Case 22
HISTORY AND PHYSICAL EXAMINATION
An electrodiagnostic (EDX) examination was performed.
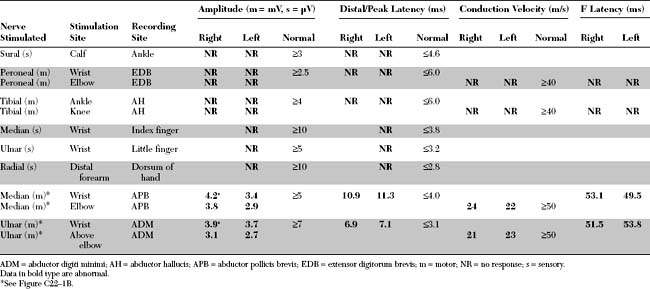
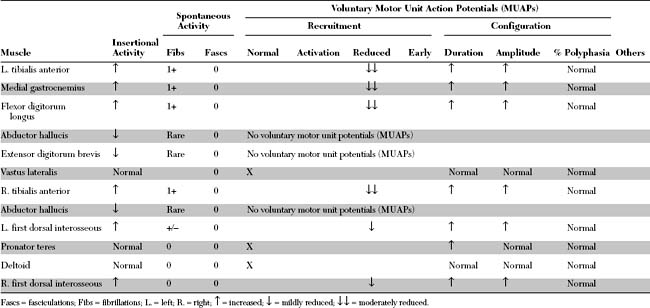
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
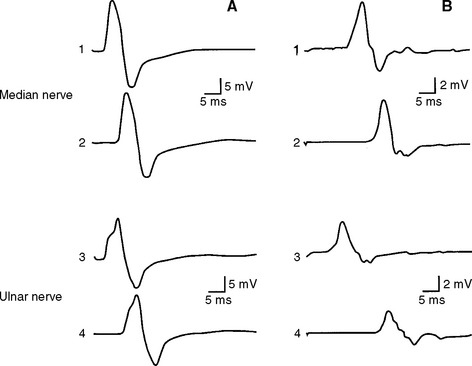
Relevant EDX findings in this case include:
DISCUSSION
Classification
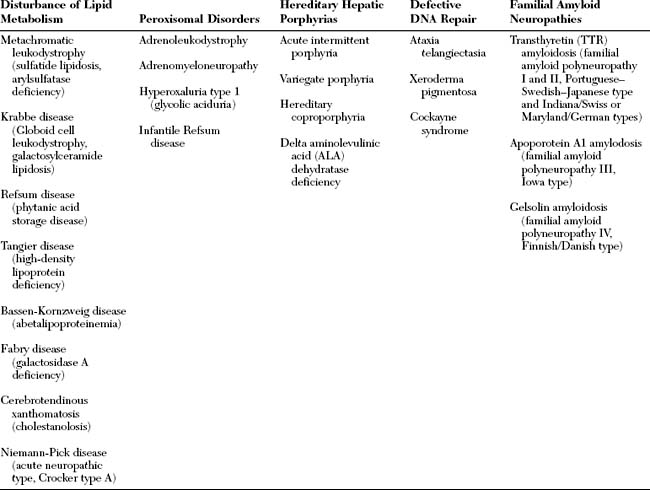
Hereditary neuropathies are a heterogeneous group of peripheral nerve disorders (Figure C22-2). Some have a known metabolic basis and potential therapies (Table C22-1). The hereditary neuropathies that are not based on known specific metabolic defect are classified into three clinical groups: (1) hereditary motor and sensory neuropathies (HMSNs); (2) hereditary sensory and autonomic neuropathies (HSANs); and (3) hereditary motor neuropathies (HMNs).
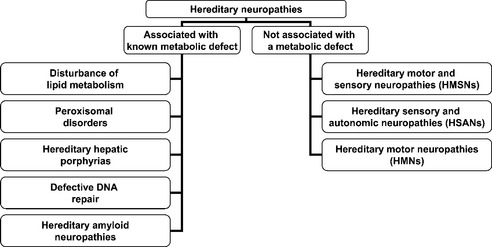
Figure C22-2 Classification of hereditary neuropathies.
(Adapted, with revisions, from Thomas PK. Classification and electrodiagnosis of hereditary neuropathies. In: Brown WF, Bolton CF, eds. Clinical electromyography, 2nd ed. Boston, MA: Butterworth-Heinemann, 1993, pp. 391–425.)
The hereditary motor and sensory neuropathies (HMSNs) were classified by Dyck and Lambert into three predominant types (1) HMSN I, a demyelinating type; (2) HMSN II, a neuronal (axonal) type; and (3) HMSN III (Dejerine-Sottas disease), a severe demyelinating neuropathy of infancy and early childhood. HMSN I and II are characterized by skeletal deformities (pes cavus, hammer toes, scoliosis), insidious onset of distal lower more than upper extremities weakness, atrophy and sensory loss, and reduced or absent deep tendon reflexes. Based on clinical examination, these disorders are difficult to distinguish from each other because of similar phenotypes. With the recent influence of chromosomal linkage and gene identification, the term Charcot-Marie-Tooth disease (CMT) reemerged which created some confusion in the nomenclature and classifications of these disorders.
Charcot-Marie-Tooth disease (CMT) is subdivided into six major types with some but not perfect correlation to the HMSN classification (Table C22-2). CMT1 and CMT2 are interchangeable with HMSN I and HMSN II. The name Dejerine-Sottas syndrome (DSS, Dejerine-Sottas disease) is preserved and is the same condition as HMSN III. The term CMT3 is not commonly used since the genes involved with DSS are the same as CMT1. CMT4 is a new designation for a group of autosomal recessive CMT and should not be confused with HMSN IV which is Refsum disease. CMTX is an X-linked disorder and hereditary neuropathy with liability to pressure palsy (HNPP) is a distinct disorder characterized by recurrent mononeuropathies.
Table C22-2 Charcot-Marie-Tooth Disease (CMT, Hereditary Motor and Sensory Neuropathy, HMSN) Subtypes, Its Variants and Their Genetic Causes
| Disorder | Locus/Gene | Protein |
|---|---|---|
| Charcot-Marie-Tooth Disease Type 1 (CMT1, HMSN I, Autosomal-Dominant, Demyelinating) | ||
| CMT1A | 17p11.2-12/PMP22* | Peripheral myelin protein 22 |
| CMT1B | 1q22-23/MPZ | Myelin protein zero |
| CMT1C | 16p13.1-12.3/LITAF | SIMPLE |
| CMT1D | 10q21.1-22.1/EGR2 | Early growth response protein 2 |
| Charcot-Marie-Tooth Disease Type 2 (CMT2, HMSN II, Autosomal-Dominant, Axonal) | ||
| CMT2A | 1p35-36/KFI1B | Kinesin-like protein Mitousin 2 |
| CMT2B | 3q13-22/RAB7 | Ras-related protein |
| CMT2C | 12q23-24/? | ? (unknown) |
| CMT2D | 7p15/GARS | Glycy-tRNA synthetase |
| CMT2E | 8P21/NEFL | Neurofilament triplet L protein |
| CMT2F | 7q11-21/HSP27 | Small heat shock protein |
| CMT2 | 1q22/MPZ | Myelin protein zero |
| Dejerine-Sottas Syndrome (DSS, HMSN III, CMT3, Autosomal-Dominant or Recessive, Demyelinating) | ||
| DSS A | 17p/PMP22 | Peripheral myelin protein 22 |
| DSS B | 1q/MPZ | Myelin protein zero |
| DSS C | 10q/EGR2 | Early growth response protein 2 |
| DSS D | 8q23 | Unknown |
| Charcot-Marie-Tooth Disease Type 4 (CMT4, Autosomal-Recessive, Axonal or Demyelinating) | ||
| CMT4A | 8q13-21/GDAP1 | Ganglioside-induced differentiation-associated protein-1 |
| CMT4B1 | 11q22/MTMR2 | Myotubularin-related protein-2 |
| CMT4B2 | 11p15/MTMR13 | Myotubularin-related protein-13 |
| CMT4C | 5q23-33/KIAA1985 | − |
| CMT4D | 8q24.3/NDRG1 | N-myc downstream-regulated gene-1 |
| CMT4E | 10q21.1-22.1/EGR2 | Early growth response protein 2 |
| CMT4F | 19q13.1-13.2/PRX | Periaxin gene |
| X-linked Charcot-Marie-Tooth Disease (CMTX, Axonal or Demyelinating) | ||
| CMTX (X-linked) | Xq13-q21/CX32(GJB1) | Connexin 32 (gap junction protein-β-1) |
| Hereditary Neuropathy with Liability to Pressure Palsy (HNPP, Demyelinating) | ||
| HNPP (autosomal dominant) | 17p11.22/PMP22† | Peripheral myelin protein 22 |
* Duplication (98%) and point mutation (2%).
† Deletion (80%) and point mutation (20%).
The hereditary sensory and autonomic neuropathies (HSANs) are very rare and familial neuropathies with selective involvement of the primary sensory, with or without the autonomic, fibers. They should be distinguished from inherited disorders that affect large primary afferent neurons (spinocerebellar degeneration). They are currently subdivided into five types, based on mode of inheritance, natural history, electrophysiologic characteristics and histopatologic findings (Table C22-3).
Table C22-3 Hereditary Sensory and Autonomic Neuropathy (HSAN)
| Disorder | Locus/Gene | Protein |
|---|---|---|
| HSAN I (hereditary sensory radicular neuropathy) | 9q22.1-q22.3/SPTLC1 | Serine-palitoyltransferase-1 |
| HSAN II (congenital sensory neuropathy) | 12p13-33 | |
| HSAN III (familial dysautonomia, Riley-Day syndrome) | 9q31-33/IKBKAP | Inhibitor of kappaB-kinase complex associated polypeptide |
| HSAN IV (congenital sensory neuropathy with anhidrosis) | 1q21-22/TRKA | |
| HSAN V | 1q21-22/NTRK1 |
The hereditary motor neuropathies (HMNs) are loosely subdivided into proximal and distal (Table C22-4). The proximal HMNs are better known as spinal muscular atrophies (SMAs). These are among the most common autosomal recessive disorders in childhood affecting 1/10 000 live births with carrier frequency of 1/50. Spinal muscular atrophy is caused by a deficiency of the ubiquitous survival motor neuron (SMN) protein, which is encoded by the SMN genes, SMN1 and SMN2, on chromosome 5q. The distal HMNs are a genetically and clinically heterogeneous group of disorders that are also known as spinal CMT because of their overlap with CMT. They are characterized by distal weakness with or without foot deformities, but without sensory or autonomic involvement. Sensory nerve action potentials are normal while the motor NCSs reveal low-amplitude CMAPs with normal or borderline velocities, consistent with motor axonopathy. The inheritance of HMNs is either dominant or recessive. Only few have been mapped to a chromosome or have a defined gene mutation.
Table C22-4 Hereditary Motor Neuropathy (HMN)
| Proximal HMN (Spinal Muscular Atrophy, SMA, Autosomal-Recessive, Mutations of the Survival Motor Neuron 1 (SMN 1) Gene on Chromosome 5q13) | |
| SMA I | Werdnig-Hoffmann disease. Onset before the age of 6 months, inability to sit or walk, and fatal before the age of 2 years |
| SMA II | Intermediate, arrested Werdnig-Hoffmann disease. Onset between 6 and 18 months of age, able to sit but not walk and survive beyond the age of 4 years |
| SMA III | Kugelberg-Welander disease |
| SMA IIIa | Onset between the age of 2 to 3 years, survive into adulthood and able to walk independently usually until age 20–40 years |
| SMA IIIb | Onset after the age of 3 years and able to walk independently till age 30–50 years |
| SMA IV | Adult SMA. Variable age of onset, but rarely before the age of 20 years and usually after the age of 30 years |
| Bulbospinal (Kennedy Disease, X-Linked CAG Repeat Expansion of the Androgen Receptor Gene on Chromosome Xq13.1) Distal HMN (Spinal Form of Charcot-Marie-Tooth Disease) | |
| HMN I | Juvenile onset, autosomal dominant |
| HMN II | Adult onset, autosomal dominant (12q24) |
| HMN III | Mild juvenile, autosomal recessive (11q13) |
| HMN IV | Severe juvenile, autosomal recessive |
| HMN V | Upper limb predominance, autosomal dominant (7p) |
| HMN VI | Severe infantile with respiratory distress, autosomal recessive |
| HMN VII | Vocal cord paralysis, autosomal dominant (9p21.1-p12) |
| Scapuloperoneal | |
| Type I | Autosomal dominant |
| Type II | Autosomal recessive |
| Bulbar | |
| Type I | Autosomal recessive (Vialetto-Van Laere syndrome) |
| Type II | Autosomal recessive (Fazio-Londe disease) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree