Case 9
HISTORY AND PHYSICAL EXAMINATION
Electrodiagnostic (EDX) examination was performed.
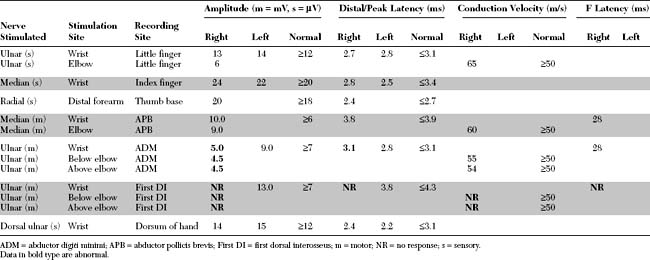
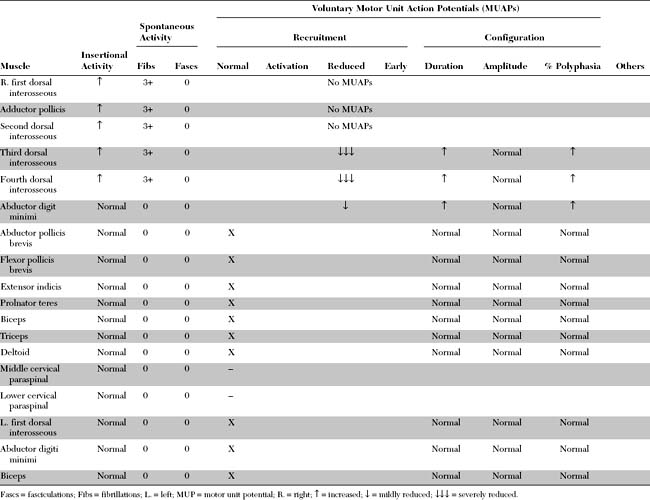
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Pertinent EDX findings include:
This is consistent with ulnar mononeuropathy at the wrist, affecting the motor branch exclusively, distal to the main branch to the hypothenar muscles, but proximal to the branch to the fourth dorsal interosseus (i.e., at the pisohamate hiatus [PHH]). The normal ulnar sensory study rules out a proximal ulnar nerve, or a lower brachial plexus lesion. This case is not due to C8/T1 radiculopathy is because the median CMAP is preserved, and there is no denervation seen in other C8/T1-innervated muscles.
DISCUSSION
Applied Anatomy
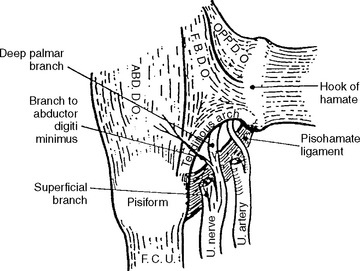
Guyon canal is formed proximally by the pisiform bone and distally by the hook of the hamate. Its floor is formed by the triquetrum and hamate bones along with the thick transverse carpal ligament, while its roof is composed of a loose connective tissue (Figure C9-1). In the distal portion of Guyon canal lies the pisohamate hiatus (PHH). This aperture is bounded anteriorly by a fibrous arch formed by the two musculotendinous attachments of the flexor brevis digiti minimi (or quinti), a hypothenar muscle, to the hook of hamate and the pisiform bone (Figure C9-2). The posterior boundary of the PHH, is formed by a thick pisohamate ligament which extends from the pisiform bone to the hook of the hamate. The origin of the major motor branch to the ADM is proximal to this hiatus in the majority of hands.

Figure C9-1 Anatomy of the ulnar nerve within Guyon canal at the wrist. 1 = ulnar artery, 2 = superficial branch of the ulnar nerve, 3 = hamulus, 4 = fibrous arch of the hypothenar muscles (see also Figure C9-2), 5 = pisiform, 6 = transverse carpal ligament, 7 = palmaris brevis, 8 = palmar carpal ligament.
(From Gross MS, Gelberman RH. The anatomy of the distal ulnar tunnel. Clin Orthop 1985;196:238–247, with permission.)
Clinical Features
Patients with ulnar neuropathy at the wrist often presents with painless unilateral hand atrophy. These ulnar nerve lesions pose a diagnostic challenge, particularly when the weakness is not associated with sensory loss. It is useful in sorting out the cause of hand weakness or atrophy to distinguish between atrophy of all intrinsic hand muscles from atrophy that is restricted to the thenar or hypothenar muscles. Table C9-1 lists the various causes of wasting and weakness of the hand.
Table C9-1 Causes of Unilateral Atrophy and Weakness of Intrinsic Hand Muscles
Several classifications of ulnar mononeuropathy at the wrist have been proposed; most separate the lesions into four types. Table C9-2 lists the common types of ulnar mononeuropathy at the wrist and hand, with their corresponding sites of lesion and clinical presentation. In ulnar neuropathy at the wrist, selective compression of the deep palmar motor branch, with normal superficial sensory branch functions, is the most common type accounting for 39 to 75+ of distal ulnar nerve lesions depending on published series.
Table C9-2 Various Types of Distal Ulnar Mononeuropathy
| Lesion Site | Nerve Affected | Clinical Presentation |
|---|---|---|
| Proximal Guyon canal | Main trunk of ulnar nerve | Ulnar palmar sensory loss and weakness of all ulnar intrinsic hand muscles |
| or | or | |
| Ulnar cutaneous branch | Ulnar palmar sensory loss only | |
| Distal Guyon canal | Deep palmar branch (proximal to branch to the abductor digiti minimi) | Weakness of all ulnar intrinsic hand muscles (interossei, ulnar lumbricals, and hypothenars) without sensory loss |
| Pisohamate hiatus | Deep palmar branch (distal to branch to the abductor digiti minimi) | Weakness of ulnar intrinsic hand muscles with sparing of the hypothenar muscles and without sensory loss |
| Palm (rare) | Deep palmar branch (distal to hypothenars) | Weakness of adductor pollicis, 1st, 2nd, and possibly the 3rd interossei only, usually sparing 4th interossei and without sensory loss |
Table C9-3 lists the common causes of ulnar mononeuropathy at the wrist. A ganglion is the most common cause accounting for 28 to 45+ of cases depending on reported series. The second most common cause is entrapment of the motor branch at the pisohamate hiatus, which may be spontaneous or as an occupational or recreational hazard (such as after prolonged bicycling, use of hand tools, etc.). Compression at this anatomic hiatus explains the selective involvement of the deep motor branch at the wrist with complete or relative sparing of the hypothenar muscles and the normal superficial sensory functions.
Table C9-3 Common Causes of Ulnar Mononeuropathy at the Wrist
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|