CARDIOVASCULAR IMAGING AND STRESS TESTING
CHAPTER

Chest Radiography for the Cardiovascular Medicine Boards
Despite continuing advances that have greatly expanded the ability to assess cardiovascular anatomy noninvasively through an array of imaging modalities, chest radiography (CR) remains a very useful part of the initial cardiovascular evaluation. CR is widely available, can be acquired rapidly and inexpensively, and has a low associated ionizing radiation dose. With an organized approach toward interpretation, and insight into the strengths and limitations of CR, the cardiologist can maximize the use of this tool in clinical practice. This chapter focuses on the most important components of the CR with regard to cardiovascular disease, namely:
1. Pulmonary vascular patterns
2. Cardiomediastinal silhouette
3. Calcification patterns
The following radiographs illustrate the appearance of a variety of cardiac abnormalities. Whenever possible, tables are included to delineate the differential diagnoses for representative chest radiographic findings.
BASIC APPROACH AND PROJECTIONS
Understanding the strengths and weaknesses of CR techniques is helpful in both the selection and interpretation of exam. Standard CR techniques include erect posteroanterior (PA) and lateral projections. In patients unable to stand for an erect PA, an anteroposterior (AP) radiograph can be performed. Additional specialized CR techniques exist, though their utilization is limited with widespread availability of tomographic imaging. The erect PA and lateral technique hold several advantages, as AP technique will magnify car- diomediastinal structures, and the ability to interpret pulmonary vasculature correctly is limited in supine patients. Additionally, more standardized techniques of acquisition are often used with PA radiographs, allowing for more reliable comparison between radiographs. Benefits of portable radiographs include the speed and convenience of obtaining a radiograph without transporting a patient.
Interpretation of radiographs can be aided by an ordered approach. Identification of the patient’s name and date of the examination is a straightforward but important step and can save further confusion or wasted time when checked first. Visible medical devices (catheters, drains, and other support devices) should be assessed to confirm position and any associated complication. When prior CRs are available, they should be assessed concurrently to help detect new abnormalities or to confirm the stability of a long-standing finding.
The three aforementioned components, pulmonary vasculature, cardiomediastinal silhouette, and calcifications, can then be reviewed in any order. Changes in each of these central components are a direct manifestation of the underlying cardiovascular disorder; and taking all three of these components into account ensures an appropriate, systematic approach to the standard CR. Other elements of CR interpretation are important (such as appropriate technique, assessment of pulmonary parenchyma) and have important clinical implications; however, we focus our discussion toward the elements most helpful in depiction of cardiovascular disease.
PULMONARY VASCULAR PATTERNS
Pulmonary Vascular Patterns in Normal and Various Cardiovascular Disease States
1. Normal
 In normal patients, the vessels in the upper zones are thinner than those at a similar distance from the hilum in the lower zones (normal ratio 1:3)
In normal patients, the vessels in the upper zones are thinner than those at a similar distance from the hilum in the lower zones (normal ratio 1:3)
 Pulmonary artery (PA)/pulmonic valve obstruction (no shunt or pulmonary hypertension)
Pulmonary artery (PA)/pulmonic valve obstruction (no shunt or pulmonary hypertension)
 Aorta/aortic valve (AV) obstructions (no shunt, left ventricular compromise, mitral valve disease)
Aorta/aortic valve (AV) obstructions (no shunt, left ventricular compromise, mitral valve disease)
 Insignificant left-to-right shunt: Qp/Qs< 1.5
Insignificant left-to-right shunt: Qp/Qs< 1.5
2. Increased (overcirculation)
 Significant left-to-right shunt: Qp/Qs>1.5 (acyanotic)
Significant left-to-right shunt: Qp/Qs>1.5 (acyanotic)
 Atrial septal defect (ASD)
Atrial septal defect (ASD)
 Ventricular septal defect (VSD)
Ventricular septal defect (VSD)
 Patent ductus arteriosus
Patent ductus arteriosus
 Partial anomalous pulmonary venous return
Partial anomalous pulmonary venous return
3. Decreased (undercirculation)
 Right-to-left shunt
Right-to-left shunt
 Tetralogy of Fallot
Tetralogy of Fallot
 Ebstein anomaly with ASD
Ebstein anomaly with ASD
 Pulmonary oligemia
Pulmonary oligemia
 Ebstein anomaly (severe ± ASD)
Ebstein anomaly (severe ± ASD)
4. Admixture shunt (no pulmonic stenosis or atresia/cyanotic)
 Transposition complexes
Transposition complexes
 Truncus arteriosis
Truncus arteriosis
 Univentricular heart (single ventricle)
Univentricular heart (single ventricle)
 Total anomalous pulmonary venous return: types I and II
Total anomalous pulmonary venous return: types I and II
 Tricuspid atresia + VSD
Tricuspid atresia + VSD
5. High-output states
 Anemia
Anemia
 Pregnancy
Pregnancy
Decreased Pulmonary Blood Flow (Fig. 8.1)
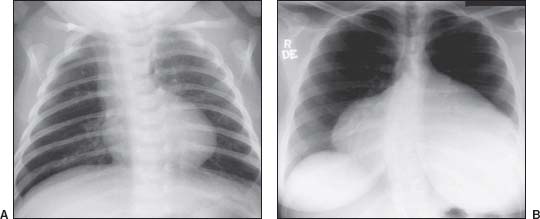
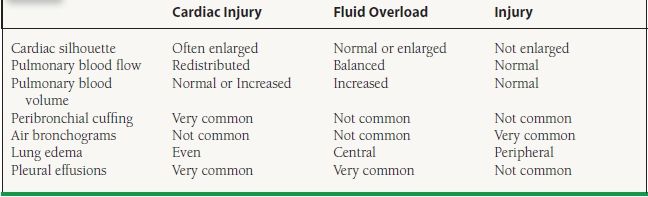
FIGURE 8.1 Decreased pulmonary blood flow. A: Tetralogy of Fallot. B: Ebstein anomaly.
Increased Pulmonary Blood Flow (Fig. 8.2)
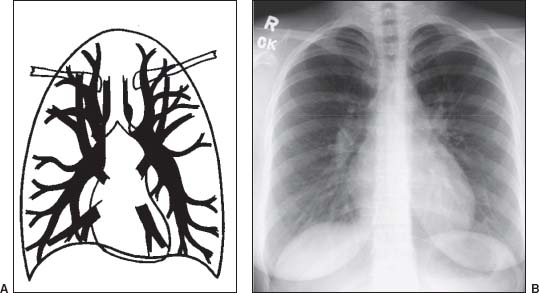
FIGURE 8.2 Increased pulmonary blood flow. A: Increased: balanced (overcirculation). B: ASD
Increased distributed (Fig 8.3)
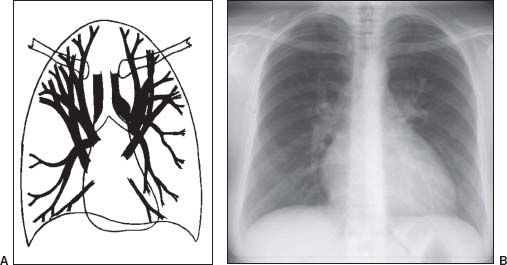
FIGURE 8.3 Increased: redistributed. A: Pulmonary venous hypertension (PVH). B: Hypertrophic cardiomyopathy (HCM) PVH.
Pulmonary Arterial Hypertension (PAH)
Causes of PAH
 Precapillary: pulmonary hypertension (both primary and pulmonary hypertension associated with hepatic disease, drugs/toxins, HIV), congenital cardiovascular disease, chronic thromboembolism, chronic alveolar hypoxia (COPD, interstitial lung disease, hypoventilation)
Precapillary: pulmonary hypertension (both primary and pulmonary hypertension associated with hepatic disease, drugs/toxins, HIV), congenital cardiovascular disease, chronic thromboembolism, chronic alveolar hypoxia (COPD, interstitial lung disease, hypoventilation)
 Postcapillary: left sided cardiovascular disease, mitral stenosis, aortic valve disease, cardiac tumors, extrinsic pulmonary venous compression, fibrosing mediastinitis, pulmonary venoocclusive disease
Postcapillary: left sided cardiovascular disease, mitral stenosis, aortic valve disease, cardiac tumors, extrinsic pulmonary venous compression, fibrosing mediastinitis, pulmonary venoocclusive disease
Increased: Central (Fig. 8.4)
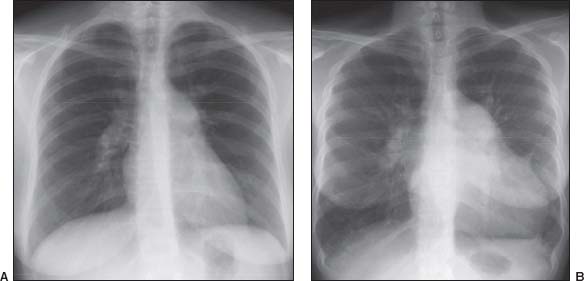
FIGURE 8.4 A: Idiopathic (pre-capillary) PAH; B: Post-capillary PAH.
Pulmonary Venous Hypertension
Stages of PVH
Stage 1: Pulmonary vascular redistribution
PCWP: Acute, 13 to 18 mm Hg; chronic, 18 to 22 mm Hg
Stage 2: Redistribution + interstitial pulmonary edema
PCWP: Acute, 18 to 25 mm Hg; chronic, 23 to 30 mm Hg
Stage 3: Redistribution + interstitial and alveolar pulmonary edema
PCWP: Acute, >25 mm Hg; chronic, >30 mm Hg>
Causes of PVH
Pulmonary venoocclusive disease
Pulmonary vein stenosis (postradiation therapy, post–atrial fibrillation ablation)
Left atrial/left ventricular obstruction
Myxoma or other tumors
Mitral valve disease
Mitral stenosis
Mitral regurgitation
Left ventricular compromise
Dilated cardiomyopathy
Acute or chronic myocardial ischemic disease
Restrictive cardiomyopathy
Pericardial disease
Constrictive pericarditis
Pulmonary Edema Patterns
Increased hydrostatic pressure gradient
Increased capillary permeability
Decreased osmotic pressure gradient
Lymphatic incompetence
TABLE
8.1 Radiographic Features of Different Types of Pulmonary Edema