Fig. 6.1.
The Haller index is the transverse chest diameter divided by the anterior–posterior diameter on CT. This patient had a Haller index of 12 before undergoing surgery.
Management: surgery (gold standard).
Aim: produce superior cosmetic results with alleviation of the physiologic effects.
Indications: severe, progressive or symptomatic disease, compromised pulmonary physiology, Haller index >3.25 and compression on the heart impairing cardiac function [5]
Ravitch repair—open repair:
Resection of abnormal costal cartilages
Correcting the posterior displacement of the sternum
Nuss procedure—minimally invasive technique using thoracoscopy to guide the retrosternal placement of a stainless steel bar that remains in place for 2–3 years (Fig. 6.2).
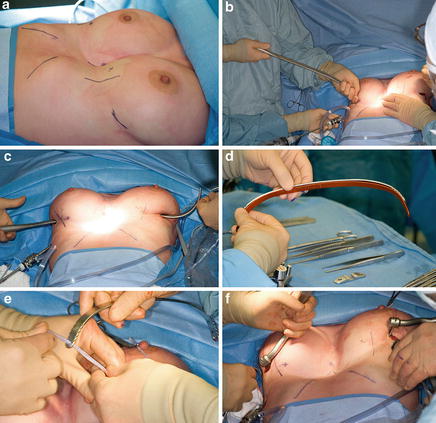
Fig. 6.2.
The Nuss procedure involves thoracosopic insertion of a steel bar retrosternally. (a) This patient had Pectus Excavatum (Haller index 12). (b, c) under thoracoscopic guidance, an insertion device is channelled underneath the sternum. (d–f) the bar (implant) is shaped intraoperatively according to the patient’s chest wall and passed through that same tract using an umbilical tape.
Preferred method over open repair
Complications (<5 %): bar displacement, bar allergy, pneumothorax requiring thoracostomy tube, and unsatisfactory cosmetic result. Very uncommon complications include cardiac injury and erosion into the sternum.
Both techniques have shown to improve pulmonary function tests (forced expiratory volume in 1 s, forced vital capacity, vital capacity, total lung capacity) after 1 year, with a greater improvement using the Nuss technique following bar removal [6].
Pectus Carinatum
Anterior protrusion of the sternum
Unlike Pectus Excavatum, it is more likely to present in later childhood and with pain.
Surgical repair involves subperichondrial resection of the costal cartilages involved with sternum osteotomy depending on the type of deformity.
Some success reported using orthotic bracing in younger children, despite poor compliance.
Sternal Defects: Deformities occurring as a result of the failure of fusion of the sternum during development
Sternal Cleft:
Normal overlying skin, with normal heart position
Repaired in early infancy using direct closure
Ectopia Cordis (“Herniated Heart”):
Heart protrudes anteriorly without any overlying tissue
Cervical Ectopia Cordis: significant protrusion of the heart, occasionally fused to the head
Cantrell’s Pentalogy (Thoracoabdominal Ectopia Cordis):
Sternal cleft, diaphragmatic defect (absence of septum transversum), pericardial defect, epigastric omphalocele and cardiac anomaly. The heart is covered by a thin membrane and often displaced into the abdomen through the diaphragmatic defect.
Poland’s Syndrome
Hypoplasia of the pectoralis major and minor, associated with syndactyly or brachydactyly
Mostly unilateral, with occasional involvement of the breast (amastia and athelia)
Increased rates of childhood leukaemia [7]
Surgical repair is indicated when there is underlying chest wall deformity leading to functional deficit.
Primary Chest Wall Tumours
Rare and highly heterogeneous group of tumours (Table 6.1).
Table 6.1.
Chest wall tumour: differential diagnosis.
Primary
Benign
Malignant
Bone
Ostoblastoma
Ewing sarcomaa (8–22 %)
Osteoid osteoma
Osteosarcomaa (10 %)
Cartilage
Chondromaa
Chondrosarcomaa (20 %)
Osteochondromaa
Fibrous tissue
Fibrous dysplasiaa
Fibrosarcoma
Desmoid tumoura (fibroma)
Vascular
Hemangioma
Hemangiosarcoma
Adipose tissue
Lipoma
Liposarcoma
Muscle
Leiomyoma
Leiomyosarcoma
Rhabdomyoma
Rhabdomysarcoma
Nerve
Neurofibroma
Neurofibrosarcoma
Schwannoma
Malignant schwannoma
Neuroblastoma
Miscellaneous
Solitary plasmacytomaa (10–30 %)
Lymphomaa (Hodgkin, non-Hodgkin)
Leukaemia
Secondary
Metastasis or local invasion from adjacent organs:
Breast, melanoma, lung, thyroid, mesothelioma, renal cell
Clinical Presentation
Majority present with a palpable (60 %), enlarging, hard and painful mass; minority (<30 %) are asymptomatic, most of which are benign [9].
Pain (40 %) occurs as a results of periosteal or neural invasion.
Growth rate is dependent on tumour type.
Metastasis or local invasion from a secondary lesion are more common and should be ruled out.
Workup
Imaging: MRI, CT, PET-CT
CT with IV contrast provides considerable detail regarding size, location, local invasion, involvement of other structures, and metastatic spread (Fig. 6.3).
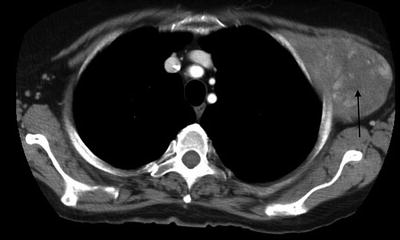
Fig. 6.3.
CT image of a chest wall tumour (black arrow).
MRI provides better resolution, anatomic delineation of the tissue planes and characterization of soft-tissue masses.
Mostly performed for tumours in the thoracic inlet and extremities.
PET-CT provides additional accuracy for diagnosis and staging, but its role has yet to be established.
Tissue diagnosis will allow for appropriate staging of the primary tumour and subsequent management. This is normally done using either core needle biopsy or excisional biopsy. Incisional biopsies can be performed for larger tumours, without compromising subsequent resection.
Management
The majority of tumours with no metastasis are treated with wide resection with or without reconstruction.
The role of chemotherapy or radiotherapy is highly dependent on the specific histopathology.
Outcomes after surgical resection show a 1-, 5- and 10-year survival of 90, 60 and 50 %, respectively [10].
Recurrence occurs in 50 %, with a 5-year survival of 17 %, depending on the primary tumour [10].
Benign tumours:
The majority are treated with wide-resection.
Desmoid tumours: locally aggressive and invasive with a high recurrence rate (25–75 %) [11, 12].
Positive margins have a 90 % 5-year probability of developing recurrence compared to 18 % with negative margins [13].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


