Case 8
HISTORY AND PHYSICAL EXAMINATION
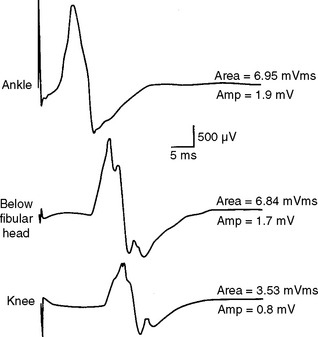
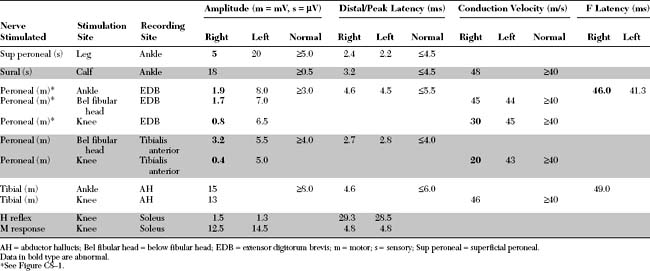
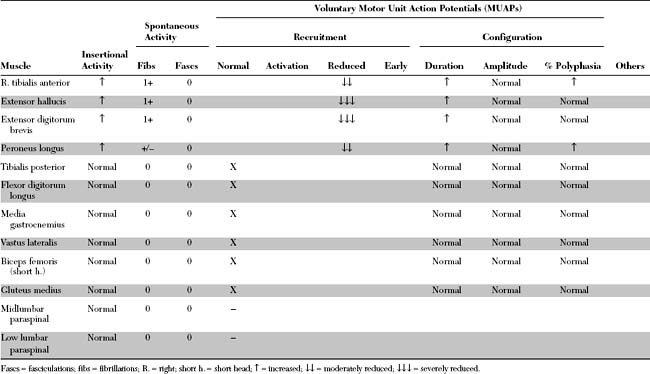
Please now review the Nerve Conduction Studies (NCS) and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Relevant electrodiagnostic (EDX) findings in this case include the following:
DISCUSSION
Applied Anatomy
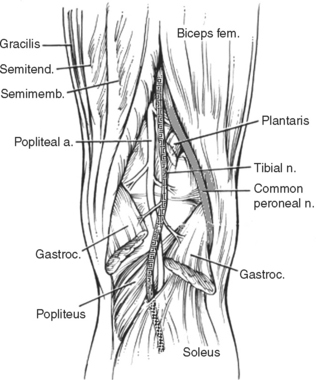
The common peroneal nerve (also called the lateral popliteal nerve) shares a common sheath with the tibial nerve (also called the medial popliteal nerve) to form the sciatic nerve. The common peroneal nerve innervates the short head of biceps femoris only, via a motor branch that exits the nerve close to the gluteal fold. All the other hamstring muscles (long head of biceps femoris, semitendinosus and semimembranosus) are innervated by the tibial nerve. The complete separation of the common peroneal nerve from the tibial nerve is variable, but is usually at the popliteal crease or up to 10 cm above it (Figure C8-2).
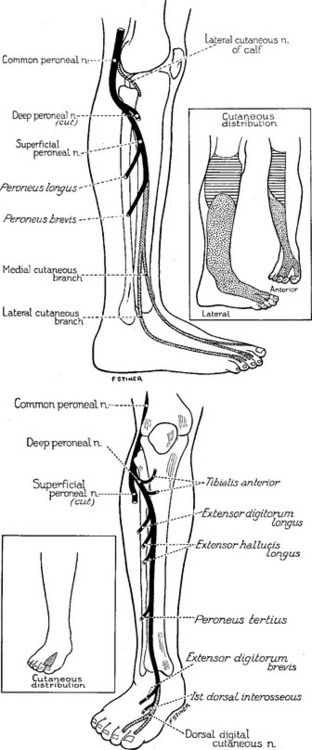
Soon after separating from the tibial nerve in the popliteal fossa, the common peroneal nerve gives off first the lateral cutaneous nerve of the calf, which innervates the skin over the upper third of the lateral aspect of the leg (Figure C8-3, top inset). It also gives the peroneal communicating nerve which joins the sural nerve in midcalf. Then, the common peroneal nerve winds around the fibular neck, where it lies in close contact with it, and passes through a tendinous tunnel between the edge of the peroneus longus muscle and the fibula, sometimes referred to as the fibular tunnel.
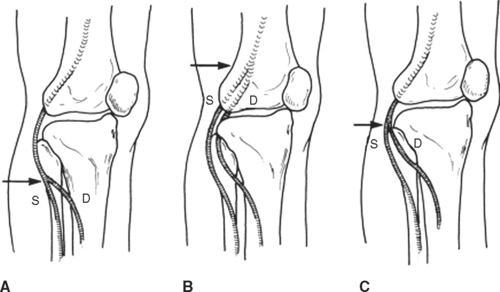
The common peroneal nerve divides into superficial and deep terminal branches usually near the fibular neck but sometimes more proximally (Figure C8-4). The common peroneal nerve around the fibular neck has a topographical arrangement where the fibers to the superficial branch are placed laterally while those destined to the deep peroneal nerve are located medially in close contact with the fibular bone. This renders the deep peroneal nerve more susceptible to compression at the fibular neck than the superficial nerve.
The superficial peroneal nerve innervates the peroneus longus and brevis and the skin of the lower two thirds of the lateral aspect of the leg and the dorsum of the foot (see Figure C8-3, top). The deep peroneal nerve is primarily motor; it innervates all ankle and toe extensors (the tibialis anterior, the extensor hallucis, and the extensor digitorum longus and brevis) and the peroneus tertius, in addition to the skin of the web space between the first and second toes (see Figure C8-3, bottom).
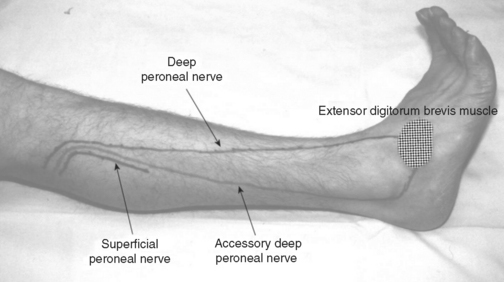
The accessory deep peroneal nerve is a common anomaly of the peroneal nerve. It is present in about 20+ of the population and sometimes bilaterally. The nerve arises as a motor branch of the superficial peroneal nerve, usually a continuation of the muscular branch that innervates the peroneus brevis muscle. The accessory deep peroneal nerve traverses along the posterior aspect of the peroneus brevis muscle, and then, accompanied by peroneus brevis tendon, passes behind the lateral malleolus near the sural nerve to reach the foot. There, it sends branches to the lateral part of extensor digitorum brevis, ankle joint, and ligaments (Figure C8-5).
Clinical Features
Peroneal mononeuropathy usually presents with a foot drop, defined as severe weakness of ankle dorsiflexion (extension) with intact plantar flexion. Foot drop should be distinguished from flail foot which, in contrast, is characterized by no or minimal ankle and foot movements in all directions, including severe weakness of ankle dorsiflexion, plantar flexion, and intrinsic foot muscles. Voluntary movement at or distal to the ankle occur in foot drop due to intact plantar flexion and intrinsic foot muscles, but are absent in flail foot. Table C8-1 lists the common causes of unilateral and bilateral footdrop, starting caudally and progressing cephalad along the neuraxis.
Table C8-1 Causes of Unilateral and Bilateral Footdrop
Unilateral footdrop
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|