Case 16
HISTORY AND PHYSICAL EXAMINATION
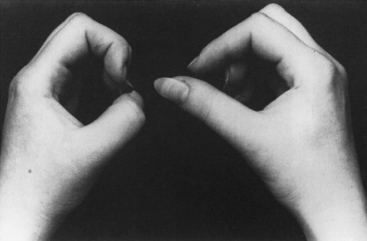
When the patient was seen 4 weeks after the onset of symptoms, he had minimal shoulder pain. Cranial nerve examination was normal. There was no Horner sign. Findings were limited to the right upper extremity, where there was complete loss of function of the right deltoid, spinati, biceps, and brachioradialis (Medical Research Council [MRC] 0/5). The right triceps was much less involved (4/5). There was mild diffuse weakness of all finger and wrist extensors, with severe weakness of the right thumb long flexion (flexor pollicis longus) and distal interphalangeal flexion of the index and middle fingers (flexor digitorum profundus). This resulted in a positive pincer or OK sign (Figure C16-1). Deep tendon reflexes of the right upper limb were absent. Sensation revealed mild sensory loss over the thumb, and lateral arm and forearm.
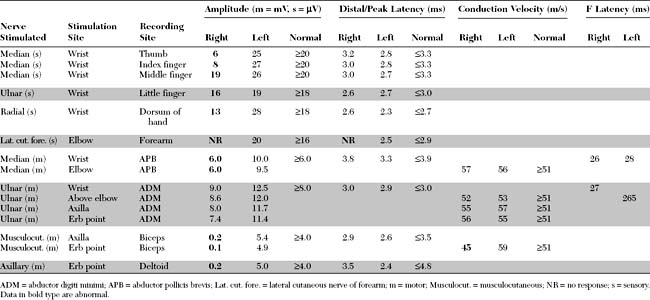
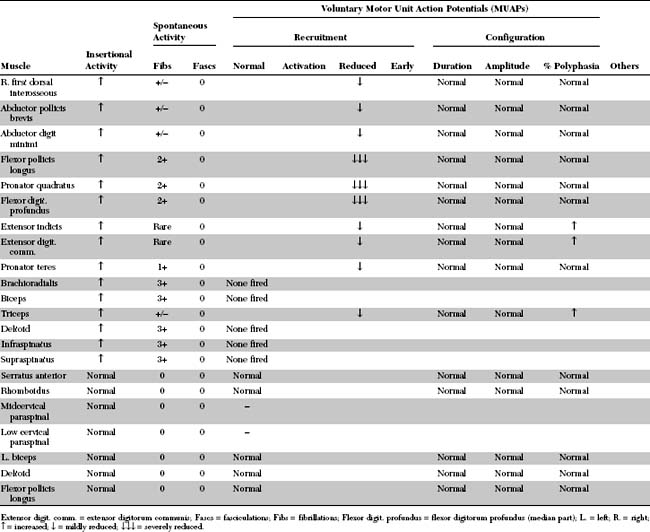
An electrodiagnostic (EDX) study was performed.
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Abnormalities on EDX examination include:
DISCUSSION
Clinical Features
Neuralgic amyotrophy is likely an immune-mediated disorder that affects peripheral nerves of the upper limb and is not restricted to elements of the brachial plexus. Unfortunately, the disorder is known by several misleading names that result sometimes in misdiagnosis (Table C16-1). Neuralgic amyotrophy has an estimated annual incidence of 1.64 cases per 100 000 population. It most often affects adults, peaking during their twenties. Males are affected twice as often as females. It is usually unilateral, but is sometimes bilateral and asymmetrical; it is occasionally recurrent. Most cases have no specific precipitating factors, but some appear few hours to weeks of an upper respiratory tract infection, a vaccination, childbirth, or an invasive diagnostic, therapeutic or surgical procedure.
Table C16-1 Terms Commonly Used to Describe the Syndrome of Neuralgic Amyotrophy (Listed Alphabetically)
As the most popular name implies, neuralgic amyotrophy is characterized by pain and weakness of the upper limb. The pain is usually abrupt in onset with a tendency to develop at night, sometimes awakening the patient from sleep. It is a severe deep boring shoulder pain, and maximal during the first few days of illness. The pain is not exacerbated by the Valsalva maneuver (e.g., cough, sneeze) which helps distinguishing it from a subacute cervical radiculopathy. Many patients visit the emergency department for pain control. In atypical cases, the pain is only modest and maximal over the antecubital fossa. The pain usually lasts for 7–10 days, gradually fades and becomes replaced by a dull ache.
Typically, the patient notices upper limb weakness, and sometimes wasting become apparent, during the first week as the pain starts to subside. Weakness of the shoulder girdle muscles, with or without scapular winging, is the most common since the upper plexus-innervated muscles are usually the most affected. The weakness is often restricted to multiple individual peripheral nerves and sometimes to a single nerve only (Table C16-2). Occasionally, the disorder afflicts the entire brachial plexus or exclusively the lower plexus leading to a near complete monoplegia or distal upper extremity weakness, respectively. Oddly, the main upper limb nerves, i.e., the median, ulnar, and radial nerves, are seldom exclusively affected. Occasionally, selective muscles are selectively denervated, presumably due to pathology of the motor branches. This includes the pronator teres, flexor pollicis longus and supraspinatus muscles (Figure C16-2). Sensory loss usually is mild but may be prominent in severe cases. Deep tendon reflexes are depressed or absent if the appropriate muscles are weakened significantly. Chest radiographs may reveal an elevated hemidiaphragm on the ipsilateral side, due to phrenic nerve palsy. Routine magnetic resonance imaging studies of the brachial plexus or upper limb usually are normal, apart from T2-weighted changes of denervated muscles. The diagnosis frequently is based on the clinical picture and is supported by EDX confirmation.
Table C16-2 Peripheral Nerves With High Predilection to Insult During Neuralgic Amyotrophy (Listed in Order of Frequency of Occurrence)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|