Case 24
HISTORY AND PHYSICAL EXAMINATION
On examination on day 4, the patient was alert and intubated, and followed commands well. He had bilateral complete ophthalmoplegia to all gaze directions with bilateral ptosis (Figure C24-1). Pupils were dilated and unreactive to light or attempted accommodation. Corneal reflexes were depressed. The patient had bilateral peripheral facial weakness. His tongue was extremely weak, with no fasciculations. His palate did not move volitionally or to gagging. Neck flexors and extensors were weak (Medical Research Council [MRC] 3/5), as were proximal pelvic and shoulder girdle muscles (4/5). However, distal muscles were normal. Deep tendon reflexes were depressed (1/4). Sensation was normal. Cerebellar function also was normal.
An electrodiagnostic (EDX) examination was requested.
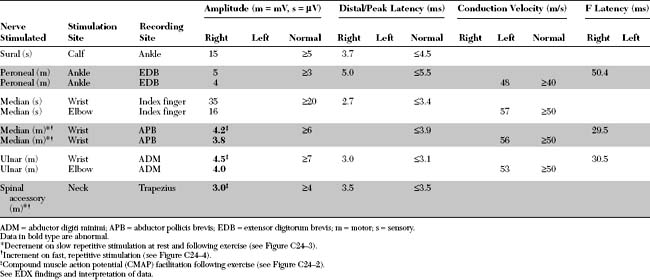
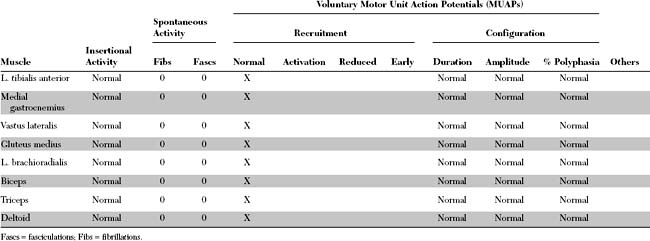
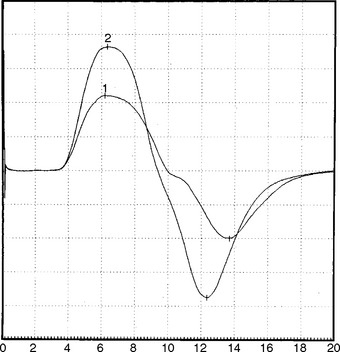
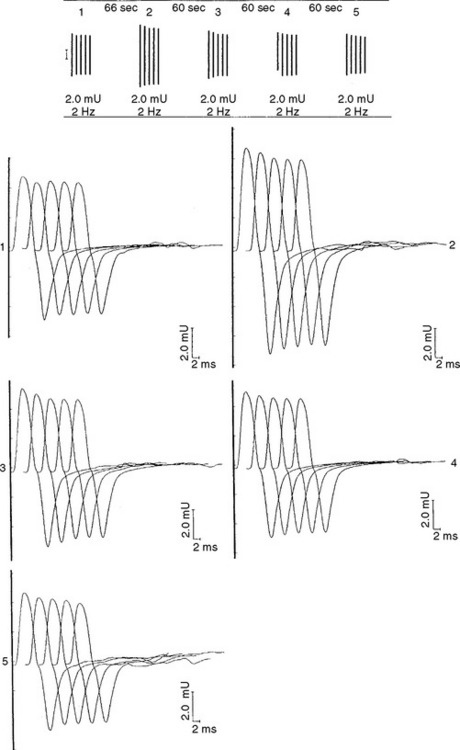
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
The relevant EDX findings in this case are:
The EDX findings are consistent with a neuromuscular junction disorder of the presynaptic type, as supported by the borderline or low-amplitude baseline CMAPs, and the significant increment (>50%) of the CMAP amplitude after brief exercise and rapid repetitive stimulation of motor nerves. This case is consistent with botulism based on subacute progression of a descending muscle paralysis (ocular to bulbar to limbs), the muscarinic involvement (pupillary dilatation), and the EDX findings (presynaptic blockade). It is not consistent with Lambert-Eaton myasthenic syndrome because of the rapid evolution of symptoms, the prominent oculobulbar muscle weakness, and the relatively modest increment on rapid repetitive stimulation and after brief exercise (see electrodiagnosis).
DISCUSSION
Physiology and Pathophysiology
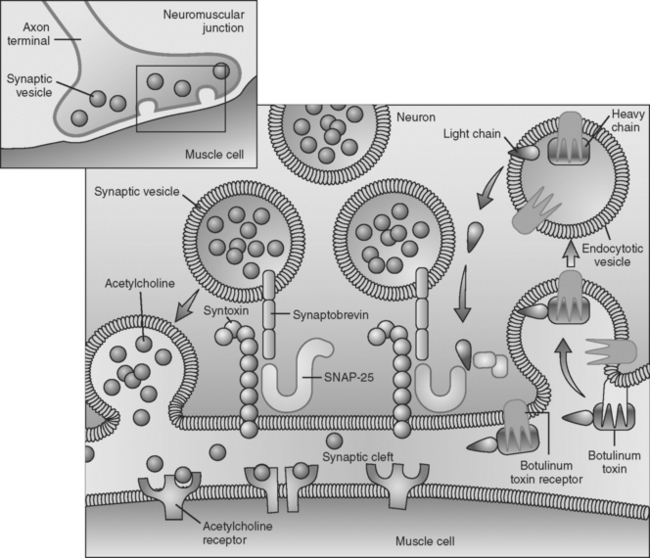
Botulinum toxin is an extremely potent toxin with doses as small as 0.05 to 0.1 μg causing death in humans. The toxin has significant affinity to both muscarinic and nicotinic cholinergic nerve terminals resulting in autonomic failure and skeletal muscle paralysis. The toxin results in failure of ACH release from the presynaptic terminal and ultimately leads to destruction of the presynaptic terminal. Botulinum toxin first attaches irreversibly to the axonal terminal, and enters via endocytosis without interfering with the calcium channel (calcium entry is not blocked by botulinum toxin). The toxin then interferes with the calcium-dependent intracellular cascade that is responsible for ACH release, by cleaving proteins essential for docking and fusion of the presynaptic vesicles at the presynaptic active zones. Electron microscopy of nerve endings exposed to the toxin reveal a “log jam” of vesicles in the presynaptic terminals. It is now known that various serotypes bind to different presynaptic proteins: botulinum toxin A and E hydrolyze synaptosomal-associated protein-25 (SNAP-25), a protein of the presynaptic membrane; botulinum toxins B, D, F, and G specifically cleave synaptobrevin, a membrane protein of the neurotransmitter-containing vesicles; botulinum toxin C cleaves both SNAP-25 and syntaxin, a nerve plasmalemma protein (Figure C24-5). Because the ultimate result of this intoxication is interference with neurotransmitter release (exocytosis of synaptic vesicles) and destruction of the nerve terminals, recovery of neurologic function is protracted since it is dependent on the regrowth of sprouts from the injured nerve terminal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree