Fig. 12.1
(a) Late changes in the foot – equinus deformity. (b) Late changes in the foot – champagne glass appearance
The champagne glass appearance (narrow ankle and expanded calf segment) is another deformity from fibrosis around the ankle and LDS changes.
Malignant change in venous ulcer (Marjolin’s ulcer) is an uncommon but dangerous event. The commonest type of malignancy is squamous cell carcinoma; basal cell carcinomas are also reported. The transformation to a malignant pathology is a slow process taking on an average 20–40 years. The lesion can destroy the underlying bone. Diagnosis is confirmed by a biopsy; MRI is the recommended imaging technique. Excision with a surrounding margin of 3–4 cm followed by skin grafting of the defect is the recommended treatment. Nodal involvement is not common because of fibrosis; but if the lesion extends to involve the normal tissue beyond the margin of the ulcer, regional lymph nodes can be affected. If lymph nodes are involved, lymphadenectomy is recommended. Inoperable lesions are treated by combination of radiation and chemotherapy with 5 FU, cisplatin, and methotrexate [8] (Fig. 12.2).


Fig. 12.2
Squamous cell carcinoma in a long-standing venous ulcer (Marjolin’s ulcer). The arrow points to the everted edge
Chronic Venus Insufficiency: Investigations
The end stage of CVI is the venous ulcer. The defect in a patient with venous ulcer may vary from simple reflux in the saphenous system to extensive structural changes in the deep venous system. The pathology in the deep venous system is strikingly different in the primary and secondary category of CVI. Again a patient with leg ulcer can have comorbidities that can affect wound healing. The goals of investigations are to clarify the following issues: to identify any systemic illness or factors that can interfere with wound healing, to differentiate primary from secondary CVI, and to identify the specific pathology in primary CVI.
Laboratory Studies
This would include routine hemogram and blood biochemistry. Anemia and diabetes are important systemic factors interfering with wound healing. Leg ulcers can result from multiple causes. These include ischemic ulcers, vasculitic ulcers, rheumatoid ulcers, and numerous other causes. Tests to rule out dyslipidemia, vasculitis, rheumatoid, and autoimmune diseases would be needed in relevant cases. Thrombophilia studies are relevant in patients with post-thrombotic ulcers.
Diagnostic Venous Investigations
An array of tests both invasive and noninvasive are available for the diagnosis of CVD. Some of them are useful in assessment of the morphological changes and others for the hemodynamic alterations. The choice of the investigations should be need based. Based on the severity of the problem and the management strategies planned, three levels of investigation are suggested [5]. Level one investigations include clinical examination and evaluation by HHD. Level 2 investigations include duplex scan along with plethysmographic studies. Level 3 studies include invasive tests such as ascending and descending venography, CT/MR venograms and venous pressure studies, intravascular ultrasound, etc. This approach is useful in optimizing the use of these tests. Patients who are to be managed by conservative methods need only level 1 studies; when superficial vein ablation and perforator surgery alone are decided, level 2 would be sufficient. Patients requiring complex procedures such as valve reconstructions or venous bypass or endovenous stenting would need level 3 tests. Good number of patients with CVI would need level 3 studies. To obtain maximum diagnostic accuracy, it is important that these tests are performed and interpreted by clinicians or technicians who are well versed with venous problems [4].
Duplex Scan Evaluation in CVI
Currently this is considered the gold standard for the evaluation of patients with CVI. Duplex scan combines ultrasound imaging along with a Doppler evaluation. Color coding of the images makes interpretation of reverse flow very rapid and easy. The pulse wave Doppler of a 4–7-MHz linear array transducer is ideal for examination of most of the veins. Reflux and obstruction involving superficial perforator and deep venous systems can be easily identified objectively and precisely localized [9].
Reflux is the predominant finding in patients with primary CVI. Apart from reflux, the morphological distortions of walls of the deep veins and the presence of collaterals would help to differentiate CVI from post-thrombotic pathology (Fig. 12.3). Reflux is confirmed by the use of provocation maneuvers, manual compression, and release or rapid inflation/deflation of cuff. Several workers have standardized the duration of pathological reflux in different venous segments. The current recommendations are as follows: for saphenous, tibial, deep femoral, and perforator reflux, the cutoff is 500 ms; for common femoral, femoral, and popliteal veins 1 s [9–11]. According to Abai and Labropoulos, for the perforators the cutoff time is 350 ms [9]. Nicolaides has summed up the duplex scan findings in CVI patients [4]:
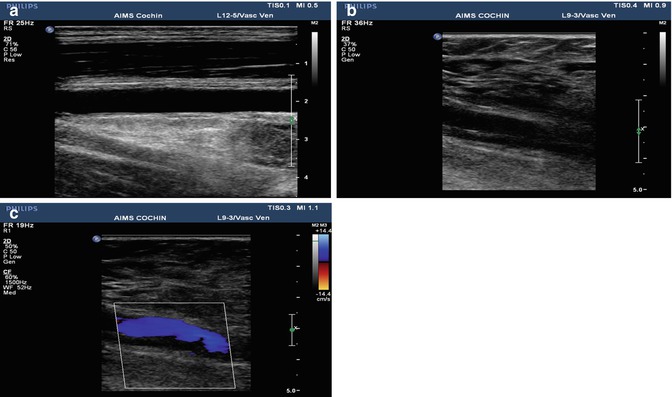
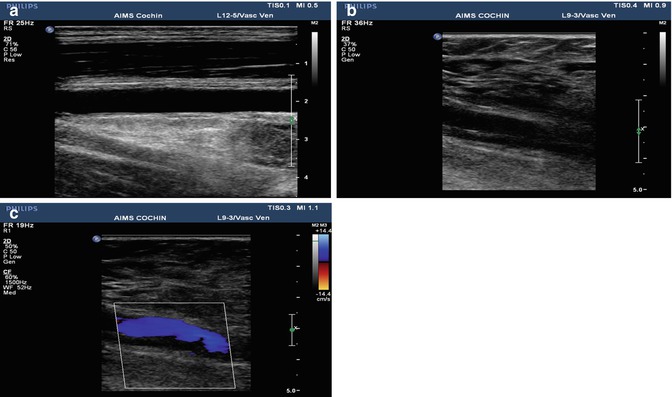
Fig. 12.3
Duplex scan findings in deep veins in primary CVI and post-thrombotic pathology. (a) Normal femoral vein showing smooth outline and flow. (b) Post-thrombotic vein showing wall irregularity and luminal membranes and filling defects. (c) Color coding demonstrating the irregular lumen
Multisegment reflux is more common in ulcerated limbs compared to non-ulcerated limbs (75 versus 22 %).
In two-thirds of patients with CVI, reflux was observed in two or more systems.
CVI is common when entire length of GSV is affected or when reflux is present in both GSV and SSV.
Reflux in the above-knee segments rarely cause ulcer in the absence of obstruction.
Two observations regarding reflux in deep veins in patients with CVI deserve attention. According to Lim and colleagues, deep vein reflux (DVR) to the level of knee and calf is associated with more severe disease irrespective of reflux in superficial veins [12]. The crucial factor in genesis of leg ulcer is the status of the popliteal vein valve. When this is competent, ulceration is rare, even with extensive disease. On the other hand, incompetence of this valve results in ulceration [13].
Duplex scan is helpful to some extent in differentiating between primary and secondary CVI. The morphological features of the deep venous system can be strikingly different in these two conditions. In primary CVI the deep veins are smooth, not scarred, and the lumen is totally free of any irregularities. In contrast, in post-thrombotic syndrome (secondary CVI) the deep vein walls can be irregular, scarred with multiple filling defect (Fig. 12.3). However, in some patients with PTS, the deep veins can still remain unscathed.
In our study of duplex scan in CVI patients, more than 50 % had reflux involving the superficial, deep, and perforator systems. In the deep veins the commonest location of reflux was in the femoral vein (85.41 %) followed by the popliteal vein (41.7 %). In the clinical class C1 to C3, the incidence of deep vein reflux was 27.1 %; in the C4 class it was 31.3 % and in the C5–6 class 41.7 %. All patients had reflux in the superficial venous system.
Plethysmographic Studies
Plethysmographic studies are generally complementary to duplex scans [11]. Photoplethysmography (PPG) was used to detect reflux. It is useful in assessing the effect of different modalities of treatment. The technique is not useful in localizing lesions. A more advanced technique, quantitative digital PPG is used to assess calf muscle pump function and venous outflow obstruction [4]. Air plethysmography (APG) is based on the measurement of changes in the limb volume by displacement of air in the cuff. It is useful to assess reflux, obstruction, and also evaluation of muscle pump function [4]. This is recommended in the evaluation of patients with advanced CVD, if duplex scan is inconclusive [11]. Ambulatory strain gauge plethysmography measures calf volume changes with exercise by using a strain gauge [4]. It is used to assess muscle pump function in terms of reflux and expelled volume [4].
Venography
Contrast venography provides information on the morphology of the venous system. Ascending venography was the gold standard investigation but is now mostly replaced by duplex scan. In a patient with CVI, ascending venogram is useful to rule out post-thrombotic pathology [4]. Some surgeons recommend this prior to valve reconstruction in deep veins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


