5
Clinical Indications and Quality Assurance
APPROACH TO THE DIAGNOSTIC USE OF ECHOCARDIOGRAPHY
DEFINITIONS AND CLASSIFICATION OF ECHOCARDIOGRAPHIC STUDIES
TRANSTHORACIC ECHOCARDIOGRAPHY
TRANSESOPHAGEAL ECHOCARDIOGRAPHY
IMAGE AND DOPPLER DATA STORAGE
QUALITY ASSURANCE IN ECHOCARDIOGRAPHY
DIFFERENTIAL DIAGNOSIS FLOW CHARTS
Approach to the Diagnostic Use of Echocardiography
Reliability of a Diagnostic Test
Accuracy
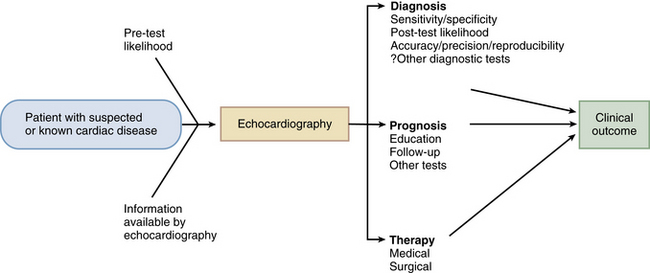
For echocardiographic diagnoses that are either present or absent (called categorical variables), accuracy reflects the certainty with which a specific diagnosis can be confirmed or excluded based on the test results (Fig. 5-1). An example is echocardiography for the diagnosis of endocarditis: the patient either has or does not have endocarditis; there is no range of values. Accuracy for this type of test is described in terms of sensitivity and specificity. The sensitivity of a test is the degree to which it identifies all patients with the disease; specificity is the degree to which a test identifies all patients without the disease.
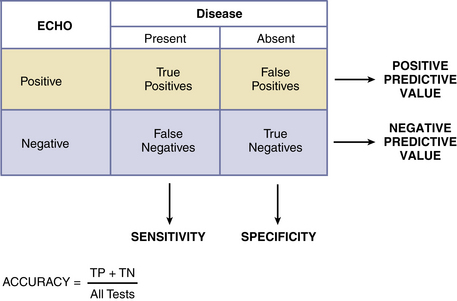
Figure 5–1 Sensitivity and specificity in comparison with positive and negative predictive value.
Note that predictive values are dependent on the prevalence of the disease in the study population and thus cannot be extrapolated to other patient groups (TP, true positives; TN, true negatives).
 Sensitivity = “true-positive” tests/all patients with the disease
Sensitivity = “true-positive” tests/all patients with the disease
 Specificity = “true-negative” tests/all patients without the disease
Specificity = “true-negative” tests/all patients without the disease
The relationship between sensitivity and specificity can be evaluated quantitatively for any given diagnostic test by graphing the sensitivity (y-axis) versus 1 − specificity (x-axis), with each point on the curve representing a different breakpoint defining the test as abnormal. The area under the curve reflects the clinical value of the test, with a larger area indicating a more reliable diagnostic test. The point on the receiver-operator curve, where sensitivity and specificity are maximized, indicates an appropriate breakpoint (Fig. 5-2).
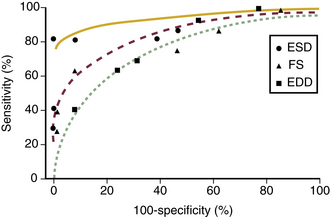
Figure 5–2 Receiver-operator curve of sensitivity versus (1 − specificity).
LV contractility was determined in a series of patients with chronic severe mitral regurgitation by measurement of elastance (Emax). The clinical value of echocardiographic LV end-diastolic dimension (EDD), end-systolic dimension (ESD), and fractional shortening (FS) for identification of impaired contractility is shown using receiver operator curves. An LV-ESD of 40 mm had the best sensitivity (82%) and specificity (100%) for prediction of impaired contractility, defined by reduced elastance. (From Flemming MA, Oral H, Rothman ED, et al: Echocardiographic markers for mitral valve surgery to preserve left ventricular performance in mitral regurgitation. Am Heart J 140:476-482, 2000.)
Precision
The reproducibility of echocardiographic imaging and Doppler data is affected by variability in:
In addition, variability can occur both when the same person repeats the data acquisition or measurement at a different time (intraobserver variability) and when data acquisition or measurement is performed by different people (interobserver variability). These sources of imprecision are a major limitation of echocardiography in clinical practice. There are several approaches to improving the precision, and thus reliability, of echocardiographic data. Appropriate training and experience help ensure correct acquisition of data, including correctly aligned image planes and Doppler recordings, optimization of instrument parameters, and standardized study protocols. Measurement precision is improved with adherence to published standards, quality control in each laboratory, and comparison with reference standards when possible. Interpretation variability is minimized by using standard terminology and diagnostic criteria, developing a consensus approach to reporting in each laboratory, and comparing images and Doppler data to previous recordings in that patient whenever possible; that is, the report should specify whether there is a change from previous studies based on direct comparison of the recorded data, with side-by-side measurements as needed. Measurement variability is reported in each chapter when this information is available.
Integration of Clinical Data and Test Results
 Positive predictive value = true positives divided by all positives
Positive predictive value = true positives divided by all positives
 Negative predictive value = true negatives divided by all negatives
Negative predictive value = true negatives divided by all negatives
Likelihood Ratio
or
A positive likelihood ratio >10 indicates an excellent test, and 5-10 indicates a good test.
The likelihood ratio for a negative test result is calculated as:
or
Pre- and Post-Test Probability
Another approach to the use of sensitivity- specificity data in patient management is to consider relevant clinical data along with the test result (Fig. 5-3). The value of a diagnostic test increases when the pre-test likelihood of disease is integrated with the test results to derive a post-test likelihood of disease. This approach is known as Bayesian analysis. For example, the pre-test likelihood of severe aortic stenosis in an asymptomatic 30-year-old woman without a systolic murmur is very low. An echocardiogram purporting to show severe aortic stenosis most likely is an erroneous interpretation (a false-positive test result). In this setting, the result does not increase the post-test likelihood of disease very much. In contrast, in an elderly man with a 4/6 aortic stenosis murmur and symptoms of angina, syncope, and heart failure, the diagnosis of severe valvular aortic stenosis can be made with a high level of certainty even before any test is performed. The echocardiogram serves only to confirm the diagnosis and define the severity of obstruction. In general, diagnostic tests are most helpful when the pre-test likelihood of disease is intermediate so that the test result will substantially change the post-test likelihood of disease.
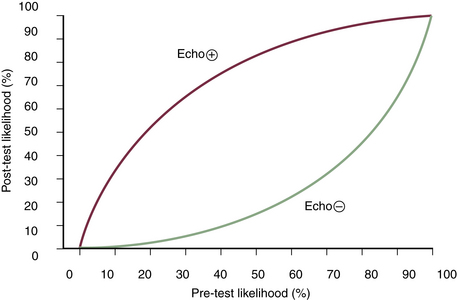
Figure 5–3 Bayesian analysis.
The pre-test and post-test likelihood of coronary artery disease in patients undergoing exercise echocardiography are shown for inducible ischemia (+echo) or a normal result (−echo). These curves were generated based on a sensitivity of 85% and a specificity of 82% of exercise echocardiography for diagnosis of significant (>70% luminal narrowing) coronary artery disease. In clinical practice, the pre-test likelihood is based on the patient’s clinical history, age, and gender. The post-test likelihood then depends on the result of the exercise echocardiogram. For example, if the pre-test likelihood is 50%, an exercise echocardiogram showing inducible ischemia indicates an 83% likelihood of coronary disease, whereas a negative test indicates only a 15% likelihood of coronary disease.
 Prompting a change in therapy or
Prompting a change in therapy or
 Leading to a change in the subsequent diagnostic strategy in that patient.
Leading to a change in the subsequent diagnostic strategy in that patient.
 A lower threshold below which the risk of the test is greater than the risk of not treating the patient and
A lower threshold below which the risk of the test is greater than the risk of not treating the patient and
 An upper threshold above which treating the patient is a lower risk than performing the test.
An upper threshold above which treating the patient is a lower risk than performing the test.
The intermediate range—in which the risk of treating or not treating the patient is greater than the risk of the diagnostic test—is known as the testing zone (Fig. 5-4). For any specific indication, the testing zone for echocardiography generally is wide because of the low risk and high accuracy of this technique. However, both an upper and lower threshold still are definable for echocardiography. The upper threshold is reached in situations in which the diagnosis is clear, and echocardiographic examination would only delay appropriate treatment. For example, a patient with a classic presentation of an ascending aortic dissection (chest pain, wide mediastinum, peripheral pulse loss) requires prompt surgery. Any delay caused by unnecessary diagnostic testing could result in additional morbidity or mortality.
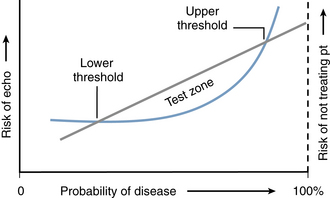
Figure 5–4 Threshold approach to clinical decision making.
The risk of the diagnostic test—in this case, echocardiography—is shown by the curved blue line (left y-axis) with the risk of not treating the patient for the suspected disease shown by the straight gray line (right y-axis). The probability of disease based on the clinical presentation is shown from 0% to 100% on the x-axis. The lower threshold is the point at which the risk of not treating the patient is greater than the risk of echocardiography. The upper threshold is the point at which the risk of echocardiography (including false-negative results, delay in treatment) is greater than the risk of not treating the patient. The test zone is the pre-test likelihood of disease between these two thresholds.
Clinical Outcomes
The most important measure of the value of a diagnostic test is its impact on subsequent clinical outcome (Fig. 5-5). While the first step in evaluation of the clinical utility of a test includes various measures of diagnostic accuracy in comparison to some accepted standard, the more important assessment is whether the diagnostic test changes the subsequent diagnostic or therapeutic plan in each patient. The definitive value of echocardiography depends on its ability to predict prognosis, for example, survival in patients with dilated cardiomyopathy, timing of valve surgery in patients with chronic regurgitation, or the rate of hemodynamic progression in patients with valvular stenosis. Echocardiographic data are increasingly used in clinical outcome studies, as referenced in the suggested readings throughout this textbook.
Indications and Appropriateness Criteria
The indications for echocardiography are based on the reliability of this approach for diagnosis in a wide range of cardiovascular diseases and are summarized in consensus guidelines developed by the American Heart Association and the American College of Cardiology. In addition, specific recommendations on the use of echocardiography often are included in disease-specific guidelines, for example, guidelines for the management of valvular heart disease and for heart failure.
 Making the correct anatomic diagnosis. For example, differentiating a primary valvular problem from systolic LV dysfunction in a patient with heart failure symptoms.
Making the correct anatomic diagnosis. For example, differentiating a primary valvular problem from systolic LV dysfunction in a patient with heart failure symptoms.
 Providing important prognostic data in a patient with a known anatomic diagnosis. For example, vegetation size in endocarditis, or LV ejection fraction in cardiomyopathy.
Providing important prognostic data in a patient with a known anatomic diagnosis. For example, vegetation size in endocarditis, or LV ejection fraction in cardiomyopathy.
 Identifying complications of a known diagnosis. For example, paravalvular abscess in endocarditis or LV thrombus in cardiomyopathy.
Identifying complications of a known diagnosis. For example, paravalvular abscess in endocarditis or LV thrombus in cardiomyopathy.
 Assessing the effect of therapy. For example, reevaluation of LV systolic function after optimization of heart failure therapy.
Assessing the effect of therapy. For example, reevaluation of LV systolic function after optimization of heart failure therapy.
Throughout this text, the accuracy (sensitivity and specificity) of echocardiography for each specific diagnosis will be indicated, if known. The clinician then should integrate these data with the pre-test likelihood of disease in each patient. Critical evaluations of the diagnostic utility of echocardiography in specific patient populations and clinical settings will be highlighted, including evaluation of chest pain in the emergency room (Chapter 8), decision making in adults with aortic stenosis (Chapter 11) and aortic regurgitation (Chapter 12), the diagnosis and prognosis of endocarditis (Chapter 14), and intraoperative assessment of mitral valve repair (Chapter 18).
Definitions and Classification of Echocardiographic Studies
Echocardiographic imaging also is used to monitor cardiac interventions for the evaluation of procedural results and the detection of complications (Table 5-1). For example, transesophageal echocardiography (TEE) to monitor interventions in the operating room and interventional suite usually are performed and simultaneously interpreted by cardiac anesthesiologists or cardiologists participating in the procedure (see Chapter 18). Intracardiac echocardiographic (ICE) monitoring typically is done by the interventional cardiologist or electrophysiologist who is performing the primary procedure (see Chapter 4). The results of monitoring studies are included in the procedure report, and selected images may be archived.