Case 11
HISTORY AND PHYSICAL EXAMINATION
An electromyography (EMG) examination was then performed.
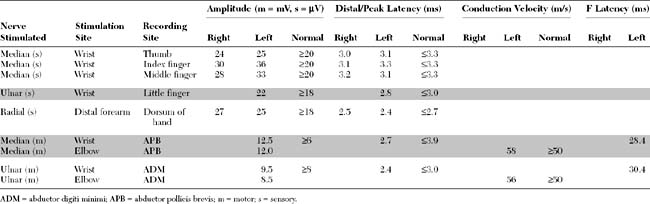
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Pertinent electrodiagnostic (EDX) findings in this case include:
DISCUSSION
Applied Anatomy
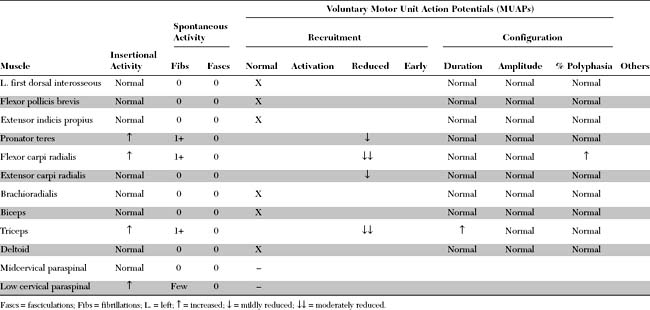
The dorsal root axons originate from the sensory neurons of the DRG, which lie outside the spinal canal, within the intervertebral foramen, immediately before the junction of the dorsal and ventral roots (Figure C11-1). These sensory neurons are unique because they are unipolar. They have proximal projections through the dorsal root, called the preganglionic sensory fibers, to the dorsal horn and column of the spinal cord. The distal projections of these neurons, called the postganglionic peripheral sensory fibers, pass through the spinal nerve to their respective sensory end-organs. The ventral root axons, however, are mainly motor (some are sympathetic, with origins from the anterolateral horn of the cord). The motor axons originate from the anterior horn cells within the spinal cord. Passing through the spinal nerves and the peripheral nerve, these motor fibers terminate in the corresponding muscles.
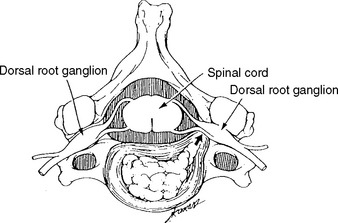
In humans, there are 31 pairs of spinal nerve roots: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal. In the cervical spine, each cervical root exits above the corresponding vertebra that shares the same numeric designation (Figure C11-2). For example, the C5 root exits above the C5 vertebra (i.e., between the C4 and C5 vertebrae). Because there are seven cervical vertebrae but eight cervical roots, the C8 root exits between the C7 and T1 vertebrae; subsequently, all thoracic, lumbar, and sacral roots exit below their corresponding vertebrae. For example, the L3 root exits below the L3 vertebra (i.e., between the L3 and L4 vertebrae).
Clinical Features
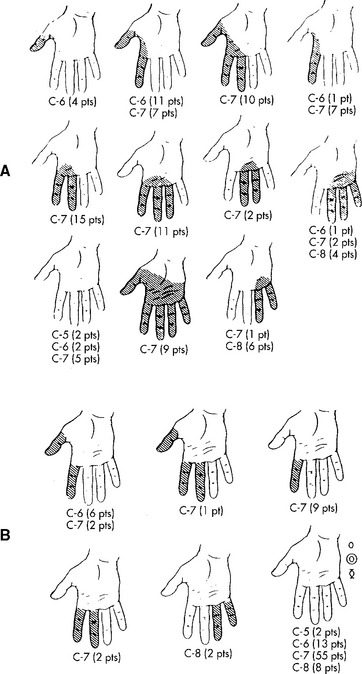
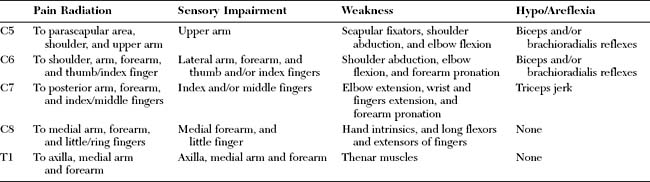
The classic study by Yoss et al., published in 1957, remains the best available clinicoanatomic study of cervical root compression. This detailed study analyzed the symptoms and signs of 100 patients with surgically proven single cervical lesions. C7 radiculopathy was the most common cervical radiculopathy, accounting for almost two thirds of patients (Figure C11-3). Figure C11-4 shows the common sensory symptoms and signs observed in these patients, while Figure C11-5 shows the weakened muscles caused by cervical radiculopathy. This study revealed the extreme variability of sensory manifestations in patients with cervical radiculopathy. Also, no single muscle was exclusively diagnostic of a specific root compression. However, based on the data, certain clinical conclusions can be made:
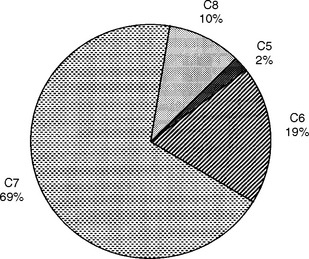
Figure C11-3 Incidence of cervical root involvement in a series of 100 patients with surgically proven single-level lesions.
(Data adapted from Yoss RE et al. Significance of symptoms and signs in localization of involved root in cervical disc protrusion. Neurology 1957;7:673–683, with permission.)

Figure C11-5 Incidence and severity of weakness of muscles or groups of muscles in cervical radiculopathy (C5–C8).
(From Yoss RE et al. Significance of symptoms and signs in localization of involved root in cervical disc protrusion. Neurology 1957;7:673–683, with permission.)
However, despite the variability in sensory and motor presentations of cervical radiculopathies, certain classical symptoms and signs exist and are extremely helpful in localizing the compressed root. Table C11-1 reveals the common presentations of cervical radiculopathies.
Electrodiagnosis
General Concepts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree