Case 7
HISTORY AND PHYSICAL EXAMINATION
The patient was referred to the electromyography (EMG) laboratory.
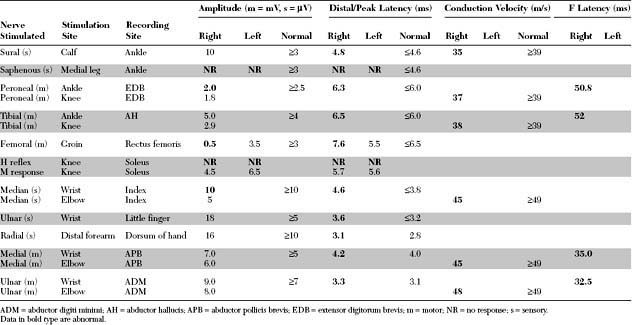
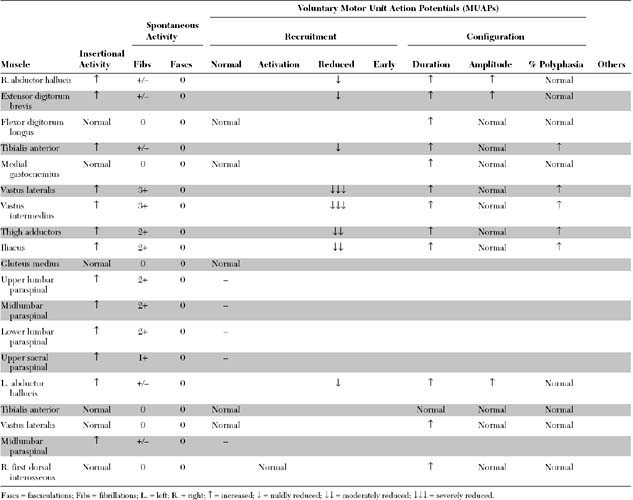
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Relevant EDX findings in this case include:
Discussion
Definition and Classification
The classification of diabetic neuropathies cannot be rigid because many overlap syndromes may be seen. A practical categorization, based on clinical presentation rather than precise etiology, divides these neuropathies into distal symmetrical polyneuropathy (the commonest), asymmetrical polyradiculoneuropathy, cranial mononeuropathy, and entrapment mononeuropathy (Table C7-1). Detailed discussions of all these syndromes are beyond the scope of this section and have been summarized in recent reviews (see Bird and Brown 2002; Brown and Asbury 1984; Harati 1987; Wilbourn 1993).
Table C7-1 Classification of Diabetic Neuropathy
* Common mononeuropathies with increased incidence in diabetics.
Clinical Features
Diabetic Sensorimotor Autonomic Polyneuropathy
Diabetic neuropathies are by far the most prevalent peripheral neuropathies encountered in clinical practice. Among all diabetic neuropathies, the mixed sensory-motor-autonomic peripheral polyneuropathy is by far the most common, and is usually related to the duration and severity of hyperglycemia. However, this form may occasionally be the presenting symptom of occult diabetes mellitus. The exact incidence of this diabetic polyneuropathy is not known; this is, in part, because of its diverse clinical presentations and different measurements used to define the presence or absence of neuropathy (Table C7-2). The reported incidence of diabetic neuropathy in general is extremely variable, ranging from 5 to 50+. In a large cohort study followed for 25 years, it was estimated that 8+ of diabetics have neuropathy at the time of diagnosis, and neuropathy develops in 50+ of patients within 25 years of diagnosis (see Pirart 1978).
Table C7-2 Available Measures That May Be Used to Assess for Diabetic Peripheral Polyneuropathy
Autonomic testing
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|