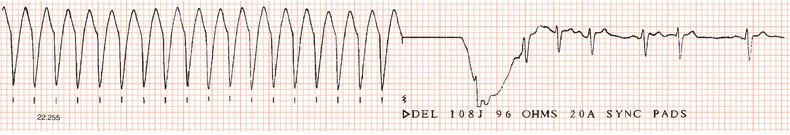
Electrical cardioversion is the use of an electric shock of brief duration and high energy to terminate a tachyarrhythmia (Figure 21.1). The shock depolarises the myocardium, thus interrupting the tachycardia and allowing the sinus node to resume control of the heart rhythm.
Chemical cardioversion is the restoration of normal rhythm by antiarrhythmic drugs, and it is discussed elsewhere.
Transthoracic cardioversion
Cardioversion is usually carried out by delivering a shock between two electrodes placed on the chest.
Procedure
Facilities for monitoring the ECG and for cardiopulmonary resuscitation must be available.
The rhythm should be checked immediately before cardioversion to ensure that spontaneous reversion has not occurred.
Anaesthesia
The patient should fast for four hours before elective cardioversion.
A conscious patient should receive a short-acting general anaesthetic, or alternatively intravenous drugs to achieve deep but brief sedation. Small incremental doses of intravenous midazolam (total 1–10 mg) in combination with fentanyl (50 mg) are very effective. It is essential that the patient’s airway and oxygen saturation are carefully monitored and that drugs to reverse fentanyl (i.e. naloxone) and midazolam (i.e. flumazenil) are immediately available in the unlikely event of respiratory depression.
Delivery of shock
The shock is delivered between two electrodes. Correct positioning is important. Usually one electrode is placed at the level of the cardiac apex, close to the mid-axillary line, and the other is positioned to the right of the upper sternum.
Alternatively, a flat paddle, if available, can be placed beneath the patient’s back, behind the heart, and a second paddle positioned over the precordium. If a flat paddle is unavailable, standard electrodes can be applied anteroposteriorly if the patient is turned onto his or her side: one paddle is placed over the precordium and the other paddle below the left shoulder to the left of the spine.
To achieve good electrical contact and to avoid burning the skin, electrode jelly must be applied to the areas beneath metal paddles. However, it is essential to avoid spreading jelly between the two paddles. Pads impregnated with electrode gel prevent jelly being spread over inappropriate areas, including the operator!
The defibrillator is charged to the desired energy level (see below), which takes a few seconds. The charge is usually delivered by pressing the button(s) on the defibrillator paddle(s). Metal paddles should be applied with firm pressure to reduce the electrical resistance of the thorax.
Before discharge it is essential to ensure that no one is in contact with the patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree