Cerebrovascular System
I. ANATOMY
A.
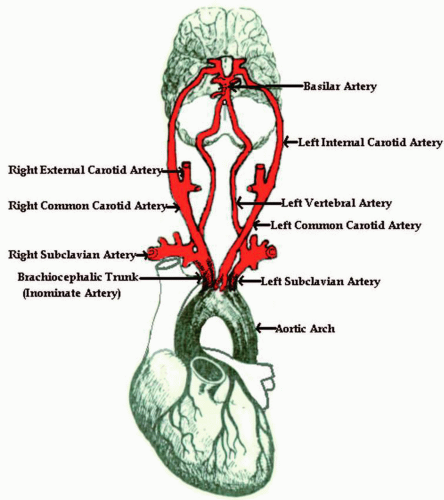
The common carotid artery (CCA) is 5 to 6 mm in size. The right CCA originates from the brachiocephalic artery, and the left CCA originates from the aortic arch. The CCA bifurcates into the internal and the external carotid arteries (Fig. 7.4). The carotid bulb is the enlarged portion of the distal CCA (or it can be part of the proximal internal carotid artery). This has baroreceptors that sense and regulate blood pressure.
B.
The internal carotid artery (ICA) is approximately 4 mm in size. It is usually located posterior and lateral to the external carotid artery (ECA), although 15% of the time this is reversed. This artery supplies the anterior brain, eyes, forehead, and nose. It enters the skull through the carotid canal. After passing into the skull, it gives off its first branch, the ophthalmic artery. After this branch, the ICA joins the circle of Willis, where it gives off the anterior choroidal and posterior communicating arteries before it finally divides into the anterior cerebral artery (ACA) and middle cerebral artery (MCA). The portions of the ICA are divided as follows:
1. Cervical—the longest portion
2. Petrous
3. Cavernous (“siphon”)—S-shaped, from whence the ophthalmic artery branches
4. Supraclinoid
C.
The ophthalmic artery is the first branch off the ICA. It has several branches:
1. Central retinal artery. This artery supplies the eye.
2. Supraorbital artery. This artery courses anterior and superior until it reaches the globe, then joins the ECA via the superficial temporal artery.
3. Frontal artery. This artery exits the orbit medially to supply the midportion of the forehead. It joins the ECA via the superficial temporal artery as well.
4. Nasal artery/angular artery. This artery branches off the frontal artery to supply the nose. As the angular artery, it courses down the lateral border of the nose. It joins the ECA via the facial artery.
D.
The external carotid artery is approximately 3 mm in size. It is usually located anterior and medial to the ICA. Unlike the ICA, it gives off branches right away. It has eight branches that supply the face, neck, tongue, thyroid gland, ear, scalp, and dura mater. The branches include: the ascending pharyngeal artery, superior thyroidal artery, lingual artery, posterior auricular artery, internal maxillary artery, superficial temporal artery, transverse facial artery, and the occipital artery.
E.
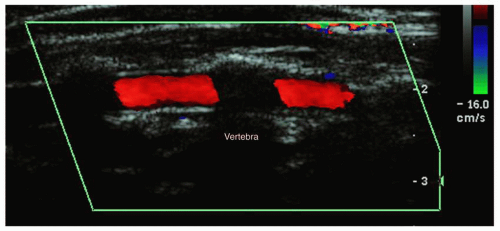
The vertebral artery originates from the subclavian arteries (Fig. 7.5). They are usually asymmetric in size, with the right usually being smaller than the left. They enter the vertebral space at the level of C6 and course through the foramina. They exit the vertebral foramina at the level of C1 and enter the skull through the foramen magnum to join together to form the basilar artery.
F.
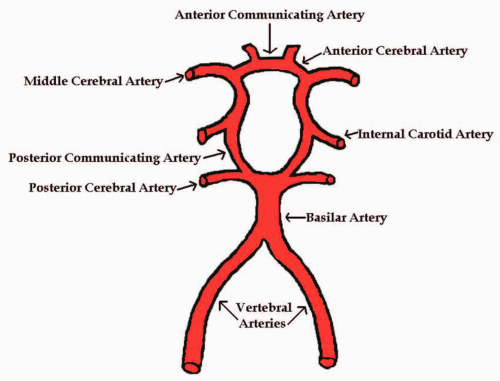
The circle of Willis (Fig. 7.6) is a circle of vessels that lie at the base of the brain connecting the anterior and posterior circulatory systems. There is a “normal” circle of Willis only 18% to 20% of the time. The most common variant is a hypoplastic ACA. The circle of Willis provides an important collateral pathway in cases of stenosis or occlusion. The circle of Willis is made up of:
1. Anterior cerebral artery —this artery carries 20% to 30% of the blood to the brain.
2. Middle cerebral artery—this artery carries 70% to 80% of the blood to the brain.
3. Posterior cerebral artery (PCA)
4. Basilar artery—this artery is formed by the vertebral arteries, and supplies blood to the posterior structures of the cranial cavity.
5. Distal ICA
6. Anterior communicating artery (ACA)
7. Posterior communicating artery (PCA)
G.
Nearly one sixth of the cardiac output is sent through the CCAs and the vertebral arteries. Approximately 75% of blood going to the brain is sent through the ICAs (each delivers 300-400 mL per minute). The other 25% of the blood going to the brain is sent through the vertebral arteries (each delivers 100 mL per minute).
H.
The brain’s blood supply is divided into two systems:
1. Anterior circulatory system. This system is made up of the carotid arteries and their branches.
2. Posterior circulatory system. This system is made up of the vertebrobasilar arteries and their branches.
I.
The major collateral pathways available for transfusion are:
1. Circle of Willis pathways include:
a. External to internal collateral via the ophthalmic artery (supraorbital artery to superficial temporal artery, frontal artery to superficial temporal artery, angular artery to transverse facial artery).
b. Crossover collateral via the ACA.
c. Posterior to anterior collateral via the PCA.
2. Intracranial to extracranial anastomoses include:
a. Connections via the ophthalmic and orbital arteries, the meningohypophyseal branches, and the carotid-tympanic branches.
b. Connections via the occipital branch of the ECA and the atlantic portion of the vertebral artery.
c. The ECA’s connections across the midline.
d. The deep cervical and ascending cervical branches of the subclavian artery to the branches of the lower
vertebral artery, the atlantic portion of the vertebral artery, and the occipital branch of the ECA.
vertebral artery, the atlantic portion of the vertebral artery, and the occipital branch of the ECA.
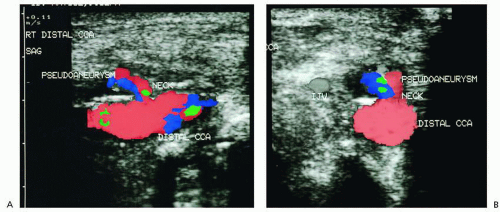
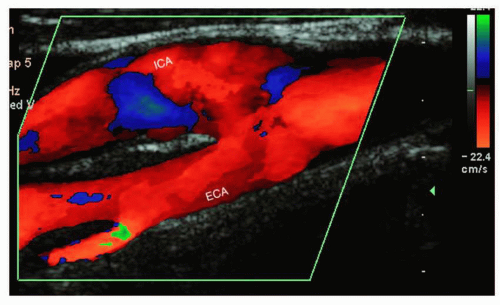 FIGURE 7.4. Sagittal color image of the internal (ICA) and external carotid arteries (ECA). (Image courtesy of Philips Medical Systems.) |
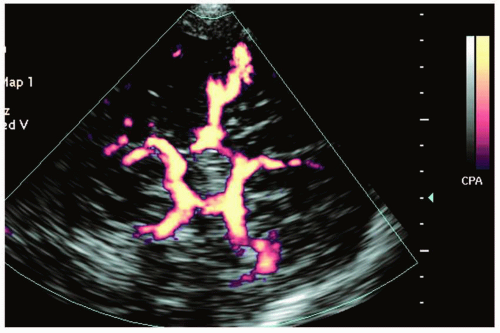 FIGURE 7.6. Color image of the circle of Willis using contrast enhancement. (Image courtesy of Philips Medical Systems.) |
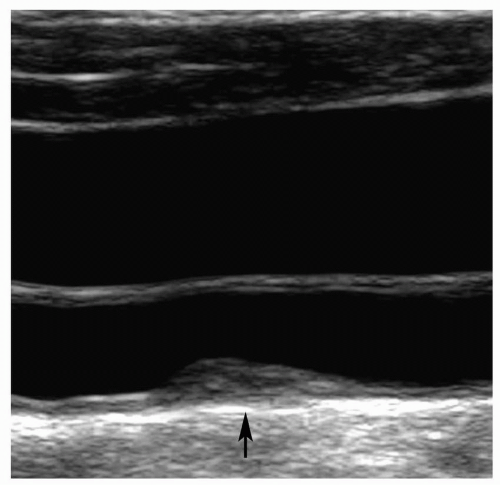 FIGURE 7.7. Sagittal gray-scale image of the common carotid artery with homogeneous fibrous plaque. (Image courtesy of Philips Medical Systems.) |
3. Small intraarterial communications.
II. PATHOLOGY
A. Arteriosclerosis
Arteriosclerosis is a number of pathologic conditions in which there is thickening, hardening, and loss of elasticity of the walls of the arteries.
B. Atherosclerosis
1. Atherosclerosis is a form of arteriosclerosis that is characterized by a variable combination of changes in the intima of the arteries. These changes include focal accumulation of: lipids or a lipid containing material (atheroma), complex carbohydrates, blood and byproducts, fibrous tissue, calcium deposits, smooth muscle cells, collagen, fibrin, and platelets. This is associated with changes in the media of the arteries.
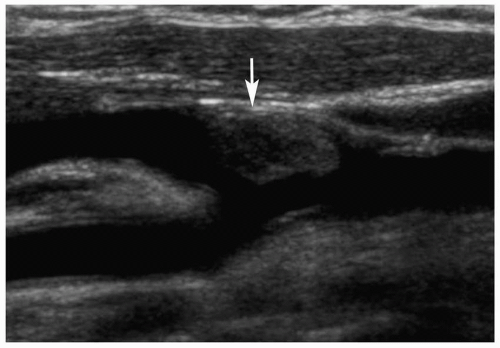 FIGURE 7.8. Sagittal gray-scale image of the carotid bulb with homogeneous fibrous plaque (arrow). (Image courtesy of Philips Medical Systems.) |
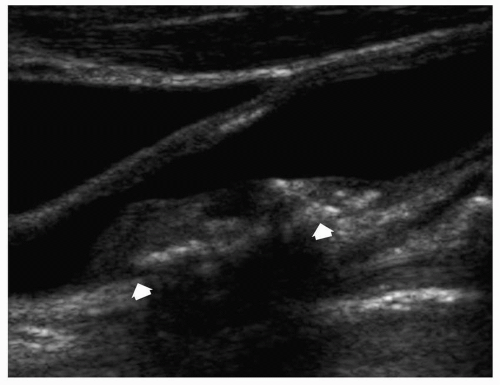 FIGURE 7.9. Sagittal gray-scale image of the internal carotid artery with heterogeneous complicated plaque (arrows). (Image courtesy of Philips Medical Systems.) |
2. Types of atherosclerotic plaque:
a. Fatty streak. A fatty streak is a thin layer of lipid material on the intima of the artery. It has low-level echoes and is homogeneous.
b. Fibrous plaque. Fibrous plaque is an accumulation of lipids, covered by additional lipid deposits, collagen, and elastic fibers. It has low- to mediumlevel echoes and is homogeneous (Figs. 7.7 and 7.8).
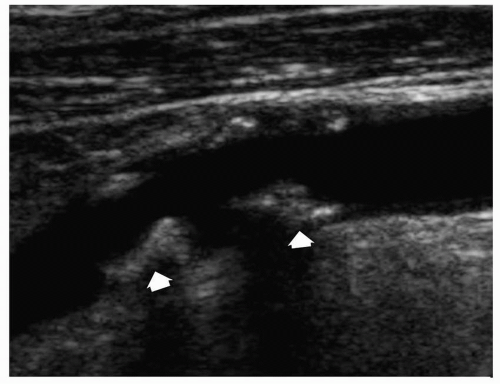 FIGURE 7.10. Sagittal gray-scale image of the internal carotid artery with heterogeneous complicated plaque (arrows). (Image courtesy of Philips Medical Systems.) |
c. Complicated lesion. This is fibrous plaque that has progressed to include fibrous tissue and additional collagen, as well as calcium and cellular debris. It is heterogeneous in appearance, and the calcium deposits have bright echoes with shadowing (Figs. 7.9 and 7.10).
d. Ulcerative lesion. This type of lesion occurs when the normally smooth surface of the fibrous cap has undergone deterioration. These may result in distal embolization. A focal indentation (possibly U shaped) or a break in the plaque’s surface is seen. There may be eddies of color within the plaque. Between 50% and 70% of patients with this type of plaque have hemispheric symptoms. All ulcerated lesions are associated with Intraplaque hemorrhage.
e. Intraplaque hemorrhage. This is seen as a sonolucent area within the plaque. There can be multiple sonolucent areas, giving a “Swiss cheese” appearance.
C. Mechanisms Involved in Cerebrovascular Disease:
1. Stenosis. This is a narrowing in the blood vessel caused by the processes of atherosclerosis.
2. Thrombosis. This is the formation of a blood clot. This is one of the most common causes of a stroke.
3. Embolism. This is a foreign substance or piece of thrombus (may be solid, liquid, or gas) that moves through the circulatory system until it becomes lodged in a distant blood vessel. This results in complete or partial obstruction of that vessel. The most frequent type of embolus is atherosclerotic plaque that breaks loose. A stenosis, thrombus, and embolus may all exist at the same time.
4. Aneurysm. This is an abnormal dilatation of the wall of a vessel. They rarely occur in the cervical carotid artery. They are due to congenital defects, or weakness of the wall from trauma, atherosclerosis, or infection.
5. Nonatherosclerotic disease. This includes:
a. Dissection of the intima can be caused by trauma. It may also occur spontaneously in a patient with atherosclerotic disease. This shows up as a mobile or fixed echogenic flap. It may or may not have thrombus formation. It may cause occlusion (Fig. 7.11).
b. Fibromuscular dysplasia, which is an overgrowth of collagen (dysplasia of the media of the arteries). This is more common in young females. This condition shows up on angiography like a “string of beads.” Many patients have nonspecific or no obvious ultrasound abnormalities.
c. Carotid body tumor. This is a highly vascular tumor that arises between the external and internal carotid arteries. It may occur bilaterally (Fig. 7.12).
d. Extravascular masses, such as lymph nodes, abscesses, or hematomas, can compress or displace the carotid arteries.
e. Posttraumatic pseudoaneurysms can occur after trauma or surgery, such as endarterectomy. This appears as a swirling pocket of blood attached
to the artery by a “neck.” On color Doppler, there is a swirling pattern of blood often with a “yin-yang” appearance (Fig. 7.13).
to the artery by a “neck.” On color Doppler, there is a swirling pattern of blood often with a “yin-yang” appearance (Fig. 7.13).
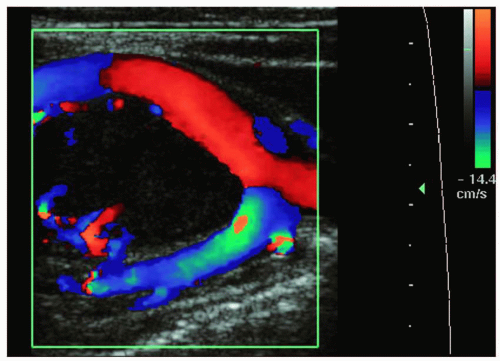 FIGURE 7.12. Sagittal color image of a carotid body tumor. (Image courtesy of Philips Medical Systems.) |
f. Aneurysm appears as an abnormal bulge in the vessel.
g. Collagen vascular connective tissue disorders.
h. Arteritis resulting from autoimmune diseases such as Takayasu arteritis, temporal arteritis, or radiation changes. This causes diffuse concentric thickening of the carotid walls, frequently involving the CCA.
6. The two most common causes for brain ischemia are embolization and hypoperfusion. These are most often caused by stenosis, thrombosis, and embolism.
7. Plaque in the carotid arteries may be removed surgically, a procedure that is called an endarterectomy. Two clinical trials recently established the therapeutic benefit of endarterectomy in asymptomatic patients
with greater than 60% diameter reduction of the ICA (the Asymptomatic Carotid Atherosclerosis Study, or ACAS), and for symptomatic patients with greater than 70% stenosis of the ICA (the North American Symptomatic Carotid Endarterectomy Trial, or NASCET).
with greater than 60% diameter reduction of the ICA (the Asymptomatic Carotid Atherosclerosis Study, or ACAS), and for symptomatic patients with greater than 70% stenosis of the ICA (the North American Symptomatic Carotid Endarterectomy Trial, or NASCET).
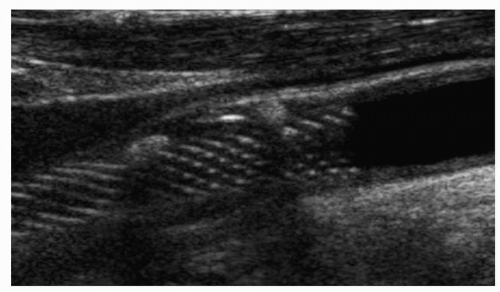 FIGURE 7.14. Sagittal gray-scale image of a carotid artery stent. (Image courtesy of Philips Medical Systems.) |
8. Although unusual, a potential complication following carotid endarterectomy is pseudoaneurysm. This may present as a painful and pulsatile mass following surgery.
9. Although endarterectomy is considered the standard for treatment of atherosclerotic carotid arterial occlusive disease, carotid angioplasty with stent placement has emerged recently as a potential alternative (Fig. 7.14). Some medical centers may also use patch angioplasty following endarterectomy. This may be done with a synthetic or a vein (usually saphenous) patch (Fig. 7.15). Vein patching may help reduce early or late restenosis after a carotid endarterectomy. A potential complication of saphenous vein patching is that it can cause the carotid artery to become dilated, risking rupture and thrombosis.
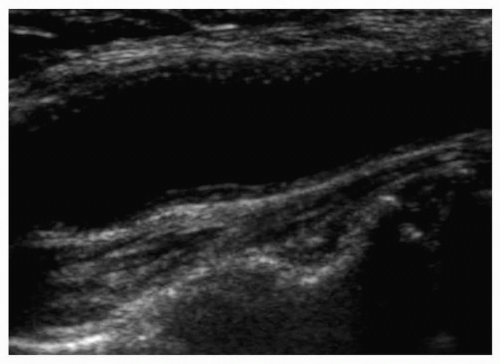 FIGURE 7.15. Gray-scale image of a vein patch in the carotid artery. (Image courtesy of Philips Medical Systems.) |
10. A bypass graft may be used for occlusion of the proximal common carotid, subclavian, or brachiocephalic arteries.
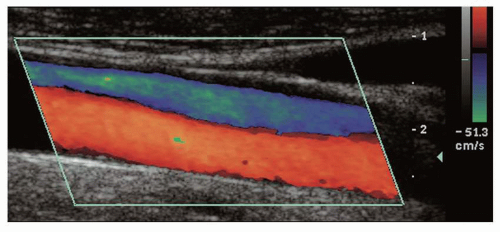
D. Subclavian steal syndrome
(also known as vertebral steal). When significant disease is present in the brachiocephalic or proximal subclavian arteries, blood must now course up the contralateral vertebral artery, cross over at the basilar artery, and course down the vertebral artery of the affected side to the subclavian artery to perfuse the arm. Even at rest, a significant difference in blood pressure of the affected arm is found when compared with the unaffected side. The difference in blood pressure is 15 to 20 mm Hg, with the side producing the lower pressure being the affected side. There is increased resistance in vertebral arterial flow, and reverse flow is seen in the ipsilateral vertebral artery. A partial vertebral steal is one that almost meets the circulatory requirements of the arm, and has bidirectional flow that can be converted to a complete steal by exercising the arm or by placing a blood pressure cuff on the arm for a few minutes, then releasing. Surgical treatment may include endarterectomy or a bypass graft.
III. HISTORY: QUESTIONS TO ASK THE PATIENT
A.
Have you ever had a cerebrovascular accident (CVA)? [A cerebrovascular accident is otherwise known as a stroke. It produces permanent neurologic deficits. Stroke is the third leading cause of death in the United States. Strokes are either ischemic (due to a decreased blood supply) or hemorrhagic (due to a blood vessel that bursts.) Approximately 80% of strokes are due to ischemia from thromboemboli. In the United States, a large portion of thromboemboli are due to atherosclerotic disease of the carotids. The plaque breaks off and interrupts blood flow to the brain. It is estimated that one third of patients who have had a transient ischemic attack (TIA) will have a CVA within 5 years.]
B.
Have you ever had a TIA? [A transient ischemic attack is a neurologic event that reverses within 24 hours or less. It usually reverses within 30 minutes. These are usually caused by embolization from the heart or the carotid arteries. Symptoms may include dysfunction of an arm or leg, speech problems, and visual disturbances.]
C.
Have you ever had a reversible ischemic neurologic deficit (RIND)? [A reversible ischemic neurologic deficit is a TIA that lasts longer than 24 hours but less than 72 hours.]
D.
Have you ever had any of the following symptoms:
1. Hemispheric symptoms:
a. Amaurosis fugax. This is transient unilateral blindness that is caused by emboli from a more central source. If this is from carotid plaque it will occur in the ipsilateral eye.
b. Hemiparesis/hemiplegia. This is paralysis or weakness on one side of the body (arm or leg or both.) If this is from carotid plaque it will occur on the contralateral side. It may be accompanied by:
c. Paresthesia or anesthesia. This is numbness or tingling on one side of the body.
d. Aphasia or dysphasia. This is a language deficit. The patient has a problem with understanding or finding words. The causal lesion would be in the carotid artery supplying the dominant hemisphere (which is the left for most patients).
e. Behavioral abnormalities.
f. Hemianopsia. This is blindness in one half of the visual field.
2. Vertebrobasilar symptoms:
a. Vertigo. This is the difficulty in maintaining equilibrium, the feeling that you are moving around in space or having objects move around you in space.
b. Ataxia. This is the failure of muscle coordination, gait disturbance, or imbalance.
c. Dysphagia. This is pain or difficulty with swallowing.
d. Dysphonia. This is impairment of the voice.
e. Dysarthria. This is abnormal articulation or pronunciation.
f. Paresthesia or anesthesia. This involves numbness and tingling on both sides of the body.
g. Diplopia. This is double vision.
h. Nystagmus. This is rapid involuntary movement of the eyeball.
i. Horner syndrome. This is ptosis (drooping) of the upper eyelid, with sinking in of the orbit and constriction of the pupil.
j. Drowsiness, stupor, or altered consciousness.
k. Motor and sensory deficits of the face. This includes a facial droop and perioral numbness. This can be unilateral, bilateral, or alternating.
l. Motor and sensory deficits of the body. This can be unilateral, bilateral, or alternating.
3. Nonlocalizing symptoms:
a. Dizziness or lightheadedness
b. Syncope—This is a transient loss of consciousness.
c. Headache, nausea, vomiting
d. Confusion
4. The MCA is the most commonly affected artery for a stroke. The symptoms that correlate with specific arteries include:
a. Internal carotid artery. Frequently seen symptoms are contralateral weakness, paralysis, numbness, and/or sensory changes; ipsilateral amaurosis fugax, and/or a bruit; possibly aphasia or altered level of consciousness.
b. Middle cerebral artery. Frequently seen symptoms are aphasia or dysphasia, severe contralateral hemiparesis or hemiplegia, dysarthria, behavioral changes, confused state, possibly agitated delirium.
c. Anterior cerebral artery. Frequently seen symptoms are contralateral hemiparesis, loss of consciousness, impaired motor and sensory functions, loss of coordination.
d. Vertebrobasilar. Frequently seen symptoms are vertigo, ataxia, diplopia, amnesia, dysphagia, loss of coordination, perioral numbness.
e. Posterior cerebral artery. Frequently seen symptoms are dyslexia and coma.
E.
Do you have hypertension?
F.
Do you have diabetes?
G.
Do you have high cholesterol?
H.
Do you smoke? How many packs per day? For how long have you smoked?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree