 217) | 0.237 |
| Peak troponin T (ng/ml) | 4.3 (1.9, 8.5) | 5.5 (2, 8.5) | 4.3 (1.9, 8.4) | 0.531 |
| Initial serum creatinine (mg/dl) | 1 (0.8, 1.2) | 1 (0.9, 1.3) | 0.9 (0.8, 1.2) | 0.070 |
| Catheterized within 24 hours | 944 (94%) | 52 (90%) | 892 (94%) | 0.145 |
| Culprit coronary artery ∗ , † | 0.394 | |||
| Left anterior descending ‡ | 434 (46%) | 20 (38%) | 414 (47%) | |
| Left circumflex | 102 (11%) | 5 (10%) | 97 (11%) | |
| Right coronary artery | 402 (43%) | 27 (52%) | 375 (42%) | |
| No. critically narrowed coronary arteries ∗ | 0.525 | |||
| 0 | 100 (11%) | 4 (8%) | 96 (11%) | |
| 1 | 412 (44%) | 27 (52%) | 385 (43%) | |
| 2 | 265 (28%) | 15 (29%) | 250 (28%) | |
| 3 | 167 (18%) | 6 (12%) | 161 (18%) | |
| Left ventricular ejection fraction (%) | 50 (40, 60) | 51 (35, 59) | 50 (40, 60) | 0.823 |
∗ Only for those with catheterization performed within 24 hours.
† Excludes n = 6 patients with undetermined culprit artery in the cocaine-negative group.
‡ Includes n = 2 with culprit left main disease in the cocaine-negative group.
Nearly 6% of patients were active cocaine users, either by history or positive urine testing. Urine testing was performed in 246 patients and was positive in 28 (11.4%). As listed in Table 1 , cocaine users with STEMI were younger and less often women, with a lower summary socioeconomic score than cocaine nonusers. Compared with cocaine nonusers, cocaine users had lower prevalences of hypertension and diabetes but were more than twice as commonly current smokers, almost threefold as frequently heavy consumers of alcohol, and about 5 times as commonly known to be infected with HIV.
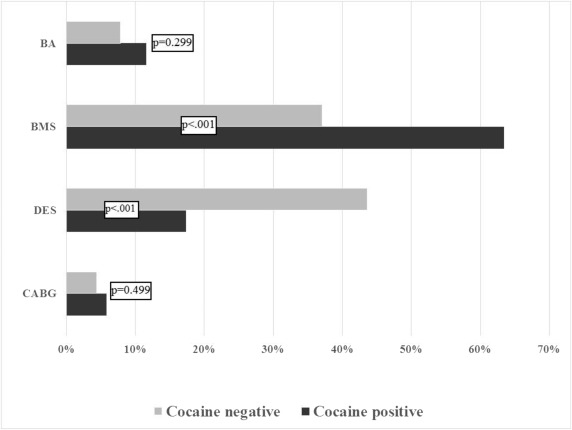
Among patients who received cardiac catheterization within 24 hours of admission, 88.7% underwent PCI and 4.5% underwent coronary artery bypass grafting. Median door-to-balloon time for nontransfers was 72 minutes (interquartile range 54 to 90) and did not differ significantly between cocaine users and nonusers (69 vs 72 minutes, p = 0.127). Comparison of the proportions of cocaine users and nonusers who did not have any critically narrowed coronary arteries, as a surrogate for potential vasospasm, revealed no significant difference between the groups ( Table 1 ). As shown in Figure 1 , cocaine users received bare metal stents almost twice as commonly as nonusers. Conversely, drug-eluting stents were deployed over twofold more frequently in cocaine nonusers versus users. High proportions of patients were discharged on recommended pharmacotherapies. Figure 2 shows that major classes of discharge medications were similar in cocaine users and nonusers, although β blockers were significantly less common in the former group.