History (angina or anginal equivalent)
Acute ischemic electrocardiogram (ECG) changes
Typical rise and fall of cardiac markers
Absence of another identifiable etiology
Occurring at rest or with minimal exertion and usually lasting >20 minutes (if not interrupted by nitroglycerin)
Severe pain of new onset (i.e., <1 month)
Occurring with a crescendo pattern (i.e., more severe, prolonged, or frequent than previously)
No evidence of myocardial infarction by biomarkers
Ischemic symptoms
Development of pathologic Q waves on the ECG
ST elevation, depression or evolutionary EKG changes consistent with ischemia
Post PCI (CK-MB 3× upper limit of normal)
Normal male pattern: Often with 1-3 mm of concave sinus tachycardia (ST) elevation greatest lead V2
Early repolarization: Often with 1-3 mm of concave ST elevation, often with notching at the J point in V4
Variant ST elevation with T wave inversion: Seen often in young black men, convex ST elevation, T wave inversion, thought to represent persistent juvenile T wave inversion + early repol, may look like STEMI
Left bundle branch block (LBBB): Typical pattern of LBBB present with anterior ST elevation
Pericarditis: Diffuse ST elevation and PR depression, PR elevation in AVR, the ratio of ST elevation: T wave height (> 0.25 measured using PR segment as the baseline in this case) in V6 is highly sensitive and specific for the diagnosis of pericarditis
Left ventricular hypertrophy with strain
Hyperkalemia: Downsloping ST elevation associated with wide QRS, peaked T waves
Pulmonary embolism: Sinus tachycardia, often anterior T wave inversions
Takotsubo cardiomyopathy (apical ballooning syndrome)
Brugada syndrome: Right bundle, downsloping ST elevation >2mm isolated to V1 and V2
TABLE 3-1 Immediately life-threatening causes (must consider these every time) | |||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 3-2 Urgent causes | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 3-3 Other causes | |||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||
Takotsubo cardiomyopathy (apical ballooning syndrome)
Coronary vasospasm (Prinzmetal angina)
Coronary dissection
Severity: The 1-10 scale is useful, functional limitations should be sought
Onset: Be specific, can affect decisions about thrombolysis and PCI
Character: Pressure versus sharp, pleuritic, tearing (aortic dissection)
Radiation: Shoulder, jaw, arm, back
Associated symptoms: shortness of breath (SOB), nausea/vomiting (N/V), palpitations, syncope
Tempering factors: Rest, particular position (pericarditis—relief sitting forward)
Exacerbating factors: Exertion, emotional state versus particular position
Self assessment: Knowing the patient’s fears is important for many reasons
Also look for history of CAD, details of prior angiography, CABG or percutaneous coronary intervention (PCI), recent stress tests or echoes, other risk factors (DM, smoking, HTN, hyperlipidemia, cocaine use)
Hypotension/hypertension
Arrhythmias
Tachypnea or hypoxia
Fever
Bilateral SBP difference >15 mm Hg (think of aortic dissection)
Asymmetric pulses and/or a focal neurologic exam (aortic dissection)
Signs of heart failure (elevated JVP, S3, crackles, hemoptysis)
New MR murmur (? papillary muscle ischemia)
A new S4 in a patient with active CP is highly suggestive of ischemia
Murmur of aortic stenosis, pulsus parvus et tardus
Abdominal tenderness (biliary tract/pancreatic disease)
Rectal exam—evaluate for melena or guaiac positive stool (? how aggressive to anticoagulate)
Rash on the chest (Zoster), make sure to examine the chest on hospital day 2, the pain often precedes the skin findings!
Troponin I or T may be detectable as early as 2 hours after injury and CK-MB become detectable around 6 hours and are most sensitive at 10 hours
Myoglobin may rise somewhat sooner but is nonspecific
Must obtain serial tests q4-6 h for at least 10 hours after the start of CP to definitively r/o MI
False positive in heart failure, significant hypertension, PE
Look for typical rise and fall of enzymes in the context of CP and the ECG to make a diagnosis of NSTEMI
Heart failure can be responsible for persistent low-grade elevation of troponin thought to be from elevated LVEDP leading to subendocardial necrosis often with normal CKs
WBC: Likely mildly elevated in AMI but may also establish infectious etiology for current state
Hemoglobin: Anemia contributes to patients presenting with shortness of breath or angina
Platelets: Severely depressed <50k levels may be a contraindication to PCI
Electrolytes: Monitor for potassium and calcium abnormalities which may alter the ECG, Evaluate for infectious etiologies, electrolyte abnormalities
contributing to arrhythmias, biliary tract disease, or pancreatitis, if indicated
Creatinine: Usually elevated in patients with longstanding HTN and DM. Elevated creatinine is a relative contraindication to angiography because of the risk of renal failure secondary to contrast nephropathy
LFTs: Elevated in cases of hypotension due to shock or passive congestion due to elevated right-sided filling pressures. Also serum glutamic oxaloacetic transaminase/aspartate aminotransferase (SGOT/AST) can be elevated from an acute coronary syndrome as it is released from myocardial necrosis
Urine toxicology: Should be obtained for all young or at-risk patients with concerning chest pain (cocaine-induced MI can result from thrombosis in addition to vasospasm and therefore reperfusion may be indicated)
B-type natriuretic peptide (BNP): May be helpful in establishing the diagnosis of congestive heart failure (CHF) (see chapter on complications of AMI)
Should be obtained within 5 minutes of arrival within the emergency department
Make sure to label each ECG with the degree of pain
Comparison to an old ECG can be helpful
Repeat every 15 minutes ×2 if nondiagnostic, this has been shown to increase sensitivity
Dynamic T wave and ST changes should greatly increase your suspicion for ACS
Reoccurrence of CP should be re-evaluated with additional ECG recordings prior to giving NTG
Obtain right-sided leads in those with inferior distribution injury to evaluate for RV injury or infarct
Obtain posterior leads in patients with only anterior ST depression to r/o posterior wall STEMI
Assess for a widened mediastinum and always consider aortic dissection
Examine lung fields for evidence of a pneumonic process, pulmonary congestion, or pneumothorax
Assess ribs and soft tissues for evidence of trauma
Hypoxia/tachypnea with a clear CXR? Consider PE
Useful test for evaluating systolic function, regional WMAs, effusion, valvular lesions, and to assess for complications of MI
May be helpful in a high risk patient with ongoing CP and a nondiagnostic ECG or when the diagnosis of STEMI is in doubt
Used to assess for proximal PE and aortic dissection and to assess for other noncardiac etiologies of CP such as pneumonia or pulmonary mass
Sensitivity and specificity are institutional and reader dependent
Consider MRI if patient has CRI or is high risk for contrast nephropathy
Different phase of contrast often needed for optimal evaluation of PE and aortic dissection
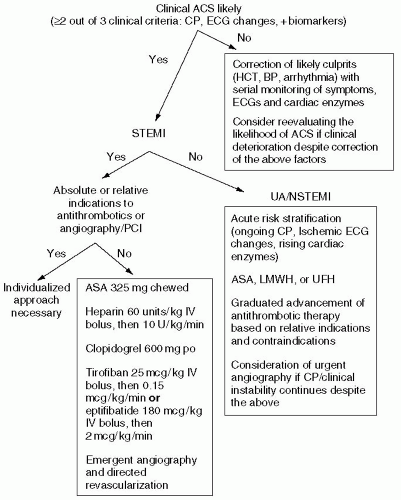
TABLE 3-4 TIMI risk score (TRS) for UA/NSTEMI11 | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 3-5 UA/NSTEMI ACS risk stratification | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 3-6 Immediate NSTEMI ACS treatment strategies checklist | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree