Case 4
HISTORY AND PHYSICAL EXAMINATION
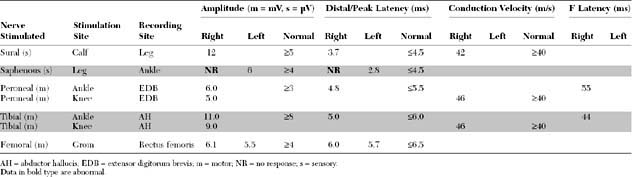
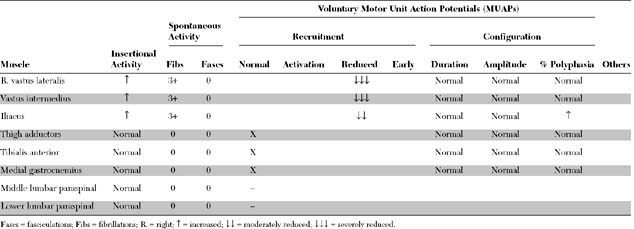
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
The pertinent electrodiagnostic (EDX) findings in this case include:
The prognosis for recovery is good because the distal femoral CMAP amplitude is normal, consistent with a predominant proximal demyelination. Note that the femoral nerve may be stimulated only at the inguinal canal distal to the location of the pelvic lesion. Some axonal loss obviously has occurred, based on the fibrillations and the absent saphenous SNAP, but these findings have no prognostic value for the outcome of motor function.
DISCUSSION
Applied Anatomy
The femoral nerve emerges from the iliacus compartment after passing underneath the rigid inguinal ligament in the groin. About 4–5 cm before crossing the inguinal ligament, it innervates the iliacus muscle. Soon after passing under the inguinal ligament (lateral to the femoral vein and artery), the femoral nerve branches widely into (1) terminal motor branches to all four heads of the quadriceps (rectus femoris, vastus lateralis, vastus intermedius, and vastus lateralis) and sartorius muscles, and (2) three terminal sensory branches, the medial and intermediate cutaneous nerve of the thigh which innervate the skin of the anterior thigh, and the saphenous sensory nerve (Figure C4-1).
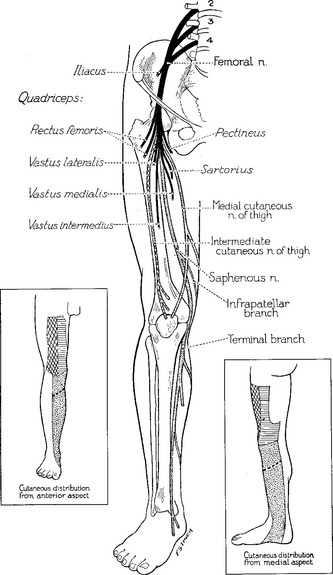
Figure C4-1 The femoral nerve and its terminal motor and sensory branches including the saphenous nerve.
(From Haymaker W and Woodhall B. Peripheral nerve injuries: principles of diagnosis. Philadelphia, PA: WB Saunders, 1953, with permission.)
Clinical Features
The femoral nerve is a relatively short nerve. Its main trunk can be compressed at the inguinal ligament or in the retroperitoneal pelvic space. Most femoral mononeuropathies are iatrogenic, occurring during intra-abdominal, intrapelvic, inguinal, or hip surgical or diagnostic procedures. The nerve injury often results from direct nerve trauma or poor leg positioning during one of these procedures but may be due to a compressive hematoma or rarely due to inadvertent nerve laceration, suturing or stapling. Table C4-1 lists the various causes of femoral mononeuropathy grouped according to the site of injury.
Table C4-1 Common Causes of Femoral Mononeuropathy
1. Compression in the pelvis
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|