15 Carotid Artery Stenting
Diagnosis of Carotid Artery Disease: Anatomical Imaging
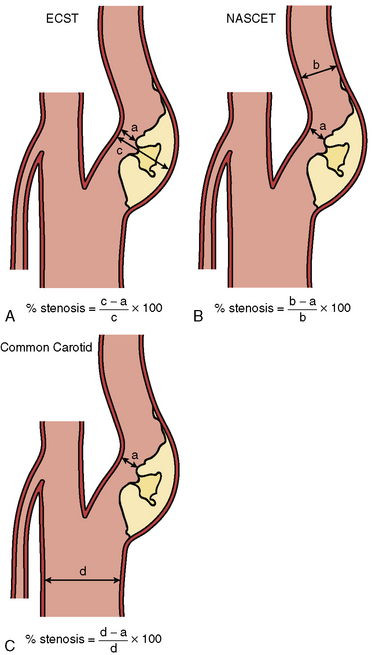
Digital subtraction angiography (DSA) is the gold standard for defining carotid anatomy with the NASCET method of stenosis measurement the most widely used (Fig. 15-1). Cerebral catheter-based angiography carries a risk of cerebral infarction of 0.5% to 1.2%; therefore, noninvasive imaging should be the initial strategy for evaluation.
Surgical Therapy
• Carotid artery stenosis after prior radical neck surgery
• High cervical carotid artery lesions that are surgically inaccessible
• Sequential lesions of the proximal to distal ICA
• Lesions of the common carotid artery and associated ICA lesions
• Recurrent stenosis of the carotid artery after CEA
• Non-atherosclerotic cause of carotid artery stenosis (e.g., fibromuscular dysplasia, Takayasu’s arteritis)
• Ipsilateral stenosis due to prior radiation therapy to the neck
• Increased operative risk due to concomitant illnesses such as CAD requiring coronary artery bypass surgery
• Contralateral occlusion and concurrent high-grade ipsilateral stenosis
Procedural Techniques
Baseline Aortography and Cerebral Angiography
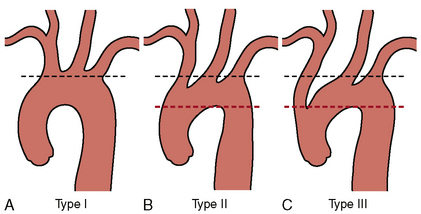
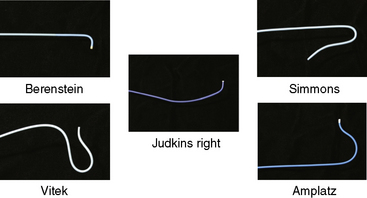
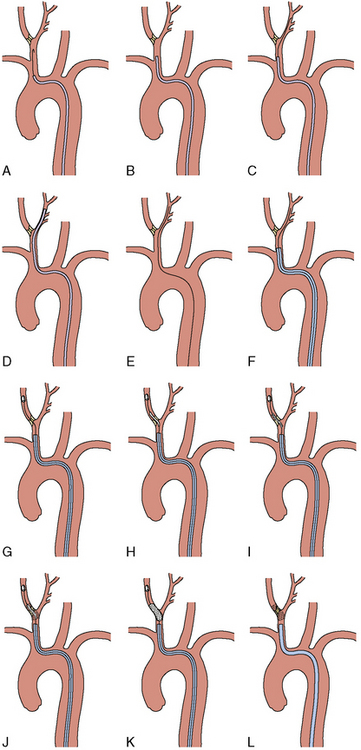
Once the morphology of the aortic arch is determined (Fig. 15-2), catheters are chosen for selective angiography of the cervical arteries supplying the brain (right and left carotid and vertebral arteries) and the cerebral vasculature. In a type I arch, Berenstein or Judkins right (JR) catheters are often used. In type II or III arch morphologies, shepherd’s crook–shaped catheters (i.e., Simmons or Vitek catheters) may be best (Fig. 15-3).
Internal Carotid Intervention
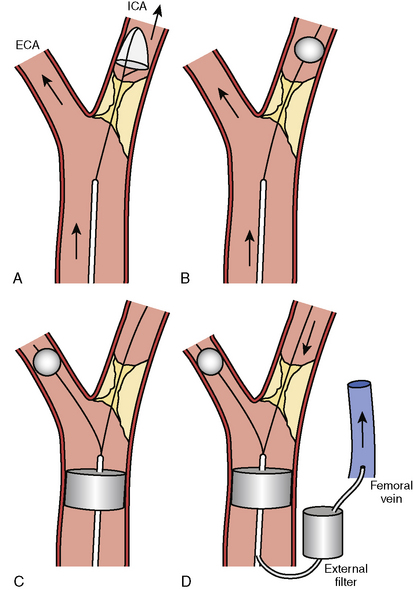
For procedures performed with a filter-type distal embolic protection device (EPD), the target lesion is crossed with the EPD. Although there are no randomized trials comparing stenting with EPDs to stenting alone, one study found that 57% of EPDs contained debris upon retrieval. EPDs are standard of care in the United States, and several types exist (Fig. 15-4). If the distal EPD will not cross the lesion, the stenosis may be crossed with a conventional 0.014-inch guidewire and subsequently predilated with a small (2.5 mm) balloon. Then the EPD should be placed. After distal EPD deployment, the lesion is often predilated with an undersized coronary balloon, typically 3 to 4 mm in diameter. A self-expanding stent is then placed across the lesion. The stent is sized to fit the CCA, and as a general rule, self-expanding stents are typically sized at least 1 mm larger than the reference diameter. There is no demonstrated benefit for using tapered stents. It is common practice, when treating an internal carotid bifurcation lesion, to place the stent across the ostium of the external carotid artery (Fig. 15-5).