Fig. 7.1.
Patient presenting with a traumatic pneumothorax after blunt trauma to the chest. Black arrows denote the outline of the collapsed lung.
Massive air leak suggests injury to major airways.
Penetrating: Air enters the pleural cavity either directly through the wound in the chest wall or from a parenchymal laceration caused by the injury.
Blunt: Parenchymal laceration secondary to an associated injury (rib fracture, bronchial rupture, alveolar rupture).
• Open Pneumothorax (Sucking Chest Wound):
Air enters the pleural cavity through the chest wall defect with inspiration, thereby eliminating the pressure gradient between the pleural cavity and alveoli.
Should be initially covered with a 3-way occlusive dressing, followed by tube thoracostomy and an occlusive dressing.
Diagnosis
Pleuritic chest pain and dyspnea are the most common symptoms.
On primary survey, several signs are indicative of a pneumothorax, including decreased or absent breath sounds, subcutaneous emphysema (Fig. 7.2), and hyperresonance. A tension pneumothorax may also present with tracheal deviation to the contralateral side, severe respiratory distress, and hemodynamic instability.

Fig. 7.2.
Significant subcutaneous emphysema seen on the chest X-ray of a patient with a pneumothorax after blunt trauma to the chest.
Diagnosis is established by an upright chest X-ray. If clinical signs of tension physiology are evident, X-ray confirmation should be omitted and immediate decompression should ensue, followed by a chest tube.
An expiratory view accentuates the separation of the parietal and visceral pleura.
Pneumothorax in supine patients accumulates into the dependent regions of the anterior and subdiaphragmatic pleura and may be detected as a deep sulcus sign.
CT scan is the gold standard for diagnosis and can detect occult pneumothoraces undetected by chest radiograph.
Management
Management depends on the clinical setting, mechanism of injury, size of the pneumothorax, and associated conditions. Advanced Trauma Life Support (ATLS) guidelines should be followed for all trauma patients [3].
The appropriate initial diagnostic tests and management options should be tailored to the presentation of the patient:
Hemodynamically unstable patients with clinical signs of a pneumothorax should have a large-bore chest tube placed as part of the primary survey (with or without needle decompression preceding it for suspected tension pneumothorax).
For patients who are stable, imaging studies can confirm the diagnosis prior to definitive management.
Observation:
Reserved for asymptomatic patients with small or occult pneumothoraces who are unlikely to have an ongoing air leak. Follow-up radiography should be obtained at 3 h to document improvement or to make sure there is no worsening.
Supplemental oxygen can help decrease the concentration of nitrogen in the body, thus creating a gradient to drive the air in the pleura (mostly composed of nitrogen) into the body.
Percutaneous Catheters:
Small- to medium-calibre tube thoracostomy can be performed percutaneously via the Seldinger technique and attached to either a Heimlich one-way valve or a suction.
Use is limited to a pneumothorax with small or no associated hemothorax.
Tube Thoracostomy:
Large-bore chest tubes are the standard of care for treatment of traumatic pneumothoraces, unstable patients, persistent or large air leaks, and associated effusions or hemothoraces.
Hemothorax
Mechanism and Pathophysiology
Abnormal presence of blood in the pleural cavity.
Significant hemothorax may be caused by injury to the great vessels, heart, lung parenchyma, or chest wall/intercostal vessels, secondary to either blunt or penetrating injury.
Diagnosis
Clinical presentation and diagnosis are similar to pneumothorax, except for dullness to percussion.
Upright chest X-ray will confirm the diagnosis if >300 mL of blood is present (Fig. 7.3).
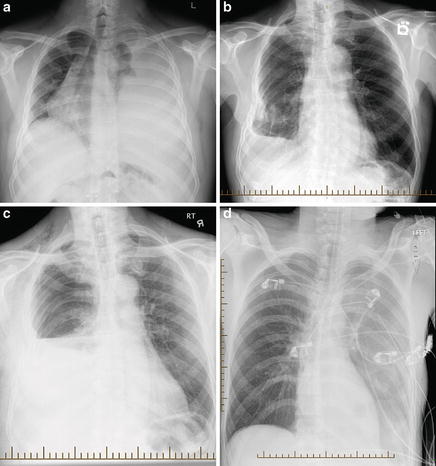
Fig. 7.3.
Traumatic hemothorax diagnosed on chest X-ray. (a) Patient presenting with a massive left hemothorax after blunt trauma to the chest. The mediastinal structures, including the heart, trachea, and major airways, are shifted to the right. Typically blood can be identified on upright chest X-ray (b, c); however this may not always be the case if the patient is supine (d).
Hemodynamically unstable patients with signs of pneumohemothorax require immediate decompression without imaging.
Management
ATLS protocols should be followed, starting with a primary and secondary survey.
Goal is complete removal of all blood. Residual blood is a nidus for the development of empyema and fibrothorax, which can also occur due to improper positioning or obstruction of the chest tube [4].
If this is not feasible with one chest tube, residual blood can either be removed by additional chest tube(s) or surgically (thoracoscopically if patient is clinically stable).
Posttraumatic empyema can also occur secondary to a foreign body, lung abscess, bronchopleural fistula, esophageal perforation, or an abdominal source [5]. See Chap. 4 : Pleural Disorders (Empyema).
Tube thoracostomy is initially performed using a 32–36 French chest tube.
Indications for thoracotomy:
Hemodynamic instability
>1,500 mL of blood drains initially upon insertion of chest tube
Persistent bleeding of >200 mL/h for 4 h
Chest Wall Injuries
The types of chest wall injuries vary depending on the mechanism of trauma, force of injury, and the patient’s characteristics. Certain injuries such as fractures of the first rib, sternum, scapula, lower ribs, and bilateral ribs are associated with other life-threatening injuries.
Rib Fractures:
Mechanism and Pathophysiology:
Most common injury following blunt chest trauma (30–40 % of all thoracic trauma) [6].
Physiologic sequelae of rib fractures are related to their impact on normal pulmonary mechanics mostly due to significant pain, causing decreased ability to cough, reduced lung volumes, and an increased risk for pneumonia.
This is especially true for the elderly who have reduced chest wall compliance, reduced bone density, and higher incidence of underlying lung disease [7].
Flail Chest: Occurs when three or more adjacent ribs are fractured in two places (Fig. 7.4). The most common mechanism is direct-impact injury (e.g., steering wheel).
Fig. 7.4.
Patient presenting with multiple rib fractures, sternal fracture, flail chest, and associated lung injuries (bilateral pneumohemothoraces and pulmonary contusions) after a crush injury to the chest. Subcutaneous emphysema can be seen throughout the anterior and lateral chest wall.
Leads to severe disruption of lung mechanics with paradoxical motion during breathing, placing patients at very high risk of respiratory failure. Patients also often have severe pulmonary contusions.
Paradoxical motion may not be obvious during positive-pressure ventilation.
Management
Aggressive pain control is fundamental in managing rib fractures and improving lung mechanics. For limited rib fractures (≤3) in healthy young adults, this might be the only necessary management and can be carried out as an outpatient.
Various methods available: regional anaesthesia, epidural infusion, paravertebral block, intrapleural infusion, patient-controlled analgesia pumps, oral or intravenous narcotics, and nonsteroidal anti-inflammatories.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


