Carotid Artery Disease
Hemal Gada
I. EPIDEMIOLOGY AND ETIOLOGY OF STROKE
A. Annually, there are nearly 800,000 strokes in the United States and 15 million strokes worldwide. Stroke is the third leading cause of death in Western societies and the leading cause of long-term disability in the United States.
B. Ischemic stroke accounts for approximately 85% of all strokes and can be classified into two broad categories.
1. Embolic: May be arterial (e.g., aortic atheroma or large vessel atherosclerosis in the carotid, vertebral, or basilar arteries) or cardiac (e.g., left ventricular thrombus postmyocardial infarction [post-MI], atrial fibrillation, valvular disorders, and cardiac tumors) in origin and most often occurs suddenly, with deficits indicating focal loss of brain function.
2. Thrombotic: May be caused by stenosis of smaller intracerebral arteries, a hyper-coagulable state, or a systemic inflammatory condition causing vasculitis, with symptoms that may fluctuate in presence and intensity.
II. NORMAL CAROTID ANATOMY
A. The aortic arch normally gives rise to the innominate artery (aka brachiocephalic artery), the left common carotid artery (CCA), and the left subclavian artery (Fig. 28.1). The innominate artery bifurcates into the right CCA and the right subclavian artery. The left common carotid arises from the aortic arch in 70% of people and from the innominate artery in 20% (“bovine arch” variant).
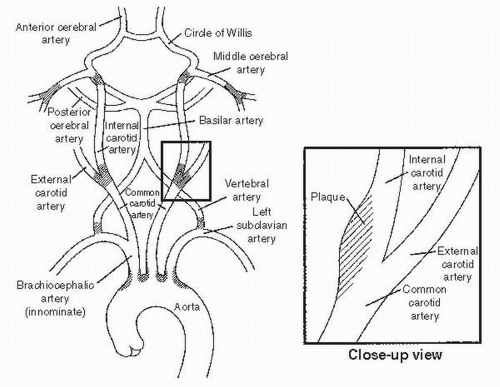 FIGURE 28.1 Normal anatomy of the aortic arch, great vessels, and circle of Willis. The shaded regions depict the areas most prone for the development of atherosclerosis. |
B. The aortic arch can be classified into three types based on the distance of the origin of the great vessels from the top of the arch (Fig. 28.2). The widest diameter of the left common carotid is used as a reference unit. If all the great vessels originate within an arc of the aortic arch subtended by a line parallel to a horizontal reference line at the top of the arch and separated from the top reference line by the reference unit, it is classified as a type I arch. In a type II arch, all the great vessels originate within an arc within two reference units from the top of the arch, and in a type III arch the great vessels originate within an arc beyond two reference units from the top of the arch. Type III arches are harder to access during percutaneous intervention than type I arches.
C. The CCAs divide into the internal and external carotids at the C4-5 level in 50% of the patients. In approximately 40% of patients, the bifurcation is higher, and it is lower in the remaining 10%.
D. The external carotid artery provides flow to the facial muscles, scalp, and thyroid. It has a complex system of collaterals, and symptoms from stenosis are rare.
E. The circle of Willis provides collateral flow between the left and right hemispheres of the brain and connects the anterior and posterior circulation.
III. RISK FACTORS FOR CAROTID ATHEROSCLEROSIS
A. Smoking and age
are the two most important risk factors for developing carotid atherosclerosis. The others, in order of importance, are hypertension, diabetes, gender (men more than women if younger than 75 years; women more than men if older than 75 years), and hyperlipidemia. As with coronary artery disease (CAD), inflammation likely plays a major role in carotid disease. African American men and Hispanic Americans appear to have a higher incidence of carotid atherosclerosis. Some data suggest a role for chronic infection in the development of carotid disease.
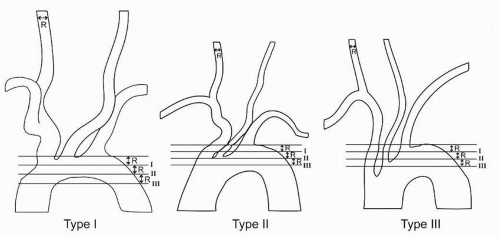 FIGURE 28.2 Aortic arch classification. The classification system is based on the distance of the origin of the great vessels from the top of the arch. |
B. Elevated serum lipoprotein(a) has been associated with intracranial, extracranial, and aortic large artery occlusive disease.
C. Between 30% and 60% of patients with peripheral arterial disease have carotid disease, and approximately 50% to 60% of patients with carotid disease have severe CAD. However, only 10% of patients with CAD have severe carotid disease.
IV. PATHOPHYSIOLOGY
A. As with coronary disease, atherosclerotic carotid disease usually develops at branch points and bends, especially at the bifurcation of the CCA and origin of the internal carotid artery (ICA) (Fig. 28.1).
B. Plaque is most often localized at the carotid bifurcation and tends to extend from the outer wall of the carotid bulb into the ICA origin (Fig. 28.1).
C. The reasons that carotid stenoses become symptomatic are not completely understood, but there is a linear increase in the risk of stroke as the stenosis increases to > 70%. Two hypotheses explain how carotid disease can cause stroke.
1. Carotid plaque is highly vascularized. Rupture of this vasculature or rupture of the plaque can result in plaque hemorrhage or ulceration, with subsequent in situ thrombus formation. This can lead to complete vessel obstruction or distal atherothromboembolism. This mechanism accounts for most cerebrovascular events caused by carotid disease.
2. Larger plaques can result in high-grade carotid stenosis or obstruction, with subsequent ischemic stroke due to a reduction in cerebral flow, in the setting of inadequate or absent collateral circulation.
V. DIAGNOSIS
A. History and physical examination
1. Careful history can aid in the localization of neurologic symptoms. Hemispheric symptoms include unilateral weakness, numbness, difficulty with speech, and visual field defects, whereas vertebrobasilar symptoms can include cerebellar disturbances such as ataxia or brain stem symptoms including syncope, dysphagia, dysarthria, or diplopia. Amaurosis fugax is transient, unilateral vision loss ipsilateral to a carotid lesion.
2. An assessment for the presence of a cervical bruit is an important part of the physical examination but should not be relied on as the sole marker for the presence of carotid disease. In the North American Symptomatic Carotid Endarterectomy Trial (NASCET), the presence of a cervical bruit had an approximately 60% sensitivity and specificity for high-grade carotid stenosis. In the Framingham study, the presence of a carotid bruit in asymptomatic patients doubled the risk of stroke, but most of these strokes occurred in vascular beds different from those of the carotid bruit. The presence of a bruit may be a general marker for patients at higher risk for cerebrovascular and cardiovascular events.
3. In addition to auscultation for carotid bruits, a complete evaluation in a patient with symptoms includes a focused neurologic examination to correlate symptoms with neurologic territory, a funduscopic examination to detect retinal embolization, and a cardiac examination to rule out potential cardioembolic sources for symptoms.
4. All patients should have an evaluation of the carotid arteries after a stroke or a transient ischemic attack (TIA). The risk of a second stroke is elevated for several years after the first stroke or TIA. Symptomatic patients with 70% or more stenosis have an 8% risk of stroke at 30 days and a 13% annual incidence of stroke. The risk of stroke in asymptomatic patients increases as the degree of carotid stenosis increases. Asymptomatic patients with 60% or more stenosis have a stroke risk of approximately 2% per year. Asymptomatic patients with 80% or more stenosis have a risk of approximately 5% per year.
B. Duplex ultrasound
1. Although carotid angiography is the gold standard, duplex ultrasound is the most widely used method for the detection and quantification of carotid artery disease. It has a sensitivity and specificity of > 80% among patients with 70% to 99% stenoses and sensitivity and specificity of > 95% among patients with complete carotid occlusion. Due to its high sensitivity and specificity in severe carotid disease and its noninvasive nature, duplex ultrasound should be the first study performed to assess for carotid disease.
2. The ultrasound diagnosis of carotid stenosis is based largely on peak systolic and end-diastolic velocities in the ICA. Duplex ultrasound criteria for carotid stenosis vary by institution, and each vascular laboratory must assess the accuracy of its criteria for stenosis in a quality assurance program. Compared with angiography, duplex ultrasound is noninvasive, less expensive, and can be done at the bedside. Limitations include the inability to image intracranial disease, limited ability to assess collateral flow, occasional inaccuracy in distinguishing high-grade stenoses (“string sign”) from complete obstructions, and the need for an experienced sonographer. Conditions that may elevate intravascular flow velocities, such as common carotid disease, vessel tortuosity, contralateral carotid disease, or presence of a carotid stent, may result in an artificially high estimate of ICA stenosis. The ability of ultrasound to assess the posterior carotid circulation is limited.
C. Computed tomography angiography (CTA)
1. CTA offers high sensitivity and specificity for the identification of severe (> 70%) carotid artery disease (sensitivity 75% to 100%, specificity 63% to 95%, negative predictive value up to 100%). CTA allows for visualization of the carotid artery lumen as well as adjacent bony and soft tissue structures. Advantages include high sensitivity (particularly for carotid artery occlusion), reproducibility, and the ability to visualize the entire carotid artery including the extracranial and intracranial portions. Disadvantages include cost and the need for contrast injection, which may be unsuitable for patients with chronic kidney disease or volume overload.
D. Magnetic resonance angiography
1. Contrast-enhanced magnetic resonance angiography (CEMRA) is rapidly gaining acceptance as a sensitive (91% to 95%) and specific (88% to 92%) test for severe carotid disease. Advantages include high sensitivity, reproducibility, and the ability to visualize the entire carotid artery including the extracranial and intracranial portions. The use of a paramagnetic agent as a vascular contrast confers higher quality images less prone to artifact. Disadvantages include high cost and the inability to study critically ill patients, claustrophobic patients, or patients with ferromagnetic implants such as pacemakers.
2. The combination of CEMRA and Doppler ultrasound results in a lower number of misclassifications and higher sensitivity and specificity for the diagnosis of severe ICA stenosis. When there is concern regarding the accuracy of one study, it is justifiable to perform both.
E. Contrast angiography
1. Contrast angiography with digital subtraction angiography (DSA) is the gold standard for assessment of carotid atherosclerosis. It allows the simultaneous assessment of the aortic arch, subclavian arteries, vertebral arteries, and intracranial circulation. Angiography enables the accurate assessment of collateral circulation. This is important because the presence of collateral circulation in medically treated patients with high-grade stenosis reduces the risk of ipsilateral stroke.
2. The risk of neurologic events during carotid angiography has historically been cited from as low as 0.5% for major events to as high as 4% for all events. In the hands of an experienced interventional cardiologist, the risk of stroke in one study was found to be approximately 0.5%. In our institution, 1 stroke was
observed in 580 consecutive diagnostic carotid catheterizations. Nonetheless, the risk-benefit ratio of performing carotid angiography must be carefully evaluated for each patient.
observed in 580 consecutive diagnostic carotid catheterizations. Nonetheless, the risk-benefit ratio of performing carotid angiography must be carefully evaluated for each patient.
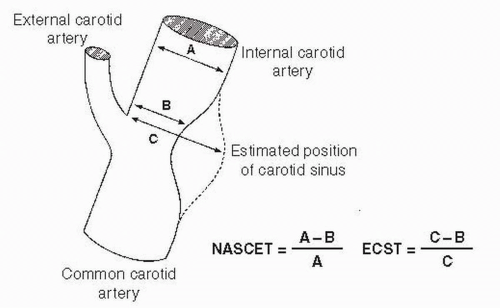
3. Two criteria are used to quantify carotid stenosis angiographically: the NASCET criteria and the European Carotid Surgery Trialists’ (ECST) Collaborative Group criteria (Fig. 28.3). According to the NASCET criteria, the normal reference internal carotid diameter is the maximum diameter of the ICA distal to the lesion and distal to the carotid bulb. According to the ECST criteria, however, the normal reference diameter is determined by the estimated position of the external wall of the carotid bulb. The same lesion has a higher percentage of stenosis using the NASCET criteria compared with the ECST criteria. In addition, the NASCET criteria are difficult to apply in subtotal occlusions with collapse of the distal ICA due to underfilling. However, the NASCET criteria inherently have less variability and are now recommended as the standard for reporting of angiographic carotid stenosis in Medicare physician quality initiatives.
4. Technique
a. Complete cerebral angiography involves angiography of the aortic arch and carotid arteries, intracerebral angiography, and angiography of the vertebral arteries and posterior circulation.
b. A low-osmolar or iso-osmolar, nonionic, heparinized contrast agent should be used. In the absence of contraindications, the patient should be antico-agulated with 50 U/kg of intravenous heparin. The patient’s head is often put in a holder or immobilizer to prevent inadvertent movement, and the patient is advised to look at the ceiling or keep his or her eyes closed. DSA should be used, if available, to improve resolution and minimize the amount of contrast needed. Before obtaining each cine angiogram, the patient should be instructed not to move, breathe, or swallow during image acquisition.
c. Aortic arch angiography is performed using an angled pigtail catheter. Using a 0.035” guidewire, the pigtail catheter is positioned in the mid-portion of the ascending aorta, and a cine angiogram of the aortic arch is obtained in a left anterior oblique projection (approximately 45°).
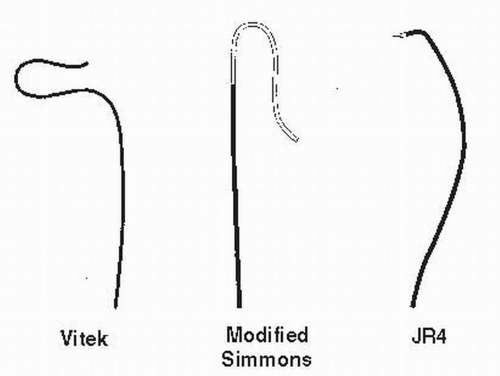
d. Carotid angiography can be safely performed using a Judkins right (JR4) or a Headhunter catheter. Alternatively, a Vitek catheter can be used with
bovine anatomy or type II or III arch. The Simmons catheter is useful in cases of severe tortuosity but requires reshaping in the aortic arch, which can lead to higher complication rates (Fig. 28.4). In the left anterior oblique projection, the JR4 catheter is positioned in the superior portion of the ascending aorta and rotated counterclockwise until it is positioned in the innominate artery. Nonselective cine angiography of the innominate, right subclavian, right carotid, and right vertebral arteries can then be performed with the image train in the right anterior oblique projection. In the right anterior oblique projection, a 0.035” wire (e.g., Stiff-Angled Glide, Magic Torque, and Wholey) is used to advance the JR4 catheter to selectively engage the right common carotid. Two basic views should be obtained for each carotid: an ipsilateral oblique view (30° to 45°) and a cross-table lateral view. The table should be positioned so that the carotid bifurcation is in the middle of the screen, and shutters and filters should be used to optimize image quality.
bovine anatomy or type II or III arch. The Simmons catheter is useful in cases of severe tortuosity but requires reshaping in the aortic arch, which can lead to higher complication rates (Fig. 28.4). In the left anterior oblique projection, the JR4 catheter is positioned in the superior portion of the ascending aorta and rotated counterclockwise until it is positioned in the innominate artery. Nonselective cine angiography of the innominate, right subclavian, right carotid, and right vertebral arteries can then be performed with the image train in the right anterior oblique projection. In the right anterior oblique projection, a 0.035” wire (e.g., Stiff-Angled Glide, Magic Torque, and Wholey) is used to advance the JR4 catheter to selectively engage the right common carotid. Two basic views should be obtained for each carotid: an ipsilateral oblique view (30° to 45°) and a cross-table lateral view. The table should be positioned so that the carotid bifurcation is in the middle of the screen, and shutters and filters should be used to optimize image quality.
e. For cerebral angiography, the patient’s head is positioned in the center of the screen. Cine angiography is performed in the posteroanterior and lateral projections. It is important to continue the cine until the venous runoff has been captured to assess for intracranial arterial venous malformations and anomalous venous drainage. To selectively engage the left carotid, the catheter is positioned in the innominate artery so that the tip is pointing superiorly. The catheter is slowly pulled back, ensuring that the tip remains pointed superiorly, until the catheter tip exits the innominate and engages the left common carotid. The same views can then be obtained for the left carotid.
VI. MANAGEMENT OF CAROTID DISEASE
A. Medical management
1. Risk factor modification.
Aggressive cardiovascular risk factor modification is recommended to reduce the risk of stroke and prevent the progression of existing disease, regardless of whether or not revascularization is indicated. Smoking cessation, blood pressure control to levels recommended by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC7) guidelines (< 140/90 mm Hg and more aggressive control in patients with atherosclerotic cardiovascular disease,
chronic kidney disease, or diabetes), control of diabetes (HbA1c < 7%), and lipid management (goal low-density lipoprotein [LDL] < 100 mg/dL, < 70 mg/dL if high CAD risk) are important treatment goals for which to strive in any patient with carotid disease.
chronic kidney disease, or diabetes), control of diabetes (HbA1c < 7%), and lipid management (goal low-density lipoprotein [LDL] < 100 mg/dL, < 70 mg/dL if high CAD risk) are important treatment goals for which to strive in any patient with carotid disease.
2. Antiplatelet therapy
a. The Antiplatelet Trialists’ meta-analysis including 73,247 high-risk patients found that antiplatelet therapy as secondary prevention resulted in a 27% (25% attributed to aspirin) relative reduction in the combined end point of vascular death, MI, and stroke.