Case 15
HISTORY AND PHYSICAL EXAMINATION
An electrodiagnostic (EDX) examination was performed.
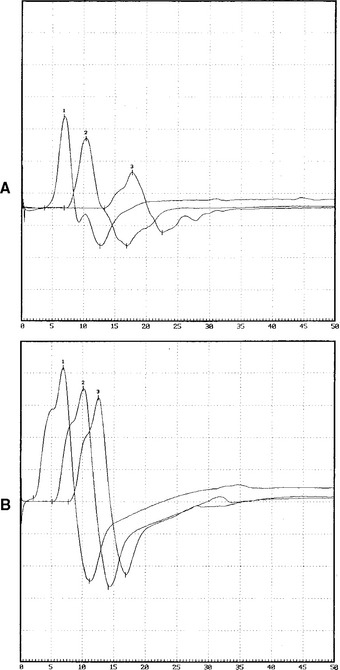
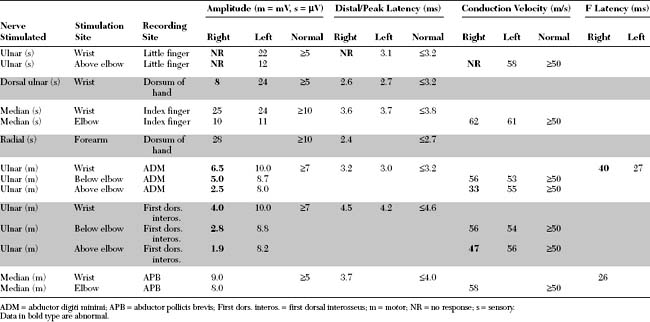
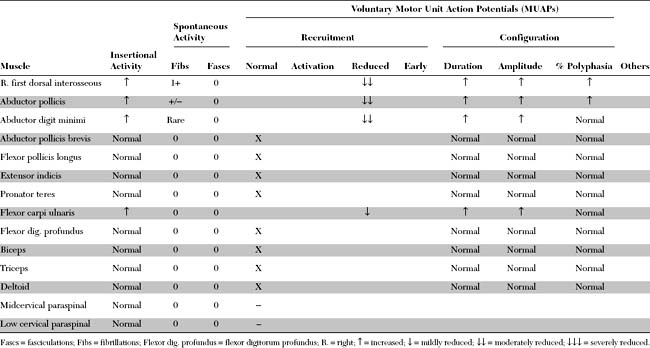
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
The EDX findings in this patient include:
DISCUSSION
Applied Anatomy
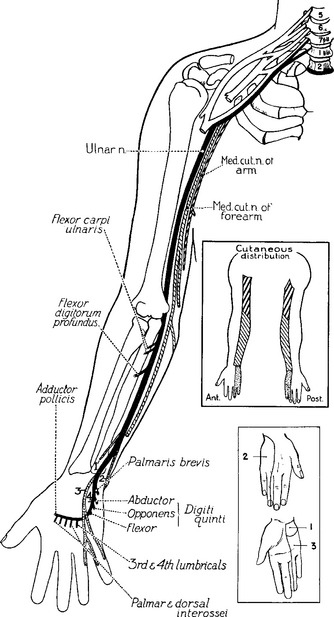
The ulnar nerve sensory and motor fibers are derived from the spinal nerves C8 and T1. Before arising from the plexus in the proximal axilla, the ulnar nerve fibers pass through the lower trunk and the medial cord of the brachial plexus (Figure C15-2). In the axilla and proximal arm, the ulnar nerve is closely related to the radial and median nerves and the brachial artery. Around the midarm, the ulnar nerve pierces the intermuscular septum and lies in close contact with the medial head of the triceps and humerus. The ulnar nerve develops no branches in the arm.
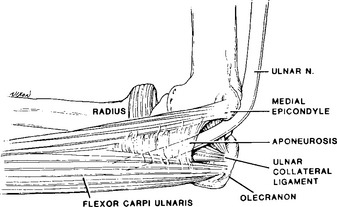
At the elbow level, and in contrast to most major human peripheral nerves, the ulnar nerve traverses the extensor, rather than the flexor, surface of the elbow joint. This renders the nerve more vulnerable to trauma around the elbow. At the elbow, the ulnar nerve crosses the ulnar groove (also called the condylar or retroepicondylar groove) behind the medial epicondyle and then passes the aponeurotic arch of the FCU to enter the cubital tunnel (Figure C15-3). This tunnel, also called the humeroulnar arcade, Osborne ligament, or arcuate arcade, is formed by the attachment of the muscle to the olecranon and medial epicondyle. Its proximal edge is variable but usually is approximately 1 cm distal to an imaginary line drawn between these two insertional points. With flexion of the elbow, the distance between the olecranon and medial epicondyle increases by approximately 1 cm, which results in tightening of the FCU aponeurosis over the nerve. In addition, the medial elbow ligament bulges, flattening the concave surface of the ulnar groove.
In the forearm, the ulnar nerve gives off its first branches. These are the motor branches to the FCU and FDP. These branches arise approximately 10 cm distal to the medial epicondyle. The ulnar nerve continues in the forearm deep to the FCU but superficial to the FDP to become superficial in the distal forearm, lying between the tendons of these two muscles. Two cutaneous sensory branches arise in the forearm, without passing through Guyon canal at the wrist, to innervate the skin in the hand. The first is the palmar ulnar cutaneous branch, which takes off at midforearm and innervates the proximal part of the ulnar border of the palm. The second is the dorsal ulnar cutaneous branch, which arises 6 to 8 cm proximal to the ulnar styloid, winds around the ulna, and innervates the dorsal surfaces of the little finger and half of the ring finger, along with the ulnar side of the dorsum of the hand (Figure C15-4).
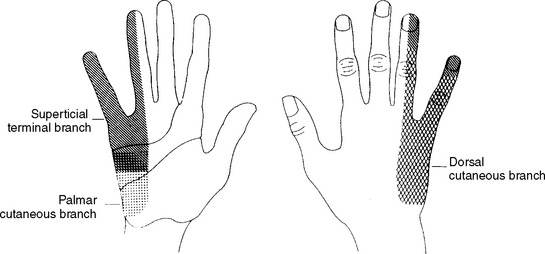
Figure C15-4 The cutaneous distribution of the three sensory branches of the ulnar nerve.
(From Stewart JD. The variable clinical manifestations of ulnar neuropathies at the elbow. J Neurol Neurosurg Psychiatry 1987;50:252–258, BMJ Publishing Group.)
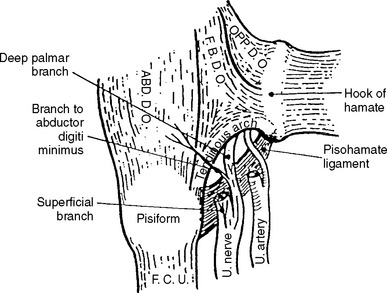
At the wrist, the ulnar nerve enters the distal ulnar tunnel (Guyon canal), where it divides into superficial (primarily sensory) and deep palmar (pure motor) branches (Figure C15-5). The superficial branch innervates the palmaris brevis muscle and the palmar aspects of digit V and half of digit IV. The deep branch innervates the hypothenar muscles, including the ADM, and travels through the palm to the dorsal and palmar interossei, the third and fourth lumbricals, the adductor pollicis, and a portion of the flexor pollicis brevis.
Figure C15-5 Anatomy of the ulnar nerve within Guyon canal at the wrist. 1 = ulnar artery, 2 = superficial branch of the ulnar nerve, 3 = hamulus, 4 = fibrous arch of the hypothenar muscles (see also Figure C15-2), 5 = pisiform, 6 = transverse carpal ligament, 7 = palmaris brevis, 8 = palmar carpal ligament.
(From Gross MS, Gelberman RH. The anatomy of the distal ulnar tunnel. Clin Orthop 1985;196:238–247, with permission.)
The flexor brevis digiti minimi (or quinti), a hypothenar muscle, has two separate attachments, at the hook of the hamate and at the pisiform bone. These musculotendinous attachments form a fibrous arch and create the superficial boundary of the pisohamate hiatus (PHH), an opening through which the deep motor branch of the ulnar nerve passes. The posterior boundary of the PHH, the pisohamate ligament, extends from the pisiform bone to the hook of the hamate (Figure C15-6). The origin of the major motor branch to the ADM is proximal to this hiatus in the majority of hands.
Clinical Features
Ulnar mononeuropathy across the elbow is a common entrapment neuropathy. It is second only to carpal tunnel syndrome in the incidence of entrapment neuropathy in general. Ulnar neuropathies across the elbow are usually caused by compression, although isolated ulnar mononeuropathy resulting from nerve infarction (such as in vasculitic neuropathy) or associated with leprosy, may occur infrequently. Causes of compressive ulnar lesions across the elbow are shown in Table C15-1. Compression of the ulnar nerve in the elbow region occurs frequently at one of the two following sites: the ulnar (condylar) groove or cubital tunnel (humeroulnar (arcuate) aponeurotic arcade). In some patients with unequivocally ulnar nerve lesions around the elbow, it is difficult to identify the exact cause, even during surgery. Most surgeons presume that the lesion is within the cubital tunnel and treat it as such.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree