Carotid Bypass
W. John Byrne
Nishan Dadian
There are two forms of carotid–carotid bypass: ipsilateral common carotid to internal carotid artery (ICA) interposition bypass and common carotid to common carotid crossover bypass. They are infrequently performed but the requisite skills are well within the province of any experienced vascular surgeon. In truth, neither type of bypass has ever been commonly indicated but many patients who previously may have been candidates (e.g., patients with symptomatic innominate artery occlusions or irradiated carotid bifurcations) now have stents placed.
Ipsilateral common carotid to ICA bypass graft, in our practice, is often a “bail-out” or emergent procedure in difficult elective “atherosclerotic” cases or when complications arise. Less commonly it is a planned elective procedure.
We favor the eversion technique for all patients undergoing elective carotid endarterectomy (CEA). In this, the ICA is divided from its origin and its wall is peeled off the plaque. The common carotid artery (CCA) and proximal external carotid artery (ECA) are next cleared of atheroma and finally the ICA is reanastomosed to its origin. As with conventional endarterectomy, the surgeon must identify a good “end-point” where the plaque ends and the intima becomes normal. This is readily accomplished in most patients but rarely (less than 1% of operations), the plaque is continuous with the intima and a clear end-point cannot be demarcated. In this instance, we transect the internal carotid distally and perform an interposition graft from the endarterectomized CCA to the distal ICA in an end-to-end fashion, usually using a 6-mm-diameter prosthetic graft. Such difficulties can also be encountered during “conventional” CEA when an unsatisfactory end-point is identified. In both “conventional” and eversion techniques, iatrogenic injuries may occur such as perforation or excessive thinning of the ICA wall. Some centers perform routine completion angiograms after CEA and large intimal flaps will mandate bypass.
When patients sustain an immediate postoperative arterial thrombosis following elective CEA, we reexplore them emergently. If the ICA is thrombosed, we excise all endarterectomized ICA due to its assumed thrombogenicity and replace it with a prosthetic or vein graft.
Carotid wall infection is rare, especially when using the eversion technique which eschews use of prosthetic material, but not unknown. It usually arises from an infected hematoma and presents as a pseudoaneurysm or secondary hemorrhage. In conventional CEA, where patching is standard of care, an infected prosthetic patch is the cause. In
both instances, a vein graft is used following excision of all grossly infected native artery. The final, rare emergent indication is penetrating trauma.
both instances, a vein graft is used following excision of all grossly infected native artery. The final, rare emergent indication is penetrating trauma.
The commonest nonemergent indication is carotid artery restenosis following CEA. Although surgery (either redo CEA or bypass) has been supplanted by stenting, it still has a role in some patients—and, of course, in the management of in-stent restenosis (see Fig. 5.1). The second indication for bypass is patients with radiation arteritis. Atherosclerotic carotid artery aneurysms and extensive carotid body tumors (Shamblin types II and III) are the final elective indications.
Common carotid to common carotid crossover bypass was previously indicated for patients with occlusive proximal common carotid disease not amenable to subclavian-carotid bypass and not fit enough for or desirous of an ascending aorta to carotid bypass. The majority of these patients in most series (including our own) had symptomatic CCA stenoses. On rare occasion, it was performed for asymptomatic stenoses. Many of these open surgical operations have been supplanted by endovascular procedures. Ironically, endovascular therapy has generated a new indication for this operation. Stenting is now the treatment of choice for thoracic aortic aneurysms. Aortic arch “debranching,” by increasing the proximal “landing zone” for stent grafts allows more patients access to thoracic endovascular aneurysm repair (TEVAR). Debranching requires at least left common carotid to left subclavian artery bypass, but, on occasion, right CCA to left common carotid bypass as well. This permits the stent graft to lie across the origins of the left subclavian and left common carotid arteries. The last indications for carotid crossover bypass are giant cell arteritis and Takayasu’s arteritis affecting the proximal supra-aortic trunks and proximal innominate artery atherosclerosis causing severe right arm ischemia.
Contraindications
The principal contraindication to either form of carotid bypass is the patient’s general medical condition. In emergent or “bail-out” procedures, there is little option but to
proceed. In patients with severe asymptomatic primary atherosclerotic carotid artery stenosis or recurrent carotid artery stenosis the more prudent decision may be to optimize medical therapy rather than intervention if the patient has severe comorbidities or limited life expectancy.
proceed. In patients with severe asymptomatic primary atherosclerotic carotid artery stenosis or recurrent carotid artery stenosis the more prudent decision may be to optimize medical therapy rather than intervention if the patient has severe comorbidities or limited life expectancy.
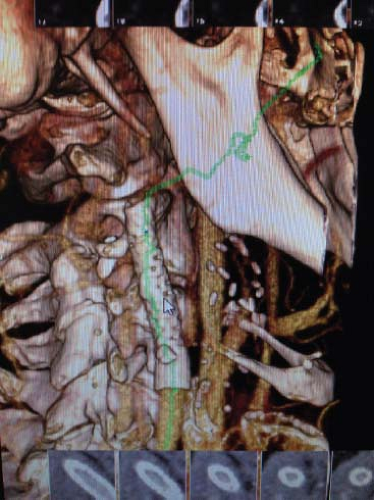
For patients undergoing either carotid bypass, assessment of benefit is key. This starts with a comprehensive history and physical examination. Cardiology evaluation is a prerequisite in most centers in the United States. In our center, at least, routine otorhinolaryngologic consultation is not obtained, even in patients who have already had contralateral carotid surgery. For all patients with suspected carotid disease, Duplex scanning is used to evaluate the extracranial carotid, subclavian, and vertebral arteries. It is rapid, noninvasive and highly sensitive and specific when performed by an experienced vascular technologist. The main limitation of carotid Duplex, however, is an inability to visualize the intrathoracic or intracranial vessels. We, therefore, often supplement Duplex with computerized tomographic angiography (CTA) to obtain a fuller picture of these arteries (see Fig. 5.1). Magnetic resonance angiography (MRA) still is used but its longer imaging times relative to CTA and lack of applicability in patients with impaired renal function has reduced its role. Catheter angiograms are reserved for those patients where there is a discrepancy between CTA and Duplex. It is more invasive than either, but is still regarded as the “gold standard” for evaluation the aortic arch and supra-aortic trunks. Given the potentially devastating consequences of carotid artery surgery, careful counseling of all patients is essential. The risk of minor and major stroke as well as the repercussions of cranial nerve damage must be explained to the patient and documented. In patients for whom vein will be needed for bypass, Duplex vein mapping and marking of the legs is performed.
On the morning of surgery, all patients have a complete blood count, basic metabolic panel and are typed and screened. They receive a prophylactic dose of intravenous antibiotics within 1 hour of skin incision, usually a first-generation cephalosporin such as cefazolin in patients who are not allergic to beta-lactams. For allergic patients, we use a weight-based dose of vancomycin. We do not routinely stop any antiplatelet agents but will stop warfarin or the newer oral antithrombin agents.
Positioning and Choice of Anesthesia
For ipsilateral bypass we usually use superficial and/or deep cervical plexus block with intravenous sedation. We reserve general anesthesia with endotracheal intubation for ipsilateral bypass patients in whom vein harvest is required or who need crossover bypass. All patients must have adequate intravenous access, pulse oximetry, and an arterial line inserted for blood pressure monitoring. On occasion, when it has not been possible to place a reliable arterial line, we will use a sphygmomanometer alone for arterial blood pressure monitoring.
Position and patient comfort is especially important when procedures are performed under regional anesthesia. A restless patient will make the surgery difficult if not impossible. For ipsilateral common carotid to internal carotid bypass, the patient is placed in the supine position with their head supported by a gel head ring or doughnut. The neck is hyperextended and the head is rotated 15 to 20 degrees away from the surgeon. This moves the mandible superiorly and facilitates access to the carotid arteries. A note of caution, avoid the temptation to rotate the neck further than this as it can lead to the plane of dissection being developed too medially as the operation progresses.
Excessive extension will also be counterproductive. The sternocleidomastoid muscle will become taut and internal jugular vein will rotate anteriorly to the carotid arteries rather than remaining in a lateral position. It is also an unpleasant position for the awake patient. We support the shoulders with rolled towels and attach adhesive tape from each side of the table to the other, across the patient’s forehead to maintain head position. We also find it useful to place the patient in a 15- to 20-degree “head up” or reversed Trendelenburg position for two reasons: patient comfort, especially when performing procedures under regional anesthesia and to decrease venous pressure and congestion and so lessen bleeding. We prepare the skin with a chlorhexidine solution, square off the surgical site, and use and an antimicrobial adhesive drape to secure the drapes. We always ensure that the sternoclavicular joint and the ear lobe are exposed. If it is anticipated that leg vein harvest will be required, the leg is prepared also.
For common carotid to common carotid crossover bypass, the positioning is the same with the neck extended as described and rotated as needed for each carotid exposure.
Technique
Ipsilateral Common Carotid to Internal Carotid Artery Bypass
Ipsilateral common carotid to ICA bypass requires surgical exposure of the carotid vessels no different to that for CEA. Initially, a 3- to 4-cm incision is made anterior to the sternocleidomastoid midway between the mastoid and the sternoclavicular joint; the platysma is divided with electrocautery and the external jugular vein is ligated and divided. The superficial cervical fascia is divided and the sternocleidomastoid muscle is retracted posteriorly. The anterior facial vein (which can be single or multiple) arises from the anterior surface of the internal jugular vein. It is ligated and divided. Often lymph nodes are encountered at this stage and they should be freed up medially and retracted laterally to facilitate exposure of the carotid arteries.
We usually dissect the CCA first. The vagus nerve lies directly posterior or posterolateral to the CCA and is usually readily separated from the artery. Care must be taken when applying a clamp on the CCA not to inadvertently crush the vagus nerve which will result in vocal cord paralysis (see Fig. 5.2). The superior laryngeal nerve branch of the vagus passes posterior to and just above the carotid bifurcation and may be at risk during dissection in this area. The recurrent laryngeal nerve, on the other hand, usually lies in the tracheoesophageal groove, protecting it from injury. A nonrecurrent inferior laryngeal nerve (NRILN) occurs on the left in 0.004% of patients. It occurs on the right in 0.6% of patients. Type 1 NRILNs arise directly from the vagus and run together with the vessels of the superior thyroid pedicle, and are therefore at risk when dissecting medially or posteriorly to the carotid bulb. Types 2A and 2B run with the inferior thyroid artery.
The ICA is medial and posterior to the ECA and deep the internal jugular vein. Usually it is located by continuing CCA exposure cephalad. However, distal exposure of the ICA must allow adequate space to clamp the artery and perform the distal anastomosis. This usually means mobilization of the hypoglossal nerve, which is tethered in place by the sternocleidomastoid branches of the occipital artery and vein. These are divided along with the descending hypoglossal branch of the ansa cervicalis to allow the nerve to be moved cephalad. We avoid placing slings on the nerve to reduce the risk of traction injury which results in dysarthria and dysphagia.
For even more distal exposure, the posterior belly of digastric muscle will also have to be divided. In this circumstance, the glossopharyngeal nerve is at risk and care must be taken to identify and preserve it as it runs along the superior border of the digastric in close proximity and superficial to the ICA. Isolated glossopharyngeal nerve palsy results in loss of ipsilateral gag reflex, taste in the posterior one-third of the tongue, a dry mouth from decreased salivation, and poor pharyngeal elevation with speaking and swallowing. However, as Naylor points out, most swallowing problems after carotid surgery are not due to damage to the glossopharyngeal nerve, which is largely a sensory
nerve only supplying motor fibers to the stylopharyngeus muscle, but from injury to motor fibers of the vagus nerve. These lie within a thin membrane bounded inferiorly by the hypoglossal nerve and superiorly by the glossopharyngeal nerve. He advises caution when incising these tissues to gain access to the upper reaches of the ICA because the vagal motor fibers may be inadvertently divided.
nerve only supplying motor fibers to the stylopharyngeus muscle, but from injury to motor fibers of the vagus nerve. These lie within a thin membrane bounded inferiorly by the hypoglossal nerve and superiorly by the glossopharyngeal nerve. He advises caution when incising these tissues to gain access to the upper reaches of the ICA because the vagal motor fibers may be inadvertently divided.
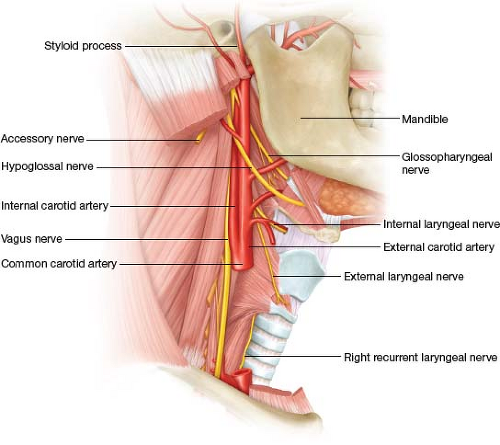 Figure 5.2 Anatomy of the carotid bifurcation displaying the cranial nerves at risk during carotid bypass. |
We have never had to divide the ramus of the mandible or subluxate it to complete these bypasses. Once distal exposure is satisfactory, one must fully dissect the carotid bifurcation and clear all carotid body fibers and connective tissue from around the ICA to free it up circumferentially. This allows for rapid proximal transection and distal division of the ICA. When performing this operation under cervical block (our usual practice), the patent will often experience some discomfort when the carotid sinus tissues are divided, so we commonly supplement the block in this area with 2 to 3 mL of 1% lidocaine.
The patient is heparinized with 3,000 units/kg 3 minutes prior to cross-clamping the vessels. The external and internal carotid arteries are clamped using Yasargil clips on to minimize risk of a clamp injury and an angled Cooley clamp is placed on the CCA. The ICA is transected from its origin and the distal ICA is also divided and the ICA excised. Assuming the patient is responding appropriately to verbal commands, no shunt is used. The graft is sewn end-to-end onto the distal ICA using a parachute technique with 6/0 polypropylene, taking care to incorporate all layers of the arterial wall (see Fig. 5.3). We favor a prosthetic graft in “clean” cases and use a 6 mm expanded polytetrafluoroethylene (ePTFE) graft. Long-term patency rates are excellent and while vein functions well, it has been associated with higher rates of early graft stenosis compared to ePTFE. Due to size discrepancy between the 6 mm ePTFE graft and the 4 to 5 mm ICA, it may be necessary to bevel the distal ICA to accommodate the graft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree