The aim of the present study was to assess the clinical and prognostic significance of right ventricular (RV) dilation and RV hypertrophy at echocardiography in patients with idiopathic pulmonary arterial hypertension. Echocardiography and right heart catheterization were performed in 72 consecutive patients with idiopathic pulmonary arterial hypertension admitted to our institution. The median follow-up period was 38 months. The patients were grouped according to the median value of RV wall thickness (6.6 mm) and the median value of the RV diameter (36.5 mm). On multivariate analysis, the mean pulmonary artery pressure (p = 0.018) was the only independent predictor of RV wall thickness, and age (p = 0.011) and moderate to severe tricuspid regurgitation (p = 0.027) were the independent predictors of RV diameter. During follow-up, 22 patients died. The death rate was greater in the patients with a RV diameter >36.5 mm than in patients with a RV diameter ≤36.5 mm: 15.9 (95% confidence interval 9.4 to 26.8) vs 6.6 (95% confidence interval 3.3 to 13.2) events per 100-person years (p = 0.0442). In contrast, the death rate was similar in patients with RV wall thickness above or below the median value. However, among the patients with a RV wall thickness >6.6 mm, a RV diameter >36 mm was not associated with a poorer prognosis (p = 0.6837). In conclusion, in patients with idiopathic pulmonary arterial hypertension, a larger RV diameter is a marker of a poor prognosis but a greater RV wall thickness reduces the risk of death associated with a dilated right ventricle.
The aim of the present study was to assess the determinants and prognostic relevance of right ventricular (RV) dilation and RV hypertrophy at echocardiography in patients with idiopathic pulmonary arterial hypertension (IPAH) and to test the hypothesis that a greater RV wall thickness is associated with better circulatory function and a better prognosis in such patients.
Methods
From July 1996 to March 2009, 72 patients were consecutively admitted to our institution for the evaluation of chronic pulmonary hypertension and were diagnosed with IPAH. The diagnosis was made after having ruling out the known causes of pulmonary hypertension. Patients with different etiologies of pulmonary hypertension were excluded. All patients underwent right heart catheterization and ultrasound examination during the hospitalization period. The patients were followed up for a median of 38 months (interquartiles range 14 to 71). During follow-up, the patients were treated according to international guidelines. The enrollment of patients expanded over several years; thus, the treatments varied over time. However, the clinical decisions were never made on the basis of the echocardiographic parameters of RV function because this was never recommended by the guidelines.
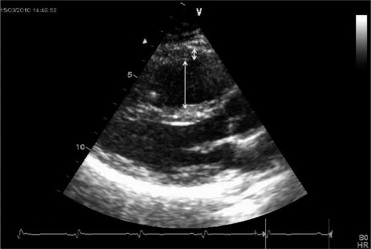
The echocardiographic examinations were performed in the same laboratory using commercially available ultrasound equipments. The complete echocardiographic protocol and intra- and interobserver agreement for the most important echocardiographic parameters have been previously reported. All echocardiographic data were averaged for 3 beats. The 2 parameters of interest in the present analysis (i.e., the RV end-diastolic diameter and the thickness of the RV free wall) were determined in the parasternal view ( Figure 1 ).
A Swan Ganz thermodilution catheter (American Edwards Laboratories, Irvine, California) was inserted transcutaneously by way of the right internal jugular vein. The thermistor was connected to a dedicated computer to display the cardiac output on-line. The following hemodynamic parameters were measured or calculated: systemic blood pressure (arm cuff sphygmomanometer), right atrial pressure, systolic, diastolic, and mean pulmonary artery pressure, pulmonary wedge pressure, cardiac output, cardiac index, systemic vascular resistance, and pulmonary vascular resistance. All the thermodilution measurements were obtained in triplicate. In most cases, the ultrasound examination and the right heart catheterization were performed on the same day.
The data are shown as the mean ± SD for the continuous variables and as the absolute and relative frequencies for the categorical variables. Pearson’s coefficient was used to evaluate the correlations between the continuous variables. The RV wall thickness and RV diameter were dichotomized on the basis of their median distribution and the between-group differences in the clinical, hemodynamic, and echocardiographic characteristics were compared. The mean group values were compared using the 2-tailed t test or the Mann-Whitney U test and proportions using the Fisher exact test. To identify the independent predictors of RV wall thickness and RV diameter, log-linear models were fitted; noncollinear variables showing p <0.2 on univariate analysis were included in the models. The relative risks and 95% confidence intervals (CIs) were computed. Cumulative survival was calculated using the Kaplan-Meier estimates. The relative risk of dying and its 95% CI were computed using a Cox model. All survival models included the year of diagnosis to account for the prolonged enrollment period of the study. Cardiac death was the only end point of the survival analysis; lung transplantation was considered as a censored observation, and those patients were withdrawn from the analysis at the intervention.
p Values <0.05 were retained for statistical significance. The computations were made using Stata, version 11 (StataCorp, College Station, Texas).
Results
Of the 72 patients, 20 were men and 52 were women. Their mean age was 52 ± 16 years. The World Health Organization functional class at referral was II for 17 patients and III-IV for 55 patients. The main echocardiographic and hemodynamic characteristics were as follows: RV diameter 37.8 ± 8.7 mm; RV wall thickness 6.7 ± 1.9 mm; tricuspid annular plane systolic excursion 14.9 ± 4.2 mm; moderate to severe tricuspid regurgitation 71.8% of patients; left ventricular ejection fraction 60 ± 8%; mean pulmonary artery pressure 51.0 ± 13.8 mm Hg; pulmonary vascular resistance 12.5 ± 6.3 Wood Units; cardiac index 2.3 ± 0.7 L/min/m 2 ; and right atrial pressure 7.6 ± 4.7 mm Hg.
The median RV diameter was 36.5 mm (range 7 to 13). The patients were accordingly divided into 2 groups: patients with a RV diameter >36.5 mm and those with a RV diameter of ≤36.5 mm. Their clinical, hemodynamic, and echocardiographic characteristics are listed in Table 1 . More female patients had a RV diameter of ≤36.5 mm. The right heart hemodynamic profile of the patients with a RV diameter greater than the median was characterized by greater pulmonary vascular resistance, greater right atrial pressure, and a lower cardiac index. Greater RV dysfunction was observed at echocardiography in the patients with a RV diameter >36.5 mm. On multivariate analysis, age (relative risk 1.01, 95% CI 1.00 to 1.02, p = 0.011) and tricuspid regurgitation (relative risk 9.9, 95% CI 1.3 to 77.9, p = 0.027) were the independent variables associated with the RV diameter.
| Variable | RV Diameter (mm) | p Value | |
|---|---|---|---|
| ≤36.5 (n = 36) | >36.5 (n = 36) | ||
| Age (years) | 50.3 ± 16.8 | 53.1 ± 16.6 | 0.483 |
| Gender | 0.017 | ||
| Women | 31 | 21 | |
| Men | 5 | 15 | |
| Functional class III or IV | 69% | 83% | 0.173 |
| Systolic pulmonary artery pressure (mm Hg) | 76.1 ± 22.5 | 84.0 ± 19.3 | 0.116 |
| Mean pulmonary artery pressure (mm Hg) | 48.0 ± 13.7 | 54.0 ± 13.8 | 0.066 |
| Pulmonary capillary wedge pressure (mm Hg) | 9.5 ± 4.4 | 10.3 ± 4.0 | 0.453 |
| Pulmonary vascular resistance (Wood Units) | 10.7 ± 4.6 | 14.3 ± 7.2 | 0.014 |
| Cardiac index (L/min/m 2 ) | 2.4 ± 0.6 | 2.1 ± 0.7 | 0.044 |
| Right atrial pressure (mm Hg) | 6.2 ± 3.4 | 9.0 ± 5.3 | 0.010 |
| Right ventricular wall thickness (mm) | 6.5 ± 2.0 | 6.8 ± 1.9 | 0.434 |
| Transtricuspid gradient (mm Hg) | 70.0 ± 18.8 | 75.4 ± 19.0 | 0.237 |
| Right ventricular fractional area change | 28.7 ± 10.3% | 20.6 ± 8.5% | 0.001 |
| Tricuspid annular plane systolic excursion (mm) | 16.6 ± 3.3 | 13.2 ± 4.4 | 0.000 |
| Moderate/severe tricuspid regurgitation | 49% | 97% | 0.000 |
| Inferior vena cava collapsibility | 85% | 33% | 0.000 |
| Left ventricular end-diastolic volume (ml) | 62 ± 26 | 54 ± 12 | 0.131 |
| Left ventricular ejection fraction | 61 ± 7% | 60 ± 8% | 0.410 |
The median RV wall thickness was 6.6 mm (range 3 to 13), and the patients were divided into 2 groups: those with a RV wall thickness >6.6 mm and those with a RV wall thickness of ≤6.6 mm. Their clinical, hemodynamic, and echocardiographic characteristics are listed in Table 2 . The right heart hemodynamic profile of the patients with a RV wall thickness greater than the median was characterized by greater systolic and mean pulmonary artery pressures, greater pulmonary vascular resistance, and a slightly lower cardiac index. The clinical and echocardiographic characteristics were substantially similar within the 2 groups, except for a slightly greater RV diameter in the patients with a greater RV wall thickness. The mean pulmonary artery pressure (relative risk 1.02, 95% CI 1.00 to 1.04, p = 0.018) was the only variable independently associated with the RV wall thickness on multivariate analysis.
| Variable | RV Wall Thickness (mm) | p Value | |
|---|---|---|---|
| ≤6.6 (n = 37) | >6.6 (n = 35) | ||
| Age (years) | 55.0 ± 13.4 | 48.3 ± 19.1 | 0.086 |
| Gender | 0.116 | ||
| Women | 30 | 22 | |
| Men | 7 | 13 | |
| Functional class III or IV | 76% | 76% | 1.000 |
| Systolic pulmonary artery pressure (mm Hg) | 70.8 ± 20.8 | 89.9 ± 16.6 | 0.000 |
| Mean pulmonary artery pressure (mm Hg) | 46.0 ± 12.7 | 56.3 ± 13.1 | 0.001 |
| Pulmonary capillary wedge pressure (mm Hg) | 9.7 ± 4.3 | 9.6 ± 4.1 | 0.555 |
| Pulmonary vascular resistance (Wood Units) | 10.5 ± 5.8 | 14.6 ± 6.1 | 0.004 |
| Cardiac index (L/min/m 2 ) | 2.4 ± 0.7 | 2.1 ± 0.6 | 0.031 |
| Right atrial pressure (mm Hg) | 7.5 ± 4.7 | 7.7 ± 4.7 | 0.837 |
| Right ventricular diameter (mm) | 35.6 ± 6.7 | 40.2 ± 9.9 | 0.022 |
| Transtricuspid gradient (mm Hg) | 64.7 ± 16.3 | 81.5 ± 17.9 | 0.000 |
| Right ventricular fractional area change | 26.3 ± 9.3% | 22.9 ± 11.0% | 0.188 |
| Tricuspid annular plane systolic excursion (mm) | 15.1 ± 4.3 | 14.7 ± 4.2 | 0.702 |
| Moderate/severe tricuspid regurgitation | 67% | 79% | 0.293 |
| Inferior vena cava collapsibility | 66% | 53% | 0.328 |
| Left ventricular end-diastolic volume (ml) | 60 ± 26 | 56 ± 15 | 0.470 |
| Left ventricular ejection fraction | 60 ± 7% | 61 ± 9% | 0.474 |
During the follow-up period, 22 patients died. The death rate per 100 person-years was 6.6 (95% CI 3.3 to 13.2) for the patients with a RV diameter of ≤36.5 mm and 15.9 (95% CI 9.4 to 26.8) for the patients with a RV diameter >36.5 mm. The enrollment-year adjusted hazard ratio was 2.64 (95% CI 1.06 to 6.57; p = 0.036). The death rate per 100 person-years was 11.2 (95% CI 6.3 to 19.7) for the patients with a RV wall thickness of ≤6.6 mm and 9.8 (95% CI 5.3 to 18.3) for the patients with a RV wall thickness >6.6 mm. The enrollment-year adjusted hazard ratio was 0.88 (95% CI 0.38 to 2.08; p = 0.785). A clear interaction was seen between the RV wall thickness and RV diameter on the prognosis. In patients with a RV wall thickness at or less than the median, dilation had a strong negative prognostic effect. The death rate per 100 person-years was 5.4 (95% CI 2.0 to 14.5) for the patients with a RV wall thickness of ≤6.6 mm and RV diameter of ≤36.5 mm, but it was 23.5 (95% CI 11.8 to 47.1) for the patients with a RV wall thickness of ≤6.6 mm and RV diameter >36.5 mm. The adjusted hazard ratio was 4.23 (95% CI 1.21 to 14.82; p = 0.024; Figure 2 ). In contrast, in patients with a RV wall thickness greater than the median, dilation had no significant negative prognostic effect. The death rate per 100 person-years was 8.4 (95% CI 3.2 to 22.5) for the patients with a RV wall thickness >6.6 mm and RV diameter of ≤36.5 mm and was 11.1 (95% CI 5.0 to 24.6) for the patients with a RV wall thickness >6.6 mm and RV diameter >36.5 mm. Adjusted hazard ratio 1.70 (95% CI 0.46 to 6.34; p = 0.428; Figure 2 ).




