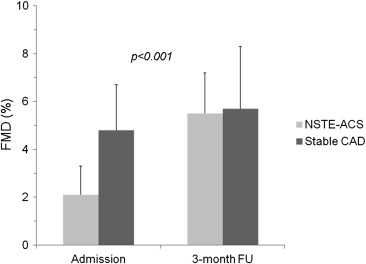
Endothelial dysfunction can predict cardiovascular outcomes in several populations of patients. The aim of this study was to assess the severity, time course, and clinical implications of endothelial dysfunction in patients with non–ST-segment elevation (NSTE) acute coronary syndromes (ACS). Sixty patients with NSTE ACS (mean age 62 ± 8 years, 44 men) and 40 controls with stable coronary artery disease (CAD) (mean age 63 ± 10 years, 27 men) were studied. In patients with NSTE ACS and in those with stable CAD, endothelial function was assessed <12 hours after admission and at 3-month follow-up by measuring right brachial artery dilation after 5 minutes of forearm ischemia (flow-mediated dilation [FMD]). Clinical outcomes were assessed after a median follow-up period of 32 months (range 14 to 36). The primary end point was a combination of cardiac death or readmission for new ACS or recurrence of angina pectoris. FMD on admission was significantly lower in patients with NSTE ACS compared to those with stable CAD (2.1 ± 1.2% vs 4.8 ± 1.9%, p <0.001). FMD improved significantly at 3-month follow-up in patients with NSTE ACS, becoming comparable to that in patients with stable CAD (5.7 ± 2.6% vs 5.5 ± 1.7%, p = 0.93). During follow-up, 14 cardiac events (23%) occurred in patients with NSTE ACS. On multivariate analysis, only diabetes (hazard ratio 18.1, 95% confidence interval 3.9 to 83.9, p <0.001) and FMD at 3 months (hazard ratio 0.78, 95% confidence interval 0.61 to 0.99, p = 0.04) were independent predictors of the primary end point in patients with NSTE ACS. In conclusion, endothelial function is markedly impaired in the acute phase of NSTE ACS but improves significantly at 3-month follow-up. In patients with NSTE ACS, FMD at 3 months after the acute event is a significant independent predictor of cardiac outcomes.
Endothelial dysfunction (ED) is the earliest vascular abnormality in the process leading to atherosclerosis. Furthermore, ED also favors vascular plaque complications, as well as platelet activation and aggregation, all of which can result in acute coronary thrombosis. Accordingly, ED has been associated with an increased risk for cardiovascular events in several clinical settings. In patients with acute coronary syndromes (ACS), several clinical and laboratory variables have been shown to be associated with an increased risk for cardiovascular events. Although a few studies have suggested a prognostic role also for ED in these patients, this aspect remains poorly investigated. Moreover, there is scant knowledge of the behavior of endothelial function in ACS and of whether variations in endothelial function over time may have any impact on clinical outcomes. A noninvasive, broadly applied, and now well-validated method to assess endothelial function is flow-mediated dilation (FMD) of the brachial artery after forearm ischemia. In this study, we aimed to define characteristics and clinical and laboratory correlates of ED, together with its changes and clinical impact in patients with non–ST-segment elevation (NSTE) ACS. A group of patients with stable coronary artery disease (CAD) was studied as a control group.
Methods
We studied 60 consecutive patients (mean age 62 ± 8 years, 44 men), admitted to our coronary care unit from May 2008 to May 2009 with diagnoses of NSTE ACS and fulfilling the following inclusion criteria: (1) ≥1 episode of chest pain at rest within the previous 48 hours, associated with ST-segment depression and/or T-wave abnormalities on electrocardiography, with or without increments of markers of myocardial necrosis, (2) no need for urgent coronary angiography, (3) confirmation of significant CAD (≥1 epicardial vessels with >50% stenosis) on angiography, (4) normal sinus rhythm on electrocardiography, (5) a normal left ventricular ejection fraction (>50%) on 2-dimensional echocardiography, (6) no significant hepatic or renal dysfunction, and (7) no evidence of malignant disease or of acute or chronic inflammatory disease. During the same period, we studied 40 gender- and age-matched patients (mean 63 ± 10 years, 27 men) admitted to undergo elective coronary angiography for a history of stable effort angina for ≥3 months and documented stress-induced myocardial ischemia.
All patients were studied <12 hours after admission and after 3 months from discharge. On admission, tests were performed before any invasive procedure. All tests were performed with patients taking drug therapy as prescribed by their attending physicians. Drug therapy was largely comparable in the 2 groups and remained unchanged during the first 3 months after discharge.
A detailed assessment of cardiovascular risk factors was done for each patient. Hypertension was defined as blood pressure ≥140/90 mm Hg or consumption of any antihypertensive drug; hypercholesterolemia was defined as total blood cholesterol level >200 mg/dl, low-density lipoprotein cholesterol ≥130 mg/dl, or consumption of lipid-lowering drugs; active smoking was defined as smoking any cigarette in the past month; diabetes mellitus was defined as fasting plasma glucose >126 mg/dl or treatment with any antidiabetic drug; and family history of CAD was considered to be present if any first-degree relative had had CAD events before 60 years of age.
Written informed consent to participate in the study was obtained from all patients. This study was in agreement with the guidelines approved by the ethics committee at our institution.
Systemic endothelium-dependent and endothelium-independent arterial dilator function was assessed by measuring FMD and nitrate-mediated dilation (NMD) of the brachial artery, respectively, using methods described in detail elsewhere. Subjects rested in a supine position for ≥10 minutes in a warm, quiet room (22°C to 24°C) before testing. A 10-MHz multifrequency probe attached to a high-resolution ultrasound machine was used to acquire images of the right brachial artery. Brachial artery diameter was measured throughout the test using a totally automated system that identifies the internal edges of the vessel and provides a diameter measurement every second; the probe is kept in a fixed position by a mechanical support throughout the whole examination. After baseline images of the right brachial artery were obtained for 1 minute, a forearm cuff, positioned 1 cm under the antecubital fossa, was inflated to 250 mm Hg. The cuff was released 5 minutes after inflation, thus inducing forearm reactive hyperemia. The basal diameter was defined as the average of all measures collected during the first minute, and FMD was calculated as the maximum percentage change of the brachial artery diameter after hyperemia compared to the basal diameter. Maximal Doppler flow velocity was also measured at baseline and at peak forearm hyperemia using the lowest insonation angle (always <60°), which did not vary throughout each study.
After recovery of brachial artery diameter to basal values, a dose of 25 μg of sublingual glyceryl trinitrate was administered. NMD was calculated as the maximum percentage change of brachial artery diameter in the following 5 minutes, compared to basal brachial artery diameter.
In patients with NSTE ACS, troponin T was measured on admission, after 6 hours, and every 12 hours thereafter, if indicated, by electroimmunoassay, based on electrochemiluminescence technology (Elecsys 2010; Roche Diagnostics, Mannheim, Germany), with a lowest detection limit of 0.01 ng/ml. To assess subclinical inflammatory state, serum C-reactive protein (CRP) levels were measured in all patients on admission and at 3-month follow-up using a high-sensitivity nephelometric method (BN100; Behring Diagnostic, Milan, Italy), with a lowest detection limit of 0.05 mg/L.
To assess sympathovagal cardiac autonomic balance, we measured heart rate variability on 24-hour 3-channel electrocardiographic Holter monitoring, which, at enrollment, was started <12 hours after admission. For the purposes of this study, the heart rate variability parameters low-frequency (0.04 to 0.15 Hz) and high-frequency (0.15 to 0.40 Hz) amplitudes were obtained by fast-Fourier transform spectral analysis of 24-hour sinus RR intervals using the Oxford Medilog Excel 3 system software (Oxford Instrument, Abingdon, United Kingdom) and following a method described in detail elsewhere.
Clinical follow-up of patients was performed through ambulatory clinical visits. Patients were asked in detail about clinical events occurring during the period of follow-up, and documentation of the events was carefully checked. In case of death, the cause was established from detailed information from the patient’s physician or, if available, clinical records. The primary clinical end point was a combination of cardiac death and readmissions for nonfatal ACS (defined as typical chest pain at rest, associated with either ST-segment depression or elevation, with or without increases in markers of myocardial necrosis), or recurrence of angina.
Continuous variables were tested for normality using the Kolmogorov-Smirnov test, and between-group comparisons were done using Student’s unpaired t tests or Mann-Whitney U tests as indicated. Proportions were compared using Fisher’s exact test, and correlation analyses were performed using Pearson’s tests. A repeated-measures analysis of variance design was applied to assess differences in the changes of FMD and NMD at follow-up between NSTE ACS and stable CAD groups. Between- and within-group comparisons were done using Student’s unpaired and paired t tests, respectively, and statistical results were adjusted for multiple comparisons using Bonferroni’s rule. Cox proportional-hazards regression analysis was used to determine the univariate and multivariate predictors of clinical events. Variables with p values <0.10 on univariate analysis were included in the multivariate model. FMD in statistical analyses was initially included as a continuous variable. However, to further define its prognostic power, we also analyzed the relation of tertile FMD values (at enrollment and at follow-up) with clinical events in Cox survival analyses. Furthermore, event-free survival curves of patients with FMD values in the lowest tertile compared to the other 2 tertiles were constructed using the Kaplan-Meier method, and curves were compared using log-rank tests. Statistical analyses were done using SPSS version 17.0 (SPSS Italia, Florence, Italy). Data are expressed as mean ± SD. Statistical significance was considered for p values <0.05.
Results
All main baseline clinical characteristics of patients with NSTE ACS and of those with stable CAD are listed in Table 1 . There were no significant differences between the 2 groups with regard to age, gender, cardiovascular risk factors, and medical therapy, except anticoagulant drugs, which were administered only to patients with NSTE ACS. All patients underwent complete coronary revascularization during hospitalization. In particular, 50 patients in the NSTE ACS group (83%) and 29 patients in the stable CAD group (72%) (p = 0.22) underwent percutaneous coronary interventions, whereas the other patients underwent surgical coronary revascularization.
| Variable | NSTE ACS (n = 60) | Stable CAD (n = 40) | p Value |
|---|---|---|---|
| Age (yrs) | 62 ± 8 | 63 ± 10 | 0.45 |
| Men/women | 44/16 | 27/13 | 0.65 |
| Family history of CAD | 28 (47%) | 20 (50%) | 0.84 |
| Hypertension ∗ | 48 (80%) | 32 (80%) | 1.00 |
| Diabetes mellitus | 17 (28%) | 17 (42%) | 0.20 |
| Hypercholesterolemia † | 42 (70%) | 26 (65%) | 0.66 |
| Hypertriglyceridemia | 32 (53%) | 15 (37%) | 0.15 |
| Active smokers | 20 (33%) | 13 (33%) | 1.00 |
| Body mass index (kg/m 2 ) | 27 ± 3 | 27 ± 4 | 0.66 |
| CAD | |||
| 1-vessel | 18 (30%) | 13 (32%) | |
| 2-vessel | 15 (25%) | 14 (36%) | 0.40 |
| 3-vessel | 27 (45%) | 13 (32%) | |
| Coronary artery bypass surgery | 10 (17%) | 11 (27%) | 0.22 |
| Percutaneous coronary intervention | 50 (83%) | 29 (73%) | |
| Drug therapy | |||
| Antiplatelet agents | 60 (100%) | 40 (100%) | 1.00 |
| Anticoagulant drugs | 60 (100%) | — | — |
| β blockers | 51 (85%) | 38 (95%) | 0.19 |
| Calcium antagonists | 12 (20%) | 7 (17.5%) | 0.80 |
| Nitrates | 13 (22%) | 5 (12%) | 0.29 |
| Angiotensin-converting enzyme inhibitors/angiotensin receptor blockers | 58 (97%) | 37 (93%) | 0.90 |
| Statins | 58 (97%) | 35 (87%) | 0.11 |
| Oral antidiabetic drugs | 17 (28%) | 17 (42%) | 0.20 |
∗ Blood pressure ≥140/90 mm Hg or consumption of any antihypertensive drug.
† Total blood cholesterol >200 mg/dl, low-density lipoprotein cholesterol ≥130 mg/dl, or consumption of lipid-lowering drugs.
Data of laboratory results and vascular function are listed in Table 2 . On admission, patients with NSTE ACS showed significantly higher serum CRP levels (p <0.001) and lower low-frequency amplitude (p = 0.01) compared to those with stable CAD. Baseline values of brachial artery diameter (3.0 ± 0.7 vs 3.2 ± 0.8 mm, respectively, p = 0.16) and blood flow velocity (45 ± 11 vs 46 ± 11 cm/s, respectively, p = 0.74) were comparable in the NSTE ACS and stable CAD groups. Similarly, no difference was found between the 2 groups in peak blood flow velocity during hyperemia (76 ± 15 vs 79 ± 15 cm/s, respectively, p = 0.34). FMD values, however, were significantly lower in patients with NSTE ACS compared to those with stable CAD ( Figure 1 ), whereas there was no difference between the 2 groups in NMD values ( Table 2 ). In patients with NSTE ACS, no clinical or laboratory variable was found to be significantly associated with FMD values on admission, including peak troponin T level, CRP level, and heart rate variability parameters ( Table 3 ).
| Variable | NSTE ACS (n = 60) | Stable CAD (n = 40) | p Value |
|---|---|---|---|
| Admission | |||
| FMD (%) | 2.1 ± 1.2 | 4.8 ± 1.9 | <0.001 |
| NMD (%) | 11.7 ± 1.0 | 12.1 ± 2 | 0.10 |
| CRP serum level (mg/L) | 14.8 ± 14 | 2.9 ± 2 | <0.001 |
| Peak troponin T (ng/ml) | 2.2 ± 3.7 | — | — |
| RR interval (ms) | 870 ± 125 | 935 ± 119 | 0.01 |
| Low-frequency amplitude (ms) | 20 ± 16 | 28 ± 21 | 0.01 |
| High-frequency amplitude (ms) | 13 ± 6 | 17 ± 16 | 0.41 |
| 3-month follow-up | |||
| FMD (%) | 5.5 ± 1.7 ∗ | 5.7 ± 2.6 † | 0.76 |
| NMD (%) | 11.8 ± 1.9 | 12.2 ± 1.8 | 0.12 |
| CRP serum level (mg/L) | 3.7 ± 5 ∗ | 3.0 ± 2 | 0.42 |
| RR interval (ms) | 893 ± 135 | 915 ± 124 | 0.42 |
| Low-frequency amplitude (ms) | 24 ± 23 ‡ | 25 ± 15 | 0.87 |
| High-frequency amplitude (ms) | 17 ± 22 | 15 ± 9 | 0.65 |
| Variable | Value | p Value |
|---|---|---|
| Gender | 0.83 | |
| Male (n = 44) | 2.09 ± 1.0 | |
| Female (n = 16) | 2.17 ± 1.5 | |
| Active smoker | 0.16 | |
| Yes (n = 20) | 1.80 ± 1.1 | |
| No (n = 40) | 2.27 ± 1.3 | |
| Hypertension ∗ | 0.71 | |
| Yes (n = 48) | 2.15 ± 1.1 | |
| No (n = 12) | 2.00 ± 1.7 | |
| Diabetes mellitus | 0.66 | |
| Yes (n = 17) | 2.01 ± 1.2 | |
| No (n = 43) | 2.16 ± 1.2 | |
| Hypercholesterolemia † | 0.34 | |
| Yes (n = 42) | 2.22 ± 1.2 | |
| No (n = 18) | 1.88 ± 1.2 | |
| Family history of CAD | 0.83 | |
| Yes (n = 28) | 2.15 ± 1.0 | |
| No (n = 32) | 2.08 ± 1.4 | |
| Multivessel CAD | 0.22 | |
| Yes (n = 42) | 2.00 ± 1.2 | |
| No (n = 18) | 2.40 ± 1.3 | |
| Age | r = 0.03 | 0.81 |
| Peak troponin T | r = −0.16 | 0.23 |
| CRP serum level | r = −0.22 | 0.09 |
| RR interval | r = 0.04 | 0.75 |
| Low-frequency amplitude | r = −0.23 | 0.08 |
| High-frequency amplitude | r = −0.05 | 0.70 |
∗ Blood pressure ≥140/90 mm Hg or consumption of any antihypertensive drug.
† Total blood cholesterol >200 mg/dl, low-density lipoprotein cholesterol ≥130 mg/dl, or consumption of lipid-lowering drugs.
At 3-month follow-up, no significant differences were observed between patients with NSTE ACS and those with stable CAD in serum CRP levels and heart rate variability parameters ( Table 2 ). Similarly, there were no differences between the 2 groups in baseline values of brachial artery diameter (3.1 ± 0.6 vs 3.3 ± 0.7 mm, respectively, p = 0.27) and blood flow velocity (42 ± 11 vs 46 ± 12 cm/s, respectively, p = 0.18), as well as in peak blood flow velocity during hyperemia (74 ± 14 vs 77 ± 19 cm/sec, respectively, p = 0.35).
Compared to enrollment, FMD at 3 months showed a significant improvement in patients with NSTE ACS (p <0.001) and in those with stable CAD (p <0.01). The improvement, however, was much larger in patients with NSTE ACS (p <0.001 for changes between groups; Figure 1 ). As a result, at 3 months, there was no difference between the 2 groups in FMD values ( Table 2 ). No difference was found also at follow-up between the 2 groups in NMD values, which remained unchanged in the 2 groups (p for changes = 0.20; Table 2 ).
During a median follow-up period of 32 months (range 14 to 36), 14 patients with NSTE ACS (23%) developed primary end points. All events occurred after the 3-month assessment of FMD. Two patients (3%) died from acute ST-segment elevation ACS, 10 patients (17%) were admitted for new NSTE ACS, and 2 patients (3%) underwent elective percutaneous coronary intervention for recurrence of effort angina and angiographic evidence of in-stent restenosis.
The univariate relation of clinical and laboratory variables with the primary end point is listed in Table 4 . Among clinical variables, only diabetes (p <0.001) was significantly associated with the primary end point, whereas no laboratory variable at enrollment, including FMD, as a continuous or dichotomized (first tertile vs second and third tertiles) variable, was significantly predictive of the primary end point of the study. FMD measured at 3-month follow-up, instead, showed a significant association with clinical events, as a continuous variable (p = 0.003) and as a dichotomized variable, with patients with FMD values in the lowest tertile (≤4.1%; n = 20) showing significantly worse event-free survival compared to those in the 2 highest tertiles (>4.1%; n = 40). Events occurred in 9 (47%) and 5 (12%) patients in these 2 groups, respectively (p = 0.007; Figure 2 ). Table 5 lists details about the associations of FMD with clinical events.



