ulceration leads to luminal thrombus apposition and distal embolization. Both in asymptomatic and in symptomatic patients, the more severe the carotid lesion, the higher the risk of subsequent stroke. The presence of ulcerated lesions, seen in up to one third of the endarterectomy specimen but underappreciated with angiography, also increases the risk of ischemic events. In the medical arm of the North American Symptomatic Carotid Endarterectomy Trial (NASCET), the 2-year stroke incidence among symptomatic patients with evidence of carotid ulcers on angiography ranged from 26.3 to 73.2% as the degree of stenosis increased from 75 to 95%.
conditions: carotids that bifurcate high, long (greater than 3 cm) ICA plaque, calcific shadows, or near-complete occlusions. In these cases, magnetic resonance imaging is of value in differentiating between the two.
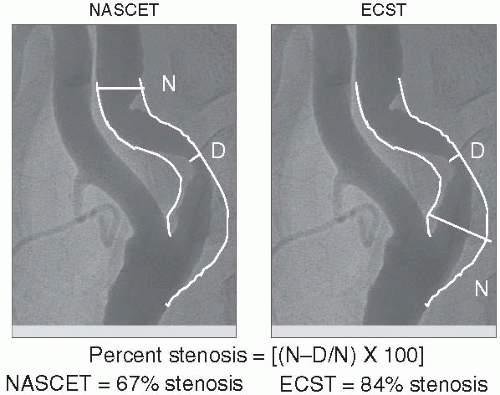
methods for calculating the degree of angiographic stenosis have been used in the major clinical trials (Fig. 11.1). Both the NASCET and the European Carotid Surgery Trial (ECST) define the stenotic segment the same way but differ in how they define the reference segment or the normal diameter. The NASCET method defines normal as the diameter just distal to the carotid bulb (neither the bulb itself nor a region of poststenotic dilatation), whereas the ECST method defines normal as the estimated diameter of the carotid bulb as it was prior to atherosclerotic narrowing. For any given stenosis, the ECST method gives a higher percentage diameter stenosis as illustrated in Figure 11.1. It is important to know which method was used to determine reference segment in order to interpret and apply trial results appropriately. Importantly, angiography remains the only scientifically validated method of defining ICA stenosis requiring endarterectomy, as in the large-scale randomized trials (i.e., NASCET, ECST) the degree of stenosis was assessed by angiography. However, in centers where MRA and duplex ultrasound imaging have been demonstrated to be concordant with angiography, angiography is usually not considered to be necessary in the clinical assessment of carotid disease prior to endarterectomy.
325 mg) was superior to high-dose ASA (650 to 1,300 mg) in preventing stroke, myocardial infarction (MI), or death both at 30 days (5.4 vs. 7.0%, P = 0.07) and at 3 months (6.2 vs. 8.4%, P = 0.03) in patients undergoing carotid endarterectomy. The Antiplatelet Trialists’ Collaboration analyzed the results of 195 trials of greater than 135,000 patients and found that platelet antagonists lowered the risk of stroke, MI, and vascular death. On the basis of this, individuals at risk for vascular events should receive antiplatelet agents for the primary prophylaxis of stroke.
TABLE 11.1 AGENTS EFFECTIVE IN VASCULAR RISK REDUCTION INCLUDING ONGOING CLINICAL TRIALS | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
surgery. The NASCET trial randomized patients with symptomatic 30 to 99% carotid artery stenosis to endarterectomy or medical management. Among 662 patients with 70 to 99% stenosis, at 2 years, those randomized to surgery had benefit in terms of ipsilateral stroke (9 vs. 26%; absolute risk reduction 17%; P < 0.001), any stroke (12.6 vs. 27.6%; P < 0.001), and major stroke or death (8.0 vs. 18.1%; P < 0.01). The perioperative (i.e., within 30 days) stroke or death rate in the trial was 5.8%. A total of 2,267 patients had stenosis less than 70% and were divided in post hoc analyses into groups with 50 to 69% stenosis and those with less than 50% stenosis. In patients with 50 to 69% stenosis, a 6.5% reduction in the
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree