Case 26
HISTORY AND PHYSICAL EXAMINATION
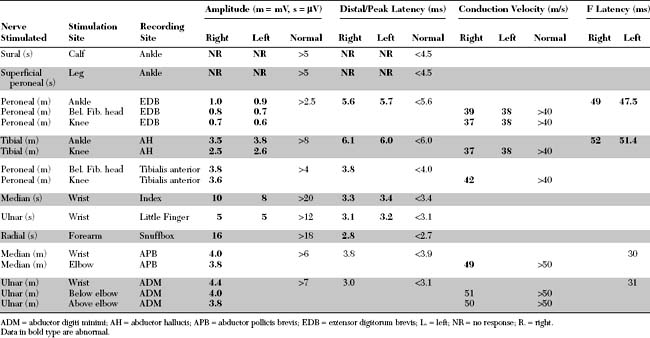
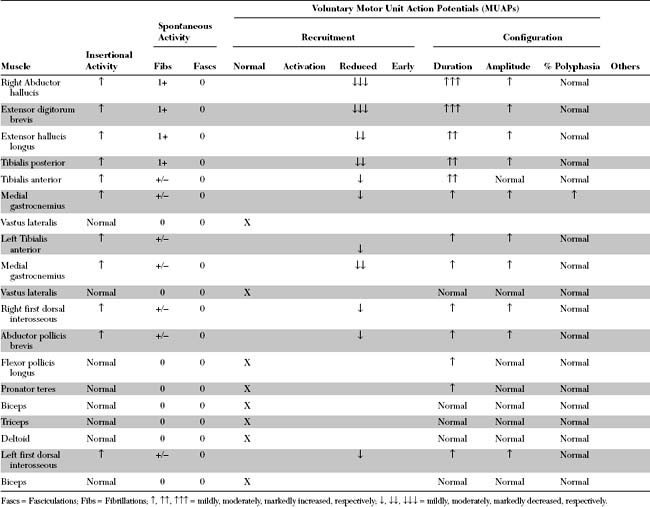
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
The abnormal EDX findings in this case include:
DISCUSSION
Definition and Pathogenesis
Peripheral Polyneuropathy
The myriad of etiologies of peripheral neuropathy pose a daunting task for the clinician. Investigating peripheral neuropathy has included several approaches. First, is the pattern recognition approach where a diagnosis of a polyneuropathy is based on highly specific associated findings such as the Mee line in arsenic or thallium poisoning, red tongue in vitamin B12 deficiency, or predilection of the sensory loss to cool areas of the body (such as earlobes, nipples, and buttock) in leprosy. Unfortunately, this approach applies to a minority of patients usually with advanced disease, requires a vast clinical experience and is mostly accomplished by senior neurologists. The second approach frequently used by many physicians (including some neurologists) is a “shotgun” approach by ordering a battery of tests on every patient with a neuropathy. This irrational approach is costly and may result in incorrect diagnosis secondary to incidental abnormalities, such as elevated blood glucose in a patient with CIDP. The third recommended approach is a systematic approach that utilizes mainly the clinical findings and EDX studies to generate a more limited differential diagnosis and help guide the laboratory investigations necessary for establishing a final diagnosis (Table C26-1). Additional studies that are useful in the accurate diagnosis of peripheral neuropathy include autonomic testing, quantitative sensory testing, antibody testing, and skin or cutaneous nerve biopsy.
Table C26-1 Essential Steps in the Classification and Etiologic Diagnosis of Peripheral Polyneuropathy
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|