Case 18
HISTORY AND PHYSICAL EXAMINATION
Electrodiagnostic (EDX) study was performed.
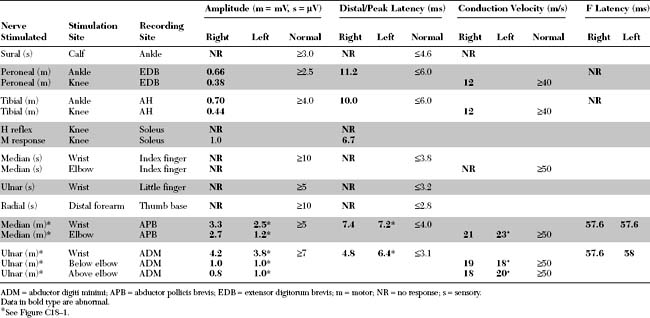
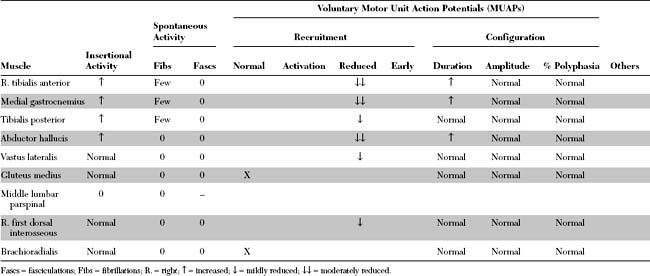
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
The abnormal EDX findings in this case include:
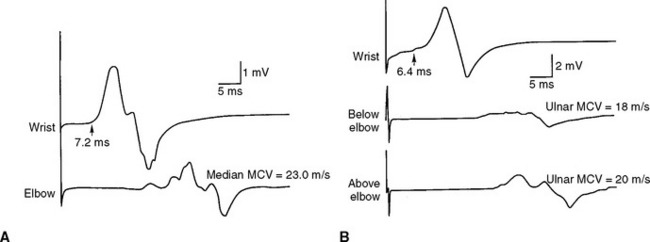
Figure C18-1 Motor nerve conduction studies of the left median nerve, recording abductor pollicis brevis (A) and the left ulnar nerve, recording abductor digiti minimi (B). Note the conduction blocks and dispersion between distal and proximal stimulations and the marked slowing of velocities and distal latencies. (See also the Nerve Conduction Studies table.)
DISCUSSION
Clinical Features
Peripheral Polyneuropathies
Peripheral polyneuropathy is a common presenting illness in neurologic practice with multiple, sometimes overwhelming, list of potential etiologies. Pattern recognition is a useful diagnostic approach but applies to a minority of patients who usually have advanced disease and often requires vast clinical experience such as by a seasoned neurologist. For an example, an asymmetrical polyneuropathy with predilection to cool skin areas (nipples, buttocks, and fingers) and skin ulcerations is highly suggestive of leprous neuropathy. Also, a distal sensory polyneuropathy with brisk reflexes, mild cognitive impairment, and a red tongue suggests combined system degeneration due to vitamin B12 deficiency. Another approach to the etiologic diagnosis of peripheral polyneuropathy is to order all available tests, including costly serology evaluations, on every patient with a polyneuropathy. Unfortunately, this irrational “shotgun” approach is quite common and often utilized by internists and some neurologists. It sometimes results in an incorrect diagnosis secondary to incidental abnormalities such as an elevated glucose on glucose tolerance test or antineuronal antiboby on serological testing.
A recommended and more rational approach may be initiated on every patient presenting with a peripheral polyneuropathy. This could be achieved by performing a thorough history and physical examination followed by EDX studies (see Figure C26–1, Case 26), and often results in limited and cost effective investigations (Table C18-1). Despite extensive investigations in specialized centers that includes EDX testing, antibody panels and genetic testing, up to 20% of patients with peripheral polyneuropathies will not have their exact causation identified. Of those with idiopathic etiology, it is estimated that a familial neuropathy accounts for about 40% if a meticulous family history is taken and relatives are carefully examined.
Table C18-1 Essential Facts Important in the Classification and Etiologic Diagnosis of Peripheral Polyneuropathy
CIDP = chronic inflammatory demyelinating polyradiculoneuropathy, HNPP = hereditary neuropathy with liability to pressure palsy, CMT = Chercot-Marie-Tooth disease, HIV = human immunodeficiency virus.
Chronic Demyelinating Polyneuropathies
In most peripheral polyneuropathies, it is often possible to define the predominant pathophysiologic mechanism, based on electrophysiologic and pathologic features, as being either primarily axonal or demyelinating. In demyelinating polyneuropathy, it is also useful to distinguish between neuropathies with segmental (multifocal) versus uniform slowing, based on electrophysiologic studies (see electrodiagnosis). Multifocal or segmental demyelinating polyneuropathies are almost always acquired, while uniform demyelinating polyneuropathies are typically hereditary.
The causes of chronic axonal neuropathies are abundant, while chronic demyelinating polyneuropathies have a fairly restrictive differential diagnosis (Table C18-2). Many acquired demyelinating polyneuropathies are immune in nature and respond to immunosupression or immunomodulation, while most axonal polyneuropathies are metabolic or toxic in nature. Since the differential diagnosis of chronic acquired demyelinating polyneuropathies is quite limited, the diagnostic work-up for patients with such entities is much less laborious and is quite different from that of patients with axonal neuropathies (Table C18-3).
Table C18-2 Common Causes of Chronic Demyelinating Peripheral Polyneuropathy
| Acquired (nonuniform multifocal slowing) |
| Hereditary (uniform slowing) |
CIDP = chronic inflammatory demyelinating polyradiculoneuropathy; HIV = human immunodeficiency virus; GM1 = ganglioside M1; MAG = myelin-associated glycoprotein; MGUS = monoclonal gammopathy of unknown significance; Ig = immunoglobulin; POEMS syndrome = polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, and skin changes; HMSN = hereditary motor and sensory neuropathy; CMT = Charcot-Marie-Tooth disease; HNPP = hereditary neuropathy with liability to pressure palsy.
* May have multifocal slowing also, usually across common entrapment sites.
Table C18-3 Recommended Work-Up of Chronic Acquired Demyelinating Peripheral Polyneuropathy
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|