Case 14
HISTORY AND PHYSICAL EXAMINATION
Electrodiagnostic (EDX) examination was performed.
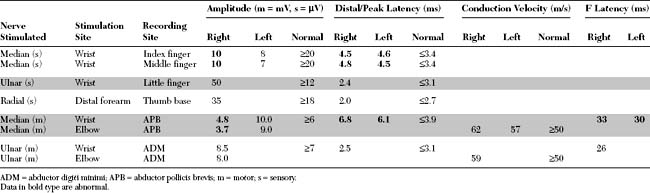
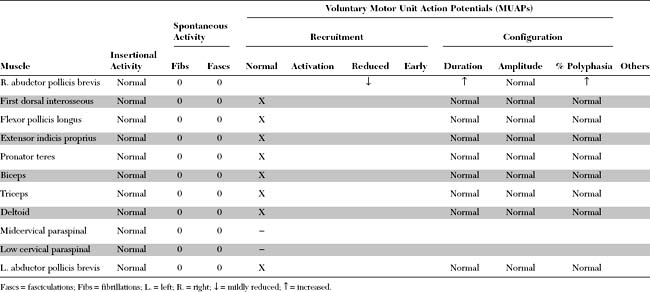
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Relevant EDX findings in this patient include:
DISCUSSION
Applied Anatomy
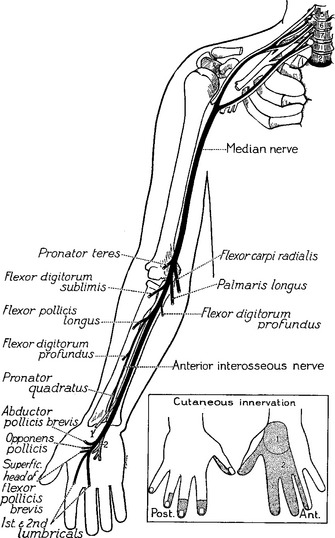
The median nerve is one of the main terminal nerves of the brachial plexus, formed by contributions from the lateral and medial cords (Figure C14-1). The lateral cord component, comprised of C6–C7 fibers, provides sensory fibers to the thumb and thenar eminence (C6), index finger (C6–C7), and middle finger (C7) and motor fibers to the proximal median innervated forearm muscles. The medial cord component, comprised of C8–T1 fibers, provides sensory fibers to the lateral half of the ring finger (C8) and motor fibers to the hand and distal median innervated forearm muscles.
Right before entering the wrist, the median nerve gives off its first cutaneous branch, the palmar cutaneous branch, which runs subcutaneously (does not pass through the carpal tunnel) and innervates a small patch of skin over the base of the thumb and the thenar eminence (see Figure C14-1). Then, the main trunk of the median nerve, along with nine finger flexor tendons, enters the wrist through the carpal tunnel. The carpal bones form the floor and sides of the tunnel while the carpal transverse ligament, which is attached to the scaphoid, trapezoid, and hamate bones, forms its roof (Figure C14-2). The carpal tunnel cross-section is variable but is approximately 2.0 to 2.5 cm at its narrowest point in most individuals.
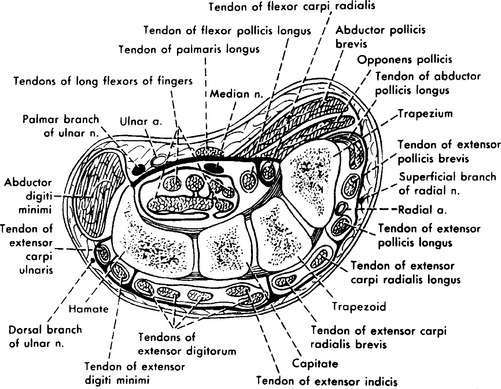
Figure C14-2 A cross-section of the wrist revealing the carpal tunnel and its contents.
(From Hollinshead WH. Anatomy for surgeons: the back and limbs, 3rd ed., vol 3. Philadelphia, PA: Harper and Row, 1982, with permission.)
Clinical Features
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy. It is slightly more common in women and usually involves the dominant hand first. It is most prevalent after 50 years of age, but it may occur in younger patients, especially in association with pregnancy and certain occupations or medical conditions. Most cases of CTS are idiopathic, but many are associated with disorders that decrease the carpal tunnel space or increase the susceptibility of the nerve to pressure. Among the medical conditions with a high risk for CTS are pregnancy, diabetes mellitus, hypothyroidism, acromegaly, rheumatoid arthritis, sarcoidosis, and amyloidosis. Some patients have congenitally small carpal tunnels, while others have anomalous muscles, wrist fractures (Colles or carpal bone), or space occupying lesions (ganglia, lipoma, schwannoma). Occupational CTS, which has reached a near-epidemic level in the industrial world, is seen in patients whose jobs involve repetitive movements of the wrists and fingers. Although most cases of CTS are subacute or chronic in nature, it occasionally may be acute, such as after crush injury of the hand, fracture (Colles or carpal bone), or acute tenosynovitis.
The differential diagnoses of CTS include: