Chapter 15
Catheter and Port Removal: Techniques and Follow-Up Care
The use of central venous catheters has increased dramatically over the past 20 years. These devices now are considered essential in providing dependable venous access for both acute and chronically ill patients. Whereas much emphasis is placed on the insertion and management of central catheters, little attention has been given to their removal, and this task is often assigned to junior physicians or nurses who are inexperienced in removal procedures. This chapter discusses the techniques for removal of the various types of venous catheters and ports; briefly mentions the complications of catheter removal; and provides therapeutic measures to deal with infected catheters, tunnels, and pockets.
Once the decision is made to remove a catheter or port either because an infection clearly has occurred, because infection is suspected to be present, or because the vascular access is no longer needed, the patient is counseled about what to expect during the removal procedure and thereafter. Informed consent is not routinely obtained for a simple catheter removal unless another catheter is going to be inserted or an associated procedure will be performed. Some operators may wish to obtain consent, however, particularly if the catheter being removed was placed initially by someone else. Necessary equipment for catheter removal includes a cut-down tray and a small table with basic instruments. A bed that allows placement of the patient in a head-down position (Trendelenburg) is ideal although not required. This special bed is not routinely available in most radiology departments. Removals are done in any suitable room, not necessarily in the angiographic laboratory; so the laboratory can be used for other purposes.
REMOVAL OF TUNNELED CATHETERS
Tunneled catheters should be removed when they are infected or no longer needed. In general, the longer a catheter has been in place, the more difficult the removal may be; however, this is not necessarily true. In fact, some infected catheters or ports will slide out easily regardless of how long they have been in place. Some patients develop thick scar tissue and cheloid very rapidly. We have seen patients in whom removal of a catheter placed a few weeks earlier was rather difficult.
The skin over the catheter exit site, the tunnel, and the area overlying the entrance site into the vein is prepared using Povidone–iodine (7.5–10%) or alcohol. Sterile drapes and towels are placed to establish a sterile field. Adequate local anesthesia is obtained with lidocaine, with or without epinephrine, and infiltrated in the soft tissues, making sure that the entire subcutaneous tunnel and the skin over the site of entry into the vein are well anesthetized. Special care must be taken not to puncture the catheter during the administration of local anesthetic because bleeding may follow if the catheter is damaged. Initially, the catheter is released from the skin at the exit site by cutting the anchoring sutures, if present. If the catheter was placed recently, that is, less than 2 weeks ago, removal requires little dissection, but this is not always true.
HELPFUL HINTS
If the catheter cuff has not yet scarred in place, administration of local anesthesia, which can be painful, especially in inflamed tissues, may not be necessary. A gentle tug on the catheter may be given before anesthetizing to determine whether the catheter will slide out of the tunnel, thereby eliminating the need for local anesthesia. We routinely mix lidocaine with sodium bicarbonate (1 mL of NaHCO3 for 10 mL of lidocaine) to decrease significantly the pain and burning associated with lidocaine.
The patient should be instructed to suspend respiration temporarily to prevent the serious risk of air embolism, which may occur if the patient takes a deep inspiration as the catheter exits the vein. The catheter is grasped with one hand, at or near the hub, and pulled slowly and steadily to ensure that the force of traction follows the path of the tunnel. Excessive force or tension must be avoided because the catheter may rupture, with resultant bleeding in the tunnel or fragment embolization. The operator must immediately hold pressure at the venous insertion site with the other hand as soon as the catheter exits the vein at the puncture site. In certain cases, such as infection, care should be taken to prevent contamination of the catheter if the tip is needed for culture. Hemostasis usually is achieved by holding gentle pressure on the vein for about 10 minutes. Elevation of the head of the bed more than 30 degrees may help with hemostasis.
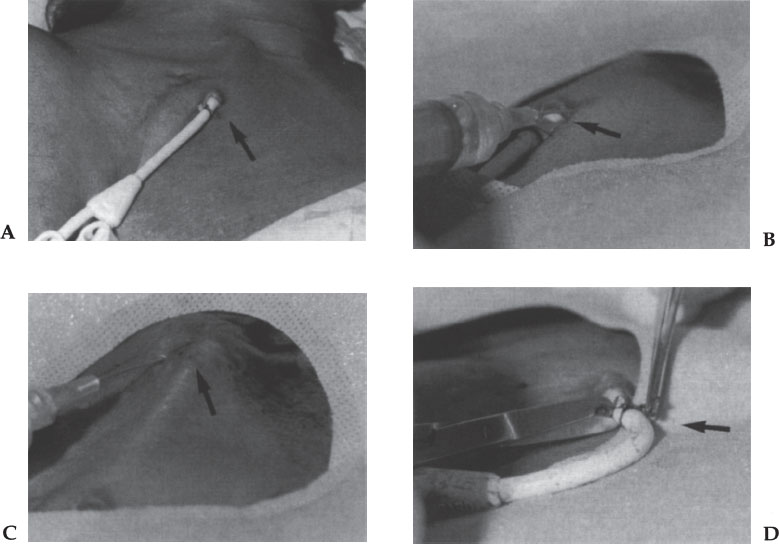
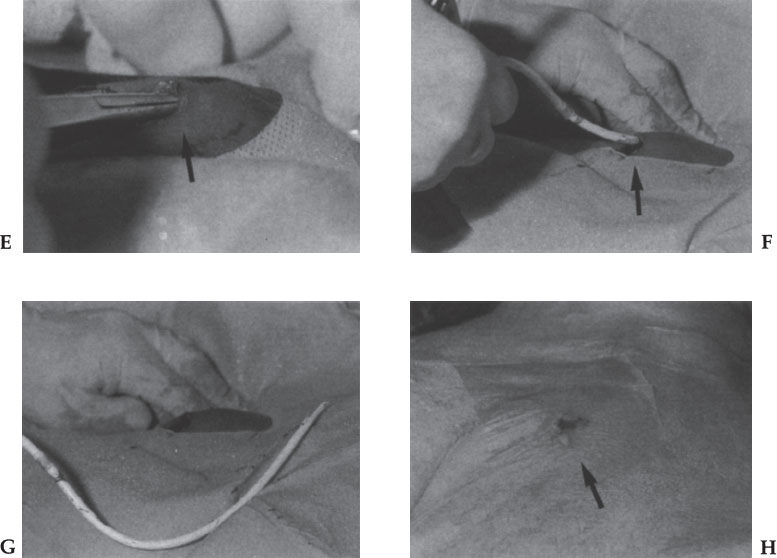
Figure 15–1 Removal of tunneled catheter. (A) Catheter exit site prepped and draped. (B, C) Exit site and tunnel infiltrated with lidocaine with 1% epinephrine. (D) The stitch holding the catheter is removed. (E) Blunt dissection of the tunnel with a Kelly clamp. (F) The catheter is withdrawn from the tunnel. (G) Hemostasis is obtained. (H) Dressing is applied. Patient is sent home.
When the catheter has been in place a long time, scarring and granulation at the cuff site(s) and elsewhere require blunt and sharp dissection along the entire tunnel to free the scar tissue. This is done using a long hemostat or a straight Kelly clamp. The dissection must be done circumferentially around the entire catheter, that is, front, back, medial, and lateral. The aim is to loosen the scar tissue and allow the catheter to become free. Progressively increasing tension may be needed, but special care must be taken to avoid rupturing the catheter. The point of greatest resistance, scarring, and adherence is usually around the Dacron cuff (or cuffs if two or more are present).
HELPFUL HINTS
Applying steady tension to the catheter may result in dimpling of the skin overlying the cuff because this is the point of “attachment.” This “dimpling” will give the operator the expected location of the cuff(s). As the closed hemostat is inserted into the subcutaneous tunnel, alongside the catheter, resistance will be encountered at the site of granulation and scar tissue. Continuing to apply tension to the catheter, forcefully advancing the closed hemostat into the scar tissue, and opening the hemostat will bluntly dissect the scar tissue and free the catheter from the tunnel.
HELPFUL HINTS
During pulling the catheter, enough tension must be applied to release the catheter free of the remaining granulation and scar tissue; however, care must be taken not to apply so much tension that the catheter breaks. Some large catheters, such as dialysis (12–14 F) catheters, are quite sturdy, and a great deal of tension can be applied during removal, but these catheters can rupture. The smaller 7 to 10 F tunneled catheters, especially Silastic catheters, will break with the application of even a little tension. When the catheters break, they usually tear on the hub side of the Dacron cuff. This is a serious situation that requires prompt action because brisk bleeding into the subcutaneous tract may occur and air embolization into the venous system is likely. The catheter must be compressed immediately. If the procedure was being done unassisted, one must get help immediately because it is impossible to hold pressure over the catheter while dissecting the tract. Once the bleeding has been controlled with compression, another incision should be made at the venous entry site or over the subcutaneous tunnel near this site. Using a hemostat, blunt dissection is done until the underlying catheter is seen and retrieved. The catheter must be clamped to stop bleeding from its torn end. The clamped catheter should then slide easily out of the vein as pressure is applied at the venous puncture site. When hemostasis is obtained, the remaining segment of catheter with the Dacron cuff may be dissected free through the new skin incision.
The patient must stop breathing momentarily while the catheter is being removed to prevent air embolism. The operator must promptly compress the venous puncture site, which is usually apparent on examination of the scar of the healed puncture site. Once hemostasis is achieved, antibiotic ointment may be applied to the exit wound and an airtight occlusive dressing placed over the site and left there for 2 to 3 days. If the exit site is large, a single interrupted stitch must be placed; otherwise, Steri-strips are used to close the skin. Tunneled catheters placed in the femoral vein are removed in a similar fashion (Fig. 15–1).
On occasion, during tension and pulling of the catheter, the Dacron cuff may be separated off the catheter and remain in the subcutaneous tissue. The cuff is left there because it is of no clinical significance and nothing needs to be done. If for cosmetic or other reasons (infected tunnel) cuff removal is desired, a direct cut-down over the region of the retained cuff may be needed for the cuff to be removed.
REMOVAL OF SUBCUTANEOUS PORTS
Ports must be removed by an experienced operator. A surgical cut-down tray is required. The skin over the pocket, the subcutaneous tunnel, and the venous puncture site are prepped with povidone-iodine (7.5–10%) and alcohol. Sterile towels and drapes are placed to create a sterile surgical field. Adequate local anesthesia is obtained using generous amounts of 1% buffered (with sodium bicarbonate) lidocaine. Care must be taken not to puncture the catheter within the tunnel while injecting the local anesthetic. Ideally, if a special table is available, the patient can be placed in a Trendelenburg position with the head turned away from the working site. A no. 10 or 15 scalpel is used to make an adequate skin incision over the previous scar, which will result in only one scar with better cosmetic results. Forceps are used to elevate and separate the tissues directly over the port. Using blunt and sharp dissection with scissors and scalpels, the scar tissue, which usually surrounds and encases the port, is released. Additional dissection may be needed to release scar tissue often found at the port stem /catheter lock as well as at the proximal portion of the tunnel. Dissection along the tunnel is rarely needed to free the catheter because the Silastic catheter is biocompatible and does not promote scar tissue. The catheter is withdrawn from the vein and tunnel easily. Once the port and catheter are free, the patient is instructed to suspend respirations to prevent air embolism. The catheter is grasped distal to the connection with the port and withdrawn in a slow, steady manner. To achieve hemostasis, the venous puncture site must be compressed for 10 minutes as soon as the catheter tip exits the vein. Dry gauze can be placed inside the pocket and pressure applied for hemostasis. The gauze is removed and the pocket examined to ensure that it is “dry” and no hematoma is forming. If bleeding sites are noted, they should be ligated or controlled. Absorbable sutures are placed to approximate the deeper subcutaneous tissues and, depending on the operator’s preferences, buried subcutaneous running absorbable sutures or simple interrupted nonabsorbable sutures are used to close the skin. Antibiotic ointment can be applied to the wound, and an airtight dressing is left in place for 2 to 3 days.
REMOVAL OF NONTUNNELED CATHETERS
Nontunneled access catheters are used for a few weeks to 3 months. Because these catheters require minimal tissue disruption, and no tunnel is formed, removal of the catheter is easy and straightforward. Nontunneled catheters are removed in a manner similar to tunneled catheters, although tunnel dissection is not needed. Once the external fixation tape and suture are removed, the patient is instructed to stop breathing, and the catheter is withdrawn in a firm and steady manner along the axis of the central vein. Hemostasis is achieved by holding pressure on the vein for 10 minutes or longer.
Peripherally inserted central catheters (PICCs) are removed easily at the bedside or at home by nursing personnel. Once the anchoring suture and tape are removed, the catheter is withdrawn from the vein and compression is applied for 3 to 5 minutes. On rare occasions, PICCs are difficult to remove. Tourniquet applicatipn and warm soaks have been tried with success. Venospasm (as confirmed by ultrasound) may be the cause of difficulty in some cases. Gentle traction usually can overcome a mild vasospasm; however, aggressive pulling may result in catheter breakage and embolism with serious consequences and embarrassment for the operator. This will require retrieval using conventional techniques. If any resistance is felt during removal by nursing personnel, the procedure should be aborted and an experienced operator or radiologist consulted. If catheter fragments and embolism occur during removal, percutaneous retrieval is done by an experienced operator in the conventional manner.
COMPLICATIONS
The incidence of complications of placement of central venous catheters and ports is low and ranges from 0.4 to 11%, including major and minor complications. There are, however, no accurate statistics for complications associated with catheter or port removal. This topic has received little attention and is not mentioned in most reviews. It is clear from the available information that the risks of central venous catheter removal are low but still may create a problem for some operators. Furthermore, the life-threatening nature of some complications (such as air embolism) may contribute to high morbidity.
Air Embolism
Besides bleeding, one of the most common and feared complications of catheter and port removal is air embolism. The signs and symptoms may be nonspecific, and the diagnosis can be made based on clinical assumption, often after an unsuspected transient cardiopulmonary collapse or neurologic dysfunction has occurred. Few documented cases are reported in the literature of air embolism during placement of central venous catheters,1–4 and even fewer documented cases are reported of air embolism during catheter removal.5–8 Breathing during removal by uncooperative patients is the cause. Also, if a fibrin sheath is present along the catheter tract in the tunnel, the sheath can be a pathway for air to enter the venous system if prompt hemostasis is not performed.
After removal of a central venous catheter, regardless of the site, a short tract between the skin and the vein may stay patent momentarily. The tract, if large enough, can allow air to enter the venous system during inspiration. Enough air to cause embolism and cardiorespiratory collapse can enter the venous system in one inspiration. For this reason, it is critical that patients suspend respiration during the withdrawal phase of catheter removal until firm pressure is maintained on the vein to occlude the puncture site. It has been reported that a tract diameter of 4.5 mm needed to insert a 14 F catheter can allow conduction of 200 cc of air in 1 second, according to Poiseuille’s law.7 The documented lethal amount of injected air in humans is 70 to 105 cc per second.1 If the embolized air is trapped in the right ventricle, it may produce right ventricular obstruction, resulting in acute right heart failure, shock, and death.
Furthermore, it has been reported that in humans the foramen ovale may remain patent in 10 to 24% of the population.9 Therefore, if a patient has a patent foramen ovale, serious and catastrophic arterial air embolism can occur. Air in the left ventricle can migrate into the carotid arteries, causing cerebral air embolism.
In addition, air can enter the venous system directly through the catheter, especially if it becomes disconnected from the intravenous line or if the hub of the catheter is open or incompletely locked. The sound of sucking air through the catheter or tract is highly suggestive of air embolism. Fluoroscopy and other radiologic examinations, such as chest radiographs, computed tomography, or echocardiogram, may show air embolized in the heart or brain. Prompt recognition of air emboli is critical to allow therapeutic intervention. Patients should be given 100% oxygen immediately. Embolized air can produce right ventricular outflow obstruction, acute right-sided heart failure, and shock. If the embolized air remains in the right side of the heart, immediately place the patient in the left lateral decubitus position with the patient’s left side down (Durant) and the head down (Trendelenburg) to allow blood to flow out of the right ventricle into the pulmonary outflow tract and preventing obstruction.10 Furthermore, the air can be trapped in the right atrium, and a catheter can be inserted into the right side of the heart and the air aggressively aspirated (as much as possible) to prevent the serious sequelae.11
Pulmonary Embolism
Pericatheter thrombus is a common complication of long-term indwelling central venous catheters. It is estimated that 42 to 100% of venous catheters become covered by a fibrin sheath.12 During withdrawal of the catheters, thrombi and fibrin may be stripped from the catheter and embolize into the lungs. These pulmonary emboli are usually small and of no clinical significance in most patients, unless they have a borderline pulmonary reserve. Furthermore, if the patient has a patent foramen ovale, the emboli can gain access to the left ventricle and embolize into the carotid circulation, leading to a stroke. Moreover, it was recently reported that the sleeve surrounding the catheters is not a true fibrin sleeve but, rather, an organized cellular–collagen tissue covered by endothelium.12
It is important to know that the cellular–collagen sleeve can be present as early as 24 hours, be complete in 1 week, and last up to 10 months after catheter removal. This process may play an important role in the withdrawal occlusion of veins. Some investigators have suggested the prophylactic use of aspirin, and even oral warfarin, to decrease the incidence of catheter-related venous thrombus formation, as is almost routinely done for arterial thrombus prevention.13 Other researchers have found no correlation between thrombus formation, duration of catheterization, type of catheter used, or regimen of anticoagulation with heparin, either therapeutic or low-dose.14
Catheter Rupture
Catheter breakage during removal is an infrequent complication. Repeated handling of the external portion of the catheter by health care personnel and patients may result in fatigue and fragmentation of the catheter material. During withdrawal, the catheter may break, leaving a segment of catheter inside the vein or in the tunnel. If this occurs, the broken segment may embolize into right heart or pulmonary arteries. The fragment can be removed percutaneously from a femoral approach with conventional retrieval methods. If the segment stays in the tunnel or at the entry site, it can be removed by direct cut-down on the vein. In our experience, the retained fragment remains in position in the tunnel and usually does not embolize.
Arterial Trauma
It is important to remember the relationship of the internal jugular veins to the carotid arteries in the neck. The puncture site in the neck is always close to the carotid artery. Too much pressure or forceful rubbing in this region may cause arteriosclerotic plaque dislodgment and embolization, causing stroke. Furthermore, stimulation of the carotid sinus during hemostasis compression may result in unwanted vasovagal bradycardia, hypotension, and even loss of consciousness. Fortunately, this event is very rare.
Infection
Catheter-related infection is a serious and significant complication of central venous catheter placement. Whether the infection is confined to the skin exit site, involves the pocket or tunnel, or has entered the bloodstream (bacteremia/sepsis), it is imperative that the interventional radiologist be knowledgeable and prepared to provide treatment and make recommendations for appropriate care.
The incidence of infectious complications differs significantly with the different types of catheters. There is a higher infection rate in nontunneled catheters. The incidence of infection of tunneled catheters is as high as 10 to 30%.15,16 The infection rate for Hickman catheters is 1.9 per 1000 catheter days when a radiologist places the catheter and 4.0 per 1000 catheter days when a surgeon places the catheters.17
Subcutaneous ports have lower infection rates, ranging from 0.03 to 0.1 per 1000 catheter days.18 On the other hand, PICCs have infection rates of 3.1 per 1000 catheter days.15 The diagnosis of catheter-related infection can be difficult. Subtle clinical signs, such as unexplained leukocytosis, low-grade fever, or an isolated positive blood culture, might be the only feature of a raging infection. Unfortunately, the frequently used parameters for diagnosing a catheter infection are nonspecific. Pain, local erythema, and swelling may be more significant indicators of catheter infection than other clinical and laboratory parameters.19
The treatment for a catheter-related infection depends on the extension of the process. Exit-site infections are the easiest to diagnose and usually present with tenderness and erythema about 1 cm around the exit site. Occasionally, a purulent exudate may be present. These infections can be treated successfully with local measures and antibiotics.
Tissue disruption of the port pocket or tunnel and tenderness and cellulitis over the port or along the tunnel indicate a serious infection or abscess. The port or tunneled catheter must be removed. Pus or cloudy fluid should be cultured and intravenous antibiotics started. The pocket must be opened and thoroughly irrigated with saline and packed with iodoform gauze twice daily until the drainage has stopped. The pocket eventually will heal by secondary intention. If the tunnel is infected, the skin over the tunnel can be incised and the tunnel drained. Alternatively, the tunnel can be enlarged, irrigated, and packed from both ends with gauze twice daily until drainage stops and eventually heals by secondary intention as the gauze is progressively withdrawn.
Occasionally, an infection is suspected, but there is no purulent drainage when the port or catheter is removed. The wound can be packed for a few days and then closed primarily, a process called delayed primary closure or tertiary healing. Because most patients who require ports and tunneled catheters are immunocompromised, the absence of pus does not exclude an infected port pocket or catheter tunnel.
Diagnosing catheter-related infections early and providing aggressive treatment reduce the morbidity and may allow salvage of the access device. Most catheter infections are caused by skin flora; therefore, antibiotic coverage of gram-positive microorganisms with cefazolin or vancomycin is usually sufficient. A 10- to 14-day course of oral or intravenous treatment is given, with modifications depending on the patient’s clinical response, or bacterial culture and sensitivity results.
SUMMARY
Catheter and port removal is done when a catheter-related infection is present or suspected or when the device is no longer needed. Care must be taken during catheter removal because complications, some of them serious (e.g., air embolism, catheter rupture, embolization) could occur.
The vascular and interventional radiologist must be prepared to remove catheters and ports and must educate ancillary personnel and home caregivers about the methods and problems associated with catheter or port removal.
REFERENCES
1. Coppa GF, Gouge TH, Hofstetter SR. Air embolism: a lethal but preventable complication of subclavian vein catherization. Int Surg. 1972;57:42–45.
2. Feliciano DV, Mattox KL, Graham JM, et al. Major complications of percutaneous subclavian vein catheters. Am J Surg. 1979;138:869–874.
3. Kashuk JL, Penn I. Air embolism after central venous catherization. Surg Gynecol Obstet. 1984;159:249–252.
4. Grace DM. Air embolism with neurologic complications: a potential hazard of central venous catheters. Can J Surg. 1977;20:51–53.
5. Sing RF, Steffe TJ, Branas CC. Fatal venous air embolism after removal of a central venous catheter. J Am Osteopath Assoc. 1995;95:204–205.
6. Mennim P, Coyle CF, Taylor JD. Venous air embolism associated with removal of central venous catheter. BMJ. 1992;305:171–172.
7. Phifer TJ, Bridges M, Conrad SA. The residual central venous catheter tract: an occult source of lethal air embolism: case report. J Trauma. 1991;31:1558–1560.
8. McCarthy PM, Wang N, Birchfield F, et al. Air embolism in single-lung transplant patients after central venous catheter removal. Chest. 1995;107:1178–1179.
9. Papadopoulous G, Kuhly P, Brock M, et al. Venous and paradoxical embolism in the sitting position: a prospective study with transesophageal endocardiology. Acta Neurol. 1994;126:140–143.
10. Durant TM, Oppenheimier MJ, Lynch PR, et al. Body position in relation to venous air embolism: a roentgenologic study. Am J Med Sci. 1954;227:509–520.
11. Minchenfelder JD, Martin JT, Altenberg BM, et al. Air embolism during neurosurgery: an evaluation of right atrial catheters for diagnosis and treatment. JAMA. 1969;208:1353–1358.
12. Xiang DZ, Verbeken EK, Van Lommel AT, et al. Composition and formation of the sleeve enveloping of a central venous catheter. J Vasc Surg. 1998;28:260–271.
13. Bern MM, Lokich JJ, Wallach SR, et al. Very low doses of warfarin can prevent thrombosis in central venous catheters: a randomized prospective trial. Ann Intern Med. 1990;112:423–428.
14. Randolph AG, Cook DJ, Gonzales CA, et al. Benefit of heparin in peripheral venous and arterial catheters: systematic review and meta-analysis of randomized controlled trials. BMJ. 1998;316:969–975.
15. Clarke DE, Raffln TA. Infectious complications of indwelling long-term central venous catheters. Chest. 1990;97:966–972.
16. Johnson A, Oppenheim BA. Vascular catheter-related sepsis: diagnosis and prevention. J Hosp Infect. 1992;20:67–78.
17. McBride KD, Fisher R, Warnock N, et al. Comparative analysis of radiological and surgical placement of central venous catheters. Cardiovasc Interv Radiol. 1997;20:17–22.
18. Hills JR, Cardella JF, Cardella K, et al. Experience with 100 consecutive central venous access arm ports placed by interventional radiologists. J Vasc Interv Radiol. 1997;8:983–989.
19. Barnes JR, Lucas N, Broadwater JR, et al. When should the “infected” subcutaneous infusion be removed? Am Surg. 1996;62:203–206.
< div class='tao-gold-member'>



