Case 5
HISTORY AND PHYSICAL EXAMINATION
An electrodiagnostic (EDX) examination was requested.
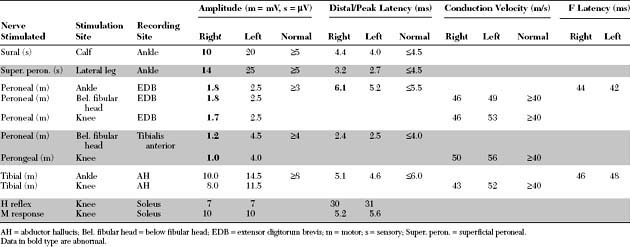
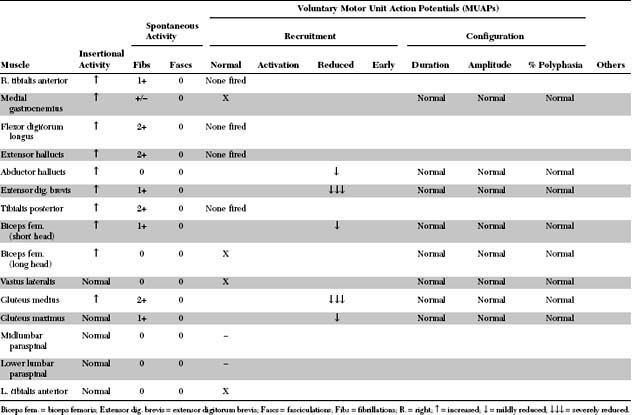
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
The relevant electrodiagnostic findings in this case are the followings:
1. The superficial peroneal and sural sensory nerve action potentials (SNAPs) were lower in amplitudes on the affected limb when compared with the asymptomatic limb. This excludes root(s) lesions because it places the lesion distal to the dorsal root ganglia, as seen with either a plexus or peripheral nerve lesions.
2. The peroneal compound muscle action potentials (CMAPs) were borderline to low in amplitude following all stimulation sites (ankle, below fibula neck, and knee) without evidence of focal slowing or conduction block. Also, the peroneal CMAPs, recording the tibialis anterior, were more affected than when recording the extensor digitorum brevis. In contrast, tibial CMAPs, H reflexes, and M responses were normal and symmetrical.
4. Needle muscle examination showed significant decrease in recruitment of motor unit action potentials (MUAPs) and variable fibrillation potentials in all L5-innervated muscles, with normal paraspinal muscles.
DISCUSSION
Applied Anatomy
The lumbosacral plexus is divided anatomically into the lumbar plexus and the sacral plexus with a connecting nerve trunk, the lumbosacral trunk (Figure C5-1).
• The lumbar plexus is formed from the ventral rami of L1, L2, L3, and most of the L4 roots. These rami divide near the vertebral column into dorsal and ventral branches. The dorsal branches of L2, L3, and L4 roots combine to form the femoral nerve, while the ventral branches of these same roots join to form the obturator nerve. The lumbar plexus gives also rise to direct motor branches to the underlying iliacus and psoas muscles, and to the ilioinguinal, iliohypogastric, genitofemoral, and lateral femoral cutaneous nerves.
• The lumbosacral trunk (also called the lumbosacral cord) is formed primarily by the L5 root, with a contributing branch from the L4 root (see Figure C5-1). It then travels a relatively long distance in close contact with the ala of the sacrum, which is adjacent to the sacroiliac joint. It is covered throughout its course by the psoas muscle, except at its terminal portion near the bony pelvic rim, where it is joined by the S1 root. Many fibers within the lumbosacral trunk are destined to reach the common peroneal nerve, and they terminate primarily in muscles of the lateral compartment of the leg.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree