Case 3
HISTORY AND PHYSICAL EXAMINATION
An electrodiagnostic (EDX) examination was performed.
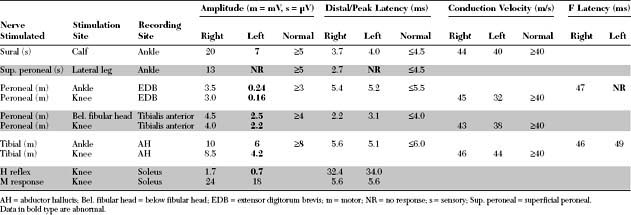
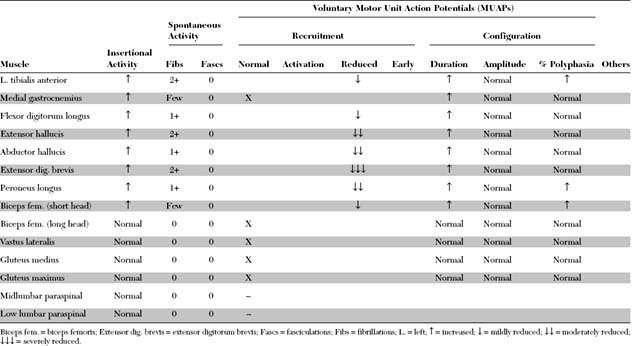
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Pertinent EDX findings include:
DISCUSSION
Applied Anatomy
The sciatic nerve (Figure C3-1) leaves the pelvis via the sciatic notch and then passes, usually, under the piriformis muscle, which is covered by the gluteus maximus. In healthy individuals, the sciatic nerve passes underneath the piriformis muscle in 85 to 90+ of cases, while in the rest, the peroneal division only passes above or through the muscle. Rarely (1 to 2+ of persons), the entire sciatic nerve pierces the piriformis muscle.
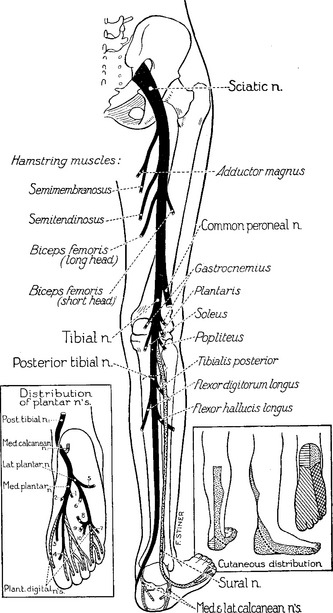
Figure C3-1 The sciatic nerve and its main branches.
(Reprinted with permission from Haymaker W, Woodhall B. Peripheral nerve injuries: principles of diagnosis. Philadelphia, PA: WB Saunders, 1953.)
The superior gluteal nerve, which innervates the gluteus medius and minimus and tensor fascia lata, branches off the sciatic trunk before the piriformis. However, the inferior gluteal nerve, which innervates the gluteus maximus, passes under the muscle (Figure C3-2). In the thigh, the tibial nerve innervates most hamstring muscles (semitendinosus, semimembranosus, and the long head of the biceps femoris), except the short head of the biceps femoris; the latter is the only hamstring muscle innervated by the common peroneal nerve. Also, the tibial nerve contributes, with the obturator nerve, to innervation of the adductor magnus muscle.
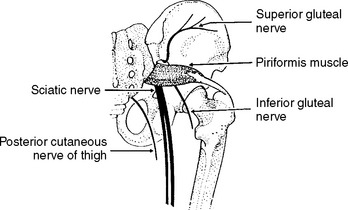
Figure C3-2 The nerve of the sciatic notch and the piriformis muscle.
(Reprinted from Stewart JD. Focal peripheral neuropathies, 2nd ed. New York: Raven Press, 1993, with permission.)
The sciatic nerve divides into its two terminal branches near the midthigh, although this is extremely variable and the separation may be as low as the popliteal fossa. In the popliteal fossa and before it winds around the fibular neck, the common peroneal nerve gives off first the lateral cutaneous nerve of the calf, which innervates the skin over the upper third of the lateral aspect of the leg. At the fibular neck, the common peroneal nerve lies in close contact with the bone, and passes through a tendinous tunnel, sometimes referred to as the fibular tunnel, which is formed between the edge of the peroneus longus muscle and the fibula. Near that point, the common peroneal nerve divides into superficial and deep branches (see Figure C8-3, Case 8). The superficial peroneal nerve innervates the peroneus longus and brevis, as well as the skin of the lower two-thirds of the lateral aspect of the leg and the dorsum of the foot. The deep peroneal nerve is primarily a motor nerve; it innervates the ankle and toe extensors (the tibialis anterior, extensor hallucis, extensor digitorum longus, and brevis) and the peroneus tertius, in addition to a small area of skin in the web space between the first and second toes.
While in the calf, the tibial nerve innervates the gastrocnemius, soleus, tibialis posterior, flexor digitorum profundus, and flexor hallucis longus. At the medial aspect of the ankle, the tibial nerve passes through the tarsal tunnel and divides at, or slightly distal to, the tunnel into its three terminal branches (see inset of Figure C3-1): (1) the calcaneal branch, a purely sensory nerve that innervates the skin of the sole of the heel; (2) the medial plantar nerve, which innervates the abductor hallucis, the flexor digitorum brevis, and the flexor hallucis brevis, in addition to the skin of the medial sole and, at least, the medial three toes; and (3) the lateral plantar nerve, which innervates the abductor digiti quinti pedis, the flexor digiti quinti pedis, the adductor hallucis, and the interossei, in addition to the skin of the lateral sole and two lateral toes.
Clinical Features
Table C3-1 lists the common causes of sciatic mononeuropathy. Total hip joint replacement is currently a leading cause of such lesions, and sciatic nerve injury is the most common neurologic complication of total hip arthroplasty, particularly with revisions or procedures requiring limb lengthening, and in patients with congenital hip dislocation or dysplasia. The estimated incidence of sciatic nerve lesion following total hip replacement is about 1–3+, although EDX studies may detect subclinical signs of sciatic nerve damage in as many as 70+ of patients. The sciatic nerve lesion is due to direct intraoperative stretch injury, but occasionally is caused by hemorrhage, prosthetic dislocation, migrating trochanteric wire, or leaking cement (methylmethacrylate) used in the arthroplasty. The manifestations of the sciatic nerve injury are acute and often noted in the immediate postoperative period. Occasionally, the onset of symptoms is delayed for several years, and the injury is due to prosthetic dislocation, osseous formation, or migrating trochanteric wire. Hip fracture or dislocation, or femur fracture may also result in sciatic nerve injury, which may also occur during closed reduction or internal fixation. External compression of the sciatic nerve is the second common cause of sciatic nerve lesions at the hip. This usually occurs in the setting of unattended coma (such as with drug overdose), but occasionally follows operative positioning in the sitting position (such as with craniotomy), poor positioning of unconscious patient (such as in the intensive care unit), or prolonged sitting (“toilet seat” and “lotus” neuropathies). Mass lesions in the buttock or thigh, such as malignant or benign tumors, persistent sciatic artery, or enlargement of the lesser trochanter (possibly from frequent sitting on hard benches), may compress the sciatic nerve. Open injuries of the sciatic nerve are usually caused by gunshot wounds, knives, or other sharp objects. Hemorrhage within the gluteal compartment is sometimes associated with sciatic nerve lesions. This may occur during anticoagulant therapy, in hemophiliacs, or following rupture of an iliac artery aneurysm or hip surgery. Intramuscular gluteal injections, not administered properly in the upper outer quadrant of the buttock particularly in thin patients or children, may damage the sciatic nerve or its peroneal component exclusively. This often occurs soon after the injection of a large quantity of a neurotoxic drug but may be delayed following repeated injections or due to fibrosis. Menstruating women with endometriosis may have cyclic radicular pain (i.e., sciatica) or overt sciatic mononeuropathy. Typically, the symptoms start few days before menstruation and stop after menses end. With progression of disease, the manifestations of endometriosis become more constant, though often worse during menses. Ischemia resulting in sciatic nerve injuries may be due to vasculitis involving the vasa nervorum, or occlusion of the iliac or femoral artery such as during intra-aortic balloon pump therapy with a catheter placed through the ipsilateral femoral artery. Occasionally, a slowly progressive sciatic mononeuropathy is idiopathic and no identifiable cause is identified despite imaging studies and surgical exploration.
Table C3-1 Common Causes of Sciatic Mononeuropathy (Listed in Descending Order of Frequency)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|