Chapter 6 Chest Radiography
Skilled interpretation of chest radiographs is central to the diagnosis and treatment of patients in the cardiothoracic intensive care unit (ICU). In this chapter the common abnormalities of chest radiographs that are encountered in cardiac surgery patients are reviewed. Where appropriate, indications for computed tomography (CT) or ultrasound scanning of the chest are discussed. Before attempting to interpret abnormalities, it is essential to appreciate the findings of the normal chest radiograph and to have a systematic approach to reviewing films. These topics are discussed first.
NORMAL CHEST RADIOGRAPH
Types of Chest Radiographs
Two types of frontal chest radiographs may be obtained:
Normal Structures on the Erect Posteroanterior Chest Radiograph
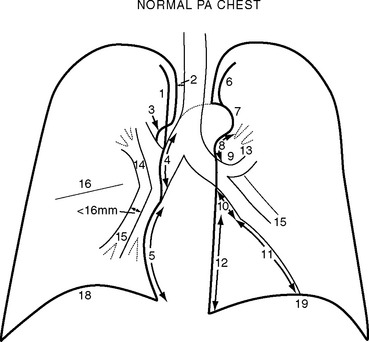
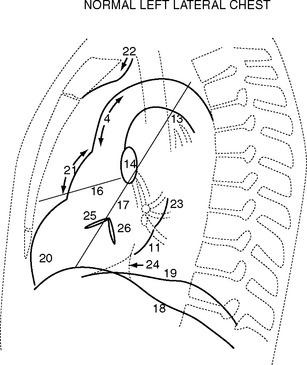
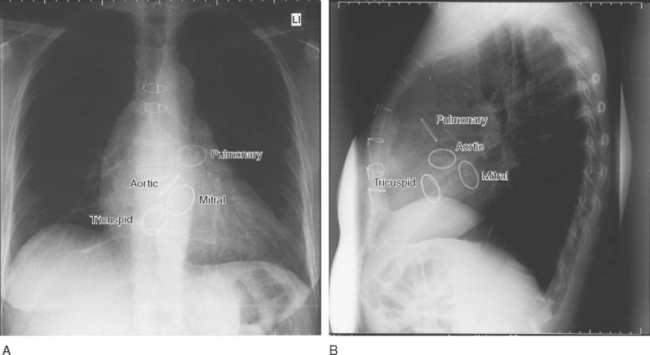
Normal structures identified on the PA and left lateral radiographs are shown in Figs. 6-1 and 6-2.
Systematic Approach to Examining Chest Radiographs
PREOPERATIVE CHEST RADIOGRAPH
Cardiac Chamber Enlargement
The PA and lateral chest radiographs can suggest specific valvular or chamber abnormalities.
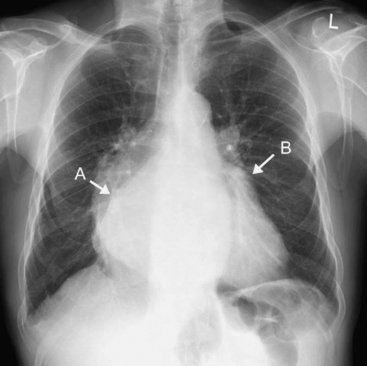
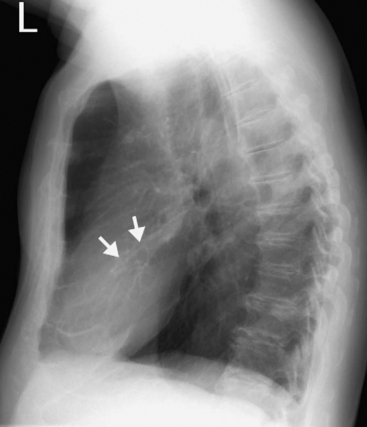
Left Atrial Enlargement
Radiographic signs of left atrial enlargement include (Fig. 6-3):
Right Ventricular Enlargement
Right Atrial Enlargement
Cardiac Calcification
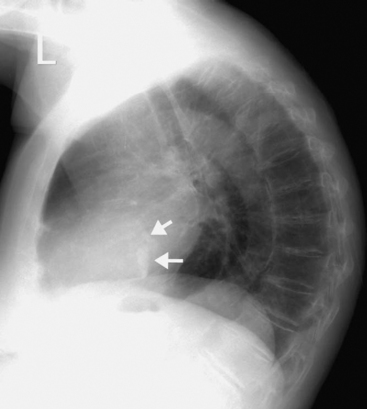
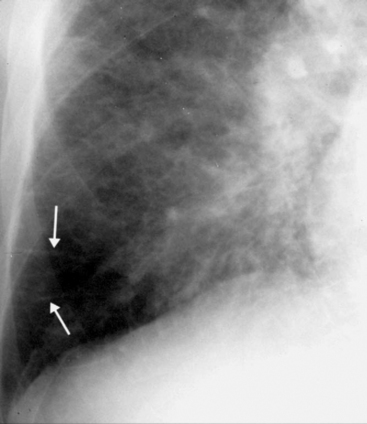
Calcification can be present in many cardiac structures, including the pericardium, the cardiac valves, and the walls of the cardiac chambers, as well as in organized thrombus and in the coronary arteries due to atheroma. Aortic valve calcification can be seen on the lateral radiograph as a ring of calcification projected centrally over the heart (Fig. 6-4). The presence of aortic valve calcification implies stenosis. Mitral annular calcification is common in patients more than 70 years of age; it appears as a C-shaped ring near the posterior and inferior aspects of the heart on the lateral radiograph (Fig. 6-5). Mitral annular calcification does not imply functional impairment of the mitral valve. In contrast, calcification of the mitral leaflets is associated with rheumatic heart disease and usually indicates significant mitral valve dysfunction, usually stenosis. Mitral leaflet calcification is seen in the same region as annular calcification but is punctate and lacks the C-shape of the more benign annular calcification. The positions of each of the four heart valves on frontal and lateral radiographs are shown in Figure 6-6.
Hiatus Hernia
Hiatus hernia results in a retrocardiac mass that is predominantly left-sided but can bulge slightly to the right of the midline on a frontal radiograph. Such hernias are common and are best appreciated on an erect chest radiograph, on which they can usually be seen to contain an air fluid level. On a supine film, a hiatus hernia may be mistaken for a left basal pneumothorax.
Pulmonary Vascularity
Pulmonary Arterial Hypertension
Signs suggestive of pulmonary arterial hypertension include:
On thoracic CT, the signs of pulmonary arterial hypertension include a transverse diameter of the main pulmonary artery greater than that of the adjacent ascending aorta as well as the presence of pericardial fluid and minor pericardial thickening.1
Pulmonary Venous Hypertension and Pulmonary Edema
Three changes in pulmonary vascularity occur in patients with raised left atrial pressure:
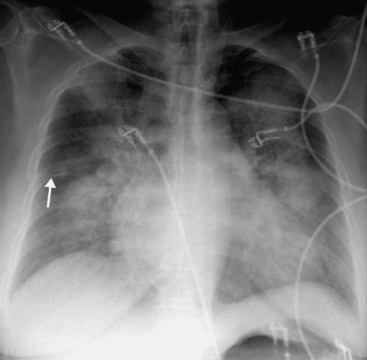
Figure 6.8 AP radiograph, patient erect, showing alveolar pulmonary edema. The perihilar and symmetric nature of the infiltrates favors a diagnosis of alveolar pulmonary edema over ARDS (see Fig. 6-17). Interstitial fluid, as demonstrated by the thickening of the horizontal fissure (arrow), can also be seen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree