Cardiovascular pharmacology In A Heartbeat
ACE inhibitors | ACE inhibitors are used in the treatment of hypertension and heart failure. The most notable side-effects are dry cough and angioedema, which are reversible on stopping. |
ARBs | ARBs antagonise the effects of ATII at its receptor and mimic the effects of ACE inhibitors. They are used in patients who are intolerant of ACE inhibitor therapy. |
Beta-blockers | Beta-blockers exert their effects by antagonising the actions of adrenaline and noradrenaline at beta-adrenergic receptors. They are used in heart failure, arrhythmias and coronary artery disease. These should be used with caution in asthmatics. |
Calcium channel blockers | Calcium channel blockers block L-type calcium channels. There are two classes of CCB; non rate-limiting CCBs used in the treatment of angina and hypertension and rate-limiting CCBs used to treat arrhythmias. Rate-limiting CCBs are contraindicated in heart failure. |
Antiarrhythmics | Antiarrhythmic drugs are classified according to their modes of action which include effects on Na channels and K channels. These drugs have an extensive list of side-effects and interactions, and it is important to note that they can be pro-arrhythmic as well. |
Antiplatelet agents | Antiplatelet agents prevent thrombus formation and are indicated in the prevention of cardiovascular events. Aspirin works by inhibiting the COX enzyme and clopidogrel works by antagonising ADP receptors on platelets. |
Anticoagulants | Anticoagulants interfere with prothrombotic mediators in the coagulation cascade. Warfarin inhibits synthesis of vitamin K clotting factors (II, VII, IX and X) and toxicity is reversed with administration of Vitamin K. Novel oral anticoagulants (apixaban, rivaroxaban and dabigatran) are increasingly used as they do not require regular monitoring. However, in cases of overdose/haemorrhage there is no direct antidote. |
Nitrates | Nitrates are vasodilators used in the treatment of angina. Common side-effects include headache and flushing, which are usually short lived. Tolerance is a known complication of nitrate treatment. |
Diuretics | Diuretics work by increasing sodium excretion and increasing urine output. Loop diuretics are used in heart failure, whereas thiazide diuretics are used in hypertension. Diuretics can have marked effects on electrolyte levels, with clinically important effects on potassium. Potassium sparing diuretics include amiloride and spironolactone. Spironolactone is an aldosterone antagonist. |
Lipid-lowering agents | Lipid-lowering drugs are exemplified by the statins, which work by inhibiting HMG CoA reductase. Well-known side-effects of statins include muscle pain and disturbed liver enzyme profiles. Note that deranged LFTs are more common. Other lipid-lowering drugs include ezetimibe, fibrates and bile acid sequestrants. |
5.2 ACE inhibitors
Drugs that end in ‘-pril’
e.g. enalapril, ramipril, lisinopril
ACE inhibitors are drugs primarily used to treat hypertension and heart failure as well as reduce mortality after myocardial infarction. Their inhibitory action on angiotensin-converting enzyme results in a reduction in blood pressure, which makes them useful medications in the treatment of hypertension. ACE inhibitors are widely used in clinical practice due to their low cost and narrow side-effect profile.
5.2.1 Mechanism of action
- ACE activity is greatest in the vascular epithelium of the lungs, but occurs in all vascular beds
- ACE inhibitors do exactly as their name suggests: they inhibit Angiotensin-Converting Enzyme
- This prevents the conversion of angiotensin I to angiotensin II
- This prevents angiotensin II from exerting its physiological effects on the:
- peripheral vasculature (vasoconstriction)
- heart (increases heart rate and contractility via sympathetic activation)
- kidneys
– aldosterone activation: causes sodium reabsorption
– ADH activation: causes water retention
– vasoconstriction of glomerular efferent arterioles: causes increased sodium reabsorption.
- peripheral vasculature (vasoconstriction)
5.2.2 Indications
- Hypertension
- Secondary prevention of acute coronary syndrome
- Heart failure and left ventricular dysfunction.
EXAM | ACE inhibitors improve mortality when used for all of these indications. |
// Why? //
Why do you give ACE inhibitors after an MI?
ACE inhibitors prevent the remodelling effects of angiotensin II on the ventricle after an MI, therefore reducing the onset of heart failure and recurrent MI.
5.2.3 Contraindications
ACE inhibitors are teratogenic and are absolutely contraindicated in pregnancy. They should also be avoided in patients with bilateral renal artery stenosis, acute kidney injury, chronic kidney disease and in hyperkalaemia.
// Why? //
Why are ACE inhibitors contraindicated in bilateral renal artery stenosis?
ACE inhibitors reduce the already compromised renal perfusion in bilateral renal artery stenosis by inhibiting angiotensin II. Angiotensin II increases blood flow to the kidneys by constricting the glomerular efferent arterioles. This may result in worsening renal failure and pulmonary oedema.
5.2.4 Side-effects
- Dry cough: this is due to an accumulation of bradykinin in the lungs as a direct result of kinase inhibition. Patients are usually switched to an angiotensin receptor blocker (ARB).
- Hypotension: this may be marked, causing orthostatic symptoms potentially warranting down-titration of dose
- Hyperkalaemia: this risk is increased with concurrent use of potassium sparing diuretics, e.g. spironolactone
- Renal impairment: in particularly at-risk groups such as renal failure
- Angioedema: this is rare but can be fatal if it compromises the airway.
// PRO-TIP //
Treatment of hyperkalaemia
To stabilise the myocardium (if abnormal ECG) | • IV calcium gluconate or |
To reduce potassium rapidly | • IV dextrose ± insulin |
To eliminate potassium | • Restore kidney function |
5.3 Angiotensin receptor blockers
Drugs that end in ‘-sartan’
e.g. candesartan, losartan, valsartan
In contrast to ACE inhibitor treatment, where the production of angiotensin II is reduced, angiotensin receptor blockers (ARBs) work by directly antagonising the effects of angiotensin II at its receptor. Clinical indications are the same as those listed for ACE inhibitors. As ARBs are more expensive than ACE inhibitors, they are generally only used to treat patients who are intolerant of ACE inhibitor therapy (i.e. when there is a persistent cough).
Contraindications are similar to those of ACE inhibitors. ARBs mimic clinical advantages of ACE inhibitors and share a similar side-effect profile, with the exception of a dry cough.
5.4 Beta-blockers
These are the drugs that end in ‘-olol’
- Non-selective (β1 and β2): propranolol, carvedilol
- β1 selective: atenolol, metoprolol, bisoprolol
Beta-blockers have been historically utilised in the treatment of hypertension. Newer agents, however, have superseded their role in that capacity. They are nevertheless important in the management of conditions such as heart failure and coronary artery disease.
5.4.1 Mechanism of action
- Beta-blockers block the action of adrenaline and noradrenaline on beta-adrenergic receptors
- Beta-blockers reduce SA nodal and AV nodal conduction as well as myocardial contractility, earning them the terms negative chronotropes and negative inotropes, respectively
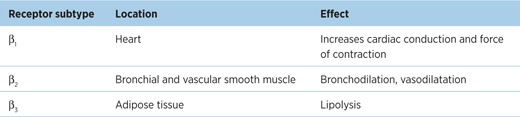
- There are three main subtypes of beta-receptors (see Table 5.1). Some beta-blockers block all beta-adrenergic receptors while some are selective (see below).
Table 5.1 – Effects on beta receptors
// Why? //
Beta-blockers reduce heart rate, consequently increasing diastolic filling time and improved end-diastolic volumes increase stroke volume and cardiac output (and coronary blood flow). They also reduce the sympathetic activity driving left ventricular remodelling and worsening myocardial function.
5.4.2 Indications
- Secondary prevention of MI: reduces mortality
- Chronic heart failure: reduces mortality (see below)
- Atrial fibrillation (rate control)
- Stable angina
- Hypertension (not first-line therapy)
- Others: tremor, anxiety, palpitations, tachycardia.
5.4.3 Contraindications
- Asthma (severe)
- Worsening or unstable heart failure
- Second- or third-degree heart block or marked bradycardia
- Raynaud’s disease (refer to Chapter 15)
EXAM | Beta-blockers are relatively contraindicated in asthma due to risk of bronchospasm. A switch to a calcium channel blocker is indicated at this point. However, if a beta-blocker must be used, a β1-selective drug such as bisoprolol is preferred over a non-selective drug such as propranolol. |
5.4.4 Side-effects
- Cardiovascular: bradycardia, hypotension, cold peripheries
- Other: bronchospasm, erectile dysfunction, lethargy/fatigue, headache, sleep disturbances
- Masked hypoglycaemia in patients with diabetes (beta-blockers dampen the autonomic responses to hypoglycaemia, such as tachycardia).
EXAM | Beta-blockers in combination with rate-limiting calcium channel blockers (e.g. verapamil) can result in severe bradycardia and heart failure. This combination is best avoided. |
5.5 Calcium channel blockers
Rate-limiting: verapamil, diltiazem
Non rate-limiting: nifedipine, amlodipine
Calcium channel blockers (CCBs) are classified into two main categories based on their affinities for their various sites of action; non rate-limiting dihydropyridines (DHPs) and rate-limiting non-dihydropyridines (NDHPs). These drugs will be discussed according to this classification.
5.5.1 Mechanism of action
Non rate-limiting | Rate-limiting |
Site: blocks L-type calcium channels in smooth muscle cells of the coronary and systemic vasculature | Site: blocks L-type calcium channels in cells of the myocardium and nodal conducting tissues |
Effect: dilates coronary and systemic vessels (reduces left ventricular afterload) | Effect: reduces myocardial contractility (negative inotropic effect) and decreases heart rate (negative chronotropic effect) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


