Case 2
HISTORY AND PHYSICAL EXAMINATION
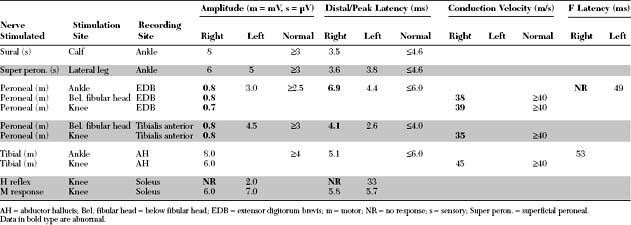
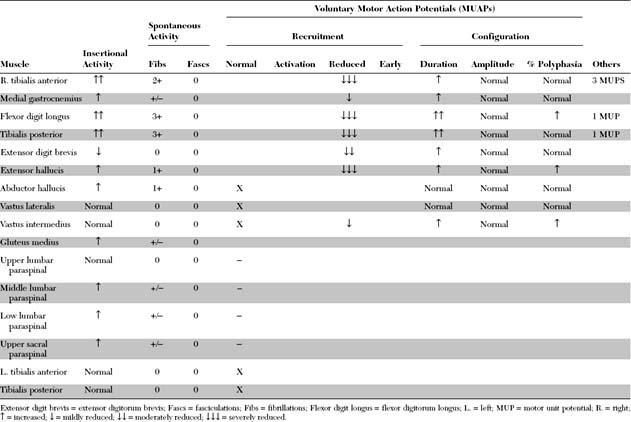
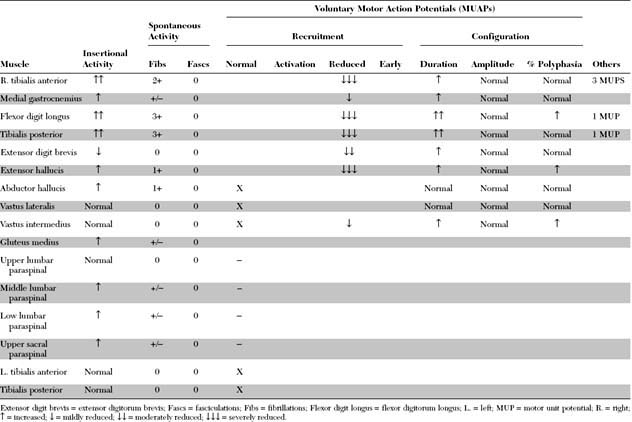
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Relevant EDX findings in this patient are:
DISCUSSION
Applied Anatomy
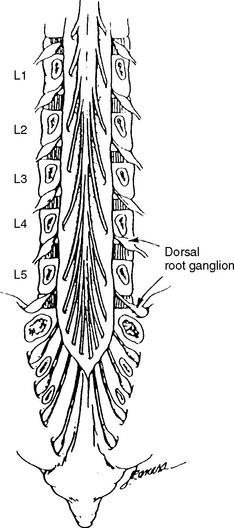
The dorsal root axons originate from the sensory neurons of the dorsal root ganglia (DRG), which lie outside the spinal canal within the intervertebral foramen (Figure C2-1), and immediately before the dorsal and ventral roots are joined. These sensory neurons are unique because they are unipolar. They have proximal projections through the dorsal root, called the preganglionic sensory fibers, which extend to the dorsal horn and column of the spinal cord. The distal projections of these neurons, called the postganglionic sensory fibers, join the motor fibers in the ventral root to form the spinal nerve, and then pass through the corresponding peripheral nerve to reach their respective sensory end-organs. The ventral root axons are mainly motor, and originate from the anterior horn cells within the spinal cord. Passing through the spinal nerves and the peripheral nerve, these motor fibers terminate in the corresponding muscles. At each intervertebral foramen, a mixed spinal nerve is formed by the fusion of the dorsal (afferent, sensory) and ventral (efferent, motor, and sympathetic) roots. Nerve roots have no epineurium and less collagen than peripheral nerves, which result in increased susceptibility to compression, stretch, and infiltration.
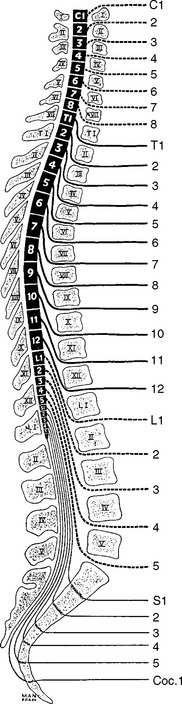
In humans, there are 31 pairs of spinal nerve roots: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal. In the cervical spine, each cervical root exits above the corresponding vertebra that shares the same numeric designation. For example, the C5 root exits above the C5 vertebra (i.e., between the C4 and C5 vertebrae). Because there are seven cervical vertebrae but eight cervical roots, the C8 root exits between the C7 and T1 vertebrae; subsequently, all thoracic, lumbar, and sacral roots exit below their corresponding vertebrae (Figure C2-2). For example, the L3 root exits below the L3 vertebra (i.e., between the L3 and L4 vertebrae).
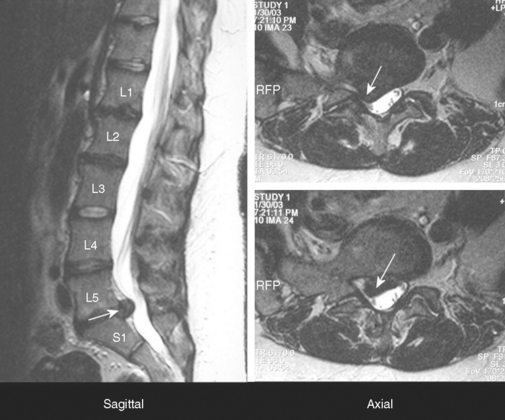
In adults, the spinal cord ends at the L1 vertebra, resulting in a disparity between the lengths of the vertebral column and the spinal cord. Hence, spinal cord segments, mostly the thoracic and lumbar, are higher than the corresponding vertebras. This disparity is most pronounced in the lumbar region where there is a difference of approximately three segments, while there is usually a two-segment disparity in the thoracic region (see Figure C2-2). Since the cord terminates at L1 vertebra, the lumbosacral roots traverse relatively long intraspinal courses before exiting through their respective intervertebral foramina, thus forming the cauda equina. Due to the intricate anatomic relationships between the cauda equina and lumbar spinal column, a disc herniation at one level may injure different nerve roots and the vertebral level of a lumbosacral root compression does not always correlate with its exit level. For example, the S1 root is most often compressed by a posterolateral L5–S1 disc herniation (Figure C2-3). Also, the L5 root may be compressed by any disc herniation up to the level of conus medullaris at or rostral to L5–S1 (see Figure C2-2), including a lateral L5–S1 disc herniation and a posterolateral L4–L5 disc herniation. Less often, the L4–L5 disc may protrudes laterally into the foramen at that level and compress the exiting L4 root. If large, the lateral disc may injure both the L4 and L5 roots. Finally, if the L4–L5 disc herniation is central, it may compress several roots on one or both sides of the cauda equina, often asymmetrically.
Clinical Features
Low back pain is an extremely common symptom, but only a relatively small number of patients with low back pain have root compression in the lumbar region. Lumbosacral radiculopathy may be due to a variety of causes (Table C2-1), but is often caused by disc herniation, spondylitic changes (especially at the facetal joints leading to foraminal stenosis), or calcification of the ligamentum flavum. When combined, these changes can result in acquired lumbar canal stenosis. Disc herniation is more common in patients younger than 50 years while degenerative and spondylotic changes are more common in patients older than 50 years.
Table C2-1 Causes of Lumbosacral Radiculopathy
Table C2-2 lists common findings in patients with the various lumbosacral radiculopathy. Straight leg raise test is a maneuver that causes stretching of the sciatic nerve, sacral plexus, and the L5 and S1 nerve roots. While the patient is supine, the pain is reproduced with passive straight leg raising or when the examiner flexes the leg at the hip and then extends it at the knee. The test is most reliable when it is positive between 30° and 70°. Reverse straight leg raise testing is performed by passive hip extension while the patient is prone and causes stretching of the femoral nerve, the lumbar plexus, and upper lumbar roots (L2, L3, or L4). Pain in the groin or anterior thigh is considered a positive test.
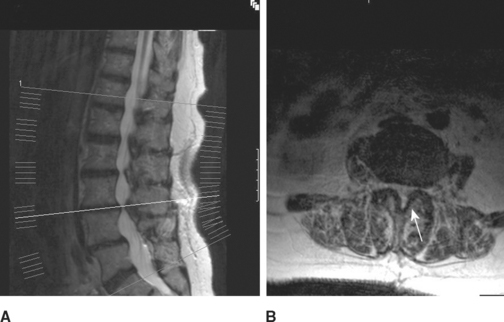
Lumbosacral root compression may involve a single root (monoradiculopathy) or multiple roots that are contiguous and may be bilateral (polyradiculopathy). Cauda equina lesions should be considered when more than two contiguous nerve roots are involved. Midline cauda equina syndrome results in early compression of sacral nerve roots, which lie medially within the cauda equina, leading to low back pain, sphincteric and sexual dysfunction, and paresthesias and sensory loss in sacral dermatomes (“saddle anesthesia”). When the lesion is large (such as with large midline L4–5 disc herniation), lumbosacral nerve roots may be involved resulting in leg weakness and sensory loss that may develop either early or later in the course, and sometimes result in paraplegia when multiple bilateral nerve roots are involved. Another clinically distinct cauda equina syndrome is the one caused by lumbar canal stenosis (Figure C2-4). This often presents with intermittent neurogenic claudication which is characterized by low back and leg pain, sometimes with paresthesias and weakness, brought on by standing and often worsened by walking. Typically, the symptoms are completely relieved several minutes after the patient sits down and are occasionally improved by bending at the waist. The symptoms are often bilateral but may be unilateral. The neurological examination in patients with lumbar canal stenosis may be entirely normal or show evidence of a single lumbosacral monoradiculopathy or patchy lumbosacral polyradiculopathy often involving the L4, L5, or S1 roots.
Electrodiagnosis
General Concepts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree