(1)
Department of Neuroscience, University of Turin Ospedale Molinette, Turin, Italy
Abstract
A venous thrombosis involving the SSS linked to an infectious disease was described about 200 years ago in 1825 by Ribes. Since then, a progressive improvement in diagnostic methods, in particular angiography (Huhn 1957, 1962; Krayenbuhl 1961, 1967; Vines and Davis 1971) and later CT, MRI, and MRI angiography, has made it possible to identify this pathology. The true incidence of cerebral venous thrombosis (CVT), however, remains unknown, even if there is no doubt that it is more frequent than had previously been thought (Krayenbuehl 1967; Ameri and Bousser 1992; Bousser et al. 1985; Einhäupl and Masuhr 1994; Bousser and Russell 1997; Linn and Brückmann 2010).
A venous thrombosis involving the SSS linked to an infectious disease was described about 200 years ago in 1825 by Ribes. Since then, a progressive improvement in diagnostic methods, in particular angiography (Huhn 1957, 1962; Krayenbühl 1961, 1967; Vines and Davis 1971) and later CT, MRI, and MRI angiography, has made it possible to identify this pathology. The true incidence of cerebral venous thrombosis (CVT), however, remains unknown, even if there is no doubt that it is more frequent than had previously been thought (Krayenbühl 1967; Ameri and Bousser 1992; Bousser et al. 1985; Einhäupl and Masuhr 1994; Bousser and Russell 1997; Linn and Brückmann 2010).
20.1 Etiopathogenesis
A frequent cause is infection, either intracranial extension of infectious diseases involving the skin–bone cavities of the craniofacial area or in cases of general bacterial septicemia or viral infection, especially due to HIV and cytomegalovirus. In young women, CVT occurs during pregnancy, in puerperium, and in patients using oral contraceptives. Other causes are pathologies of the red blood cells, such as thrombophilia, polycythemia, sickle cell disease, leukemia, and lymphoma, and in many coagulation disorders, such as protein C and S deficiency and disseminated intravascular coagulation. CVT also is frequent in patients with Behçet’s disease, systemic lupus erythematosus, and in patients with severe dehydration and cardiac failure. Other causes are cranial trauma and neurosurgical intervention. Finally, intracranial tumors, especially meningiomas, can involve the adjacent sinus and cause thrombosis.
It should, however, be taken into consideration that in many cases—up to 35 %—the cause remains unknown (Milandre et al. 1988; Ameri and Bousser 1992; Cantu and Barinagarrementeria 1993; Einhäupl and Masuhr 1994). As far as it concerns the sinus thrombosis in patients with dural arteriovenous fistulas, see Chap. 13.
20.2 Location
The superior sagittal sinus (SSS) is the venous channel most commonly involved, followed by the transverse sinus. Both are frequently involved together (Ameri and Bousser 1992; Cantu and Barinagarrementeria 1993; Tsai et al. 1995; Linn and Brückmann 2010). The thrombosis can be limited to the sinus, and the clinical presentation may frequently be characterized by clinical symptoms owing to intracranial hypertension, such as headache and visual disturbances. Cortical vein tributaries of the thrombosed sinus can be secondarily involved as a result of retrograde propagation of the thrombus, which commonly leads to ischemia.
Isolated cortical vein thrombosis may also occur. This had been thought to be very rare (Ameri and Bousser 1992; Einhäupl and Masuhr 1994). Recently, through improvement in MRI techniques and progressive awareness of this pathology, cases have been increasingly reported (Sagduyu et al. 2006; Boukobza et al. 2009; Albayram et al. 2009; Linn and Brückmann 2010). The cortical veins can be an important collateral circulation, which, however, may be involved at any point of their course, leading to infarct (Bergui et al. 1999; Bradac and Bergui 2001).
Thrombosis of the deep venous system, involving the straight sinus and the vein of Galen, with retrograde extension to the internal cerebral and basal veins, is another usually severe condition that is, fortunately, less common. In these situations, transcerebral anastomoses via connections between the superficial and deep medullary veins can act as an important collateral circulation and connect the superficial and deep venous systems (Bergui et al. 1999; Bradac and Bergui 2001).
Cavernous sinus thrombosis is another frequent localization, and it leads to a typical cavernous sinus syndrome. The lesion can extend to the superior–inferior petrosal sinus. Involvement of the intracavernous internal carotid artery, with arteritis leading to stenosis/occlusion, can occur (Segall et al. 1982). Cavernous sinus thrombosis is commonly due to infectious processes that involve the skin of the facial region, nose, paranasal sinuses, orbita, teeth, and middle ear.
20.3 Diagnosis
CT and MRI allow the detection of changes to the brain parenchyma in the form of hemorrhagic and/or nonhemorrhagic infarcts, uni- or bilateral, and single or multiple, with various locations depending on the site and extension of the CVT. Hemorrhagic ischemia can be easily diagnosed on CT studies, presenting as hyperdense area. White matter hypodensity on CT and hyperintensity on T2 images on MRI, which indicate edema of a preceding venous infarct, is also a sign suggesting venous thrombosis. On CT, an abnormal hyperdensity can be recognized at the level of the torcular herophili, SSS, and lateral sinus. This is, however, difficult to differentiate in the majority of cases from the normally slight hyperdensity of this structure. Though it is not always present, a more reliable indicator is the so-called empty sign, which is visible after contrast injection and is due to opacification of the sinus wall contrasting with the low density of the thrombus in the lumen (Buonanno et al. 1978; Kingsley et al. 1978). Also MRI can be very useful (Bousser and Ferro 2007). In the acute phase, it shows the hypointensity and isointensity of the thrombus in the involved sinus and occasionally in the cortical or deep veins, respectively, on T2- and T1-weighted images. After 3–5 days, the clot becomes progressively hyperintense on both T1–T2 sequences. In this context, the high diagnostic value of the T2*-weighted gradient echo in identifying also isolated cortical vein thrombosis has been emphasized by some authors (Fellner et al. 2005; Urban and Müller-Forrell 2005; Boukobza et al. 2009; Linn and Brückmann 2010). Finally, in cases of suspected CVT, MRI angiography should be performed.
In doubtful cases, or whenever a more specific diagnosis is required, angiography remains a useful diagnostic method. A rapid and precise diagnosis is important since anticoagulant therapy can improve the prognosis of these patients (Villringer et al. 1994; Einhäupl et al. 2006). Examples of venous thrombosis are shown in Figs. 20.1, 20.2, 20.3, 20.4, and 20.5.
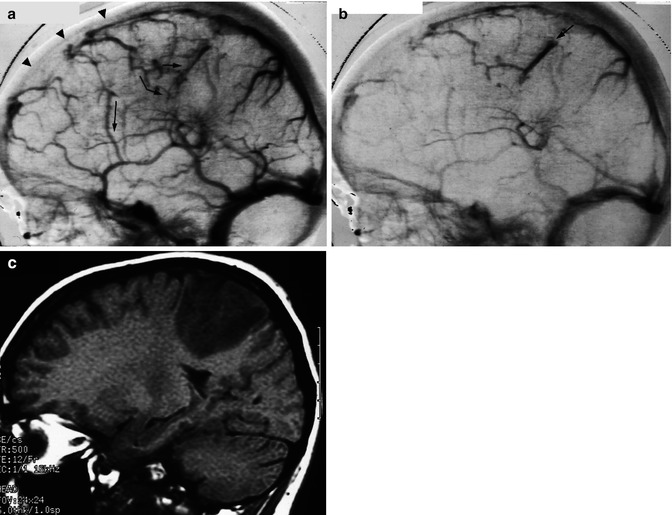
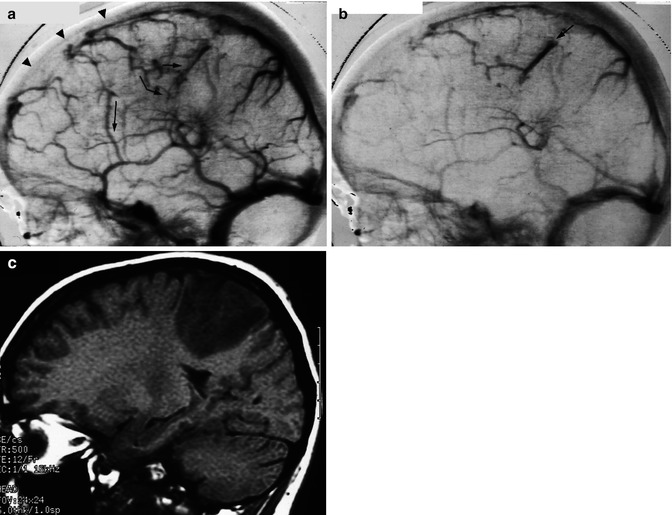
Fig. 20.1




Thrombosis of the anterior and middle segments of the superior sagittal sinus (SSS; arrowheads). Carotid angiogram, lateral view, venous phase (a). Rerouting of the venous drainage through cortical veins toward the parietal and temporal area. Some of these veins have a typical “corkscrew” appearance (arrows). Later phase (b). Distal occlusion of the cortical veins (arrow) probably explaining the parietal ischemia, visible on MRI (c)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


