Cardiovascular Pharmacology
 Just the facts
Just the factsIn this chapter, you’ll learn:
♦ guidelines for administering emergency medications
♦ drugs commonly used in advanced cardiac life support (ACLS)
♦ drug indications and dosages
♦ the most common drug interactions encountered in ACLS practice
♦ antidotes for the most common drug overdoses.
Emergency medication administration
Emergency medications used during ACLS are given most frequently by I.V. push or I.V. infusion. If you can’t obtain peripheral or central I.V. access, then you may give medications via the intraosseous (I.O.) route (bone marrow cavity is accessed) and some drugs via an endotracheal (ET) tube during cardiac arrest. Depending on the specific situation, you may also give medications subcutaneously, orally, or sublingually.
Here are some general pointers to remember when administering medication:
Keep in mind that elderly patients usually require smaller dosages than do other adult patients.
You may need to reduce the dosage for an adult patient with organ impairment (especially kidney or liver) because drug metabolism and excretion may be altered significantly.
Remember that a patient may be taking over-the-counter (OTC) medications, illegal drugs, or herbal remedies or may be consuming food or beverages that interact with the medication.
Be aware that a patient may have known or unknown drug allergies; any medication has the potential to cause an anaphylactic or hypersensitivity reaction.
After you administer a medication, continually monitor the patient for the drug’s effects, including adverse reactions. This includes continuous cardiac monitoring; assessing his vital signs before, during, and after giving the medication; and additional assessment indicated by the drug’s use.
|
ACE inhibitors
Angiotensin-converting enzyme (ACE) inhibitors are used to reduce mortality and improve left ventricular function in patients with postacute myocardial infarction (MI). They prevent adverse left ventricular remodeling, delay the progression of heart failure, and decrease sudden death and recurrent MI.
Usually given within the first 24 hours after the onset of acute MI symptoms and after blood pressure has stabilized, ACE inhibitors are indicated for suspected MI and ST-segment elevation in two or more precordial leads, hypertension, and heart failure (without hypotension) in patients not responding to digoxin or diuretics. ACE inhibitors should also be used when clinical signs of acute MI with left ventricular dysfunction are present and left ventricular ejection fraction is less than 40%. (See General precautions for ACE inhibitors.)
ACE-ing hypertension
ACE inhibitors reduce blood pressure by interrupting the reninangiotensin-aldosterone cycle. They specifically prevent the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. Reduced formation of angiotensin II decreases peripheral arterial resistance, thus decreasing aldosterone secretion, sodium and water retention, and blood pressure. ACE inhibitors also decrease systemic vascular resistance (afterload) and pulmonary artery wedge pressure (PAWP; preload), thus increasing cardiac output in patients with heart failure. (See How ACE inhibitors work, page 126.)
The ACE inhibitors given during ACLS include captopril, enalapril, lisinopril, and ramipril.
Captopril
Captopril (Capoten) is used to treat hypertension, heart failure, and acute MI. It prevents the conversion of angiotension I to angiotension II, decreasing systemic vascular resistance and
increasing cardiac output. By reducing aldosterone secretion, captopril promotes sodium and water excretion, which reduces the amount of blood that the heart needs to pump, thus lowering blood pressure.
increasing cardiac output. By reducing aldosterone secretion, captopril promotes sodium and water excretion, which reduces the amount of blood that the heart needs to pump, thus lowering blood pressure.
|
General precautions for ACE inhibitors
Observe these general precautions when you administer angiotensin-converting enzyme (ACE) inhibitors:
Don’t give to pregnant women because fetal injury or death may occur.
Don’t give to patients taking lithium because ACE inhibitors may increase lithium levels and cause toxicity.
Use with caution in patients with renal impairment.
Excessive hypotension may occur when used with diuretics or other antihypertensives.
The risk of hypoglycemia is increased in patients with diabetes.
The risk of hyperkalemia is increased in patients taking potassium-sparing diuretics.
Potassium-containing salt substitutes may cause hyperkalemia in patients taking ACE inhibitors.
How to give it
For acute MI, the initial dosage of captopril is 6.25 mg orally in a single dose. Increase to 25 mg three times per day and then to 50 mg three times per day, as tolerated. Several weeks of therapy may be required before beneficial effects are seen.
What can happen
Adverse reactions to captopril include hypotension; tachycardia; angina; angioedema; persistent, dry nonproductive cough; hyperkalemia; leukopenia; and agranulocytosis.
What to consider
Closely monitor blood pressure response to the drug.
Monitor the patient’s potassium intake and potassium level. Patients with diabetes, those with impaired renal function, and those receiving drugs that may increase the potassium level may develop hyperkalemia.
Assess renal function before and periodically throughout therapy.
Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) may decrease the antihypertensive effect of captopril.
Captopril may increase serum digoxin and lithium levels, leading to toxicity.
Captopril is contraindicated during pregnancy.
 Now I get it!
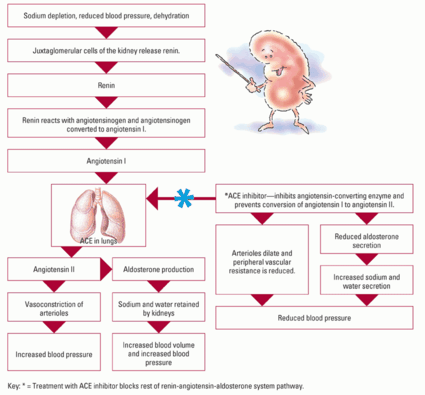
Now I get it!How ACE inhibitors work
Angiotensin-converting enzyme (ACE) inhibitors reduce blood pressure by interrupting the renin-angiotensinaldosterone system, which prevents the conversion of angiotensin I to angiotensin II.
The renin-angiotensin-aldosterone system pathway
|
Key: * = Treatment with ACE inhibitor blocks rest of renin-angiotensin-aldosterone system pathway.
Enalapril
Enalapril (Vasotec) is used to treat hypertension and heart failure. Like captopril, it prevents the conversion of angiotension I to angiotension II, thus reducing blood pressure. You may also give the I.V. form of enalapril—enalaprilat (Vasotec I.V.).
How to give it
Here’s how to administer enalapril:
Orally—Give 2.5 mg as a single dose initially and then increase to 20 mg two times per day.
I.V.—Give an initial 1.25 mg I.V. dose slowly over 5 minutes, and then 1.25 to 5 mg I.V. every 6 hours. Alternatively, you can dilute the drug in 50 mL of a compatible solution (such as dextrose 5% in water [D5W], normal saline solution for injection, dextrose 5% in lactated Ringer’s solution, dextrose 5% in normal saline solution for injection, or Isolyte E) and infuse it over 15 minutes.
What can happen
Adverse reactions to enalapril include hypotension; tachycardia; angina; angioedema; persistent, dry nonproductive cough; hyperkalemia; leukopenia; and agranulocytosis.
|
What to consider
Closely monitor blood pressure response to the drug.
Monitor the patient’s potassium intake and potassium level. Patients with diabetes, those with impaired renal function, and those receiving drugs that may increase the potassium level may develop hyperkalemia.
Assess renal function before and throughout therapy; monitor the patient for increased blood urea nitrogen (BUN) and creatinine levels.
Aspirin and other NSAIDs may decrease the antihypertensive effect of enalapril.
Enalapril is contraindicated during pregnancy and in patients with angioedema or bilateral renal artery stenosis.
Lisinopril
Lisinopril (Prinivil, Zestril) is used to treat hypertension and heart failure as well as to improve patient survival after acute MI. Like the other ACE inhibitors, it lowers blood pressure by preventing the conversion of angiotension I to angiotension II.
How to give it
Here’s how to administer lisinopril:
For heart failure—Give 5 mg orally once per day.
For acute MI—Give 5 mg orally within the first 24 hours of symptom onset, 5 mg after 24 hours, and 10 mg once per day after 48 hours for 6 weeks.
|
What can happen
Adverse reactions to lisinopril include hypotension; tachycardia; angina; angioedema; persistent, dry nonproductive cough; hyperkalemia; and leukopenia.
What to consider
Closely monitor blood pressure response to the drug.
Monitor the patient’s potassium intake and potassium level. Patients with diabetes, those with impaired renal function, and those receiving drugs that may increase the potassium level may develop hyperkalemia.
Use lisinopril cautiously in patients with impaired renal function because hyperkalemia may occur. BUN and creatinine levels may increase.
Aspirin and other NSAIDs may decrease the antihypertensive effect of lisinopril.
Lisinopril is contraindicated during pregnancy and for patients with a history of angioedema.
Ramipril
Ramipril (Altace) is used to treat hypertension and heart failure. It prevents the conversion of angiotension I to angiotension II, thus reducing blood pressure.
How to give it
The initial dosage of ramipril is 2.5 mg orally in a single dose. Maintenance dosage is 2.5 to 20 mg daily depending on the indication.
What can happen
Adverse reactions to ramipril include hypotension; tachycardia; angina; angioedema; persistent, dry nonproductive cough; hyperkalemia; and leukopenia.
What to consider
Closely monitor blood pressure response to the drug.
Monitor the patient’s potassium intake and potassium level. Patients with diabetes, those with impaired renal function, and those receiving drugs that may increase the potassium level may develop hyperkalemia.
Assess renal function closely during the first few weeks of therapy, especially in patients with severe heart failure or hypertension. BUN and creatinine levels may rise.
NSAIDs may decrease the antihypertensive effect of ramipril.
Ramipril is contraindicated during pregnancy.
|
Adrenergics
Adrenergic drugs are also called sympathomimetic drugs because they produce effects similar to those produced by the sympathetic nervous system (SNS). These drugs are typically used in ACLS as cardiac stimulants to restore heart rate, rhythm, and blood pressure while resuscitating the patient. Adrenergic drugs include dobutamine hydrochloride, dopamine hydrochloride, epinephrine, isoproterenol, and norepinephrine. Vasopressin, or antidiuretic hormone, is a posterior pituitary hormone that has adrenergic properties and is used as an alternative drug to epinephrine to treat adult shock-refractory ventricular fibrillation (VF).
Dobutamine hydrochloride
Dobutamine is used to increase cardiac output in patients experiencing cardiac decompensation with a systolic blood pressure of 70 to 100 mm Hg and no accompanying signs of shock.
|
Selective stimulator
Dobutamine selectively stimulates beta-1 adrenergic receptors to increase myocardial contractility and stroke volume. This results in increased cardiac output (a positive inotropic effect). Systolic blood pressure and pulse pressure may remain unchanged or may increase as a result of increased cardiac output.
At therapeutic doses, dobutamine decreases peripheral resistance (afterload), reduces ventricular filling pressure (preload), and may facilitate atrioventricular (AV) node conduction.
How to give it
Give an I.V. infusion of 2 to 20 mcg/kg/minute; titrate so that the patient’s heart rate isn’t greater than 10% of baseline. Remember,
you must use an infusion pump or other device to control the flow rate.
you must use an infusion pump or other device to control the flow rate.
Key points
Dobutamine hydrochloride
Increases cardiac output
Indications: cardiac decompensation situation with systolic blood pressure of 70 to 100 mm Hg and no signs of shock
Continuous I.V. infusion: 2 to 20 mcg/kg/minute, titrated so that cardiac rate isn’t greater than 10% of baseline
What can happen
Adverse reactions to dobutamine include tachycardia, fluctuations in blood pressure (hypertension, hypotension), bronchospasm, headache, and nausea.
What to consider
Before giving dobutamine, use the appropriate plasma volume expanders to correct hypovolemia.
Monitor the patient’s heart rate and rhythm and blood pressure response to the drug; hemodynamic monitoring is recommended to monitor the drug’s effect.
Avoid administering dobutamine when systolic blood pressure is less than 100 mm Hg and signs of shock exist.
Don’t give dobutamine if poisoning or drug-induced shock is suspected.
Don’t give beta-adrenergic blockers with dobutamine because these drugs may cause increased peripheral resistance.
Don’t give tricyclic antidepressants with dobutamine because these drugs may potentiate pressor response and cause arrhythmias.
Don’t give in the same I.V. line with other drugs.
Tissue necrosis and sloughing may occur if the I.V. medication leaks into surrounding tissue.
|
Dopamine hydrochloride
Although it’s an adrenergic, dopamine is also classified as a vasopressor. Dopamine is used as a secondary drug (after atropine) for symptomatic bradycardia. It’s also used to treat hypotension accompanied by signs and symptoms of shock.
Dopamine stimulates the dopaminergic, beta-adrenergic, and alpha-adrenergic receptors of the SNS. It has a direct stimulating effect on beta-1 receptors and little or no effect on beta-2 receptors.
Dose dependence
The effects of dopamine are dose-dependent. In I.V. doses of 0.5 to 5 mcg/kg/minute, it acts on dopaminergic receptors (dopaminergic response), causing vasodilation in the renal, mesenteric, coronary, and intracerebral vascular beds. Low to moderate doses (5 to 10 mcg/kg/minute) produce a beta effect, which results in cardiac stimulation. In I.V. doses greater than 10 mcg/kg/minute, it
stimulates alpha receptors, which results in increased peripheral resistance and renal vasoconstriction.
stimulates alpha receptors, which results in increased peripheral resistance and renal vasoconstriction.
|
How to give it
Give an I.V. infusion of 2 to 20 mcg/kg/minute and titrate to the patient’s response; taper the infusion slowly.
Livin’ large
Remember to administer dopamine on an infusion pump into a large vein (central venous access is recommended) to prevent the possibility of extravasation. (Phentolamine 5 to 10 mg in 10 to 15 mL of normal saline solution is used to infiltrate the area to minimize tissue necrosis if extravasation occurs in a peripheral site. Infiltration must be done within 12 hours of extravasation.) Adjust the dosage to meet individual patient needs and to achieve the desired response. Reduce the dosage as soon as the patient’s hemodynamic condition is stabilized.
What can happen
Adverse reactions to dopamine include bradycardia, tachycardia, ventricular arrhythmias, conduction disturbances, hypertension, anxiety, and dyspnea. Severe hypotension may result with abrupt withdrawal of dopamine; remember to taper the dosage gradually.
Key points
Dopamine hydrochloride
Vasopressor and adrenergic
Indications: symptomatic bradycardia, hypotension with signs and symptoms of shock
Continuous I.V. infusion: low dose, 0.5 to 5 mcg/kg/minute; cardiac dose, 5 to 10 mcg/kg/minute; vasopressor dose, 10 to 20 mcg/kg/minute
What to consider
Before giving dopamine, use the appropriate plasma volume expanders to correct hypovolemia.
Monitor the patient’s heart rate and rhythm and blood pressure response to drug.
Don’t give dopamine to patients with uncorrected tachyarrhythmias, pheochromocytoma, or VF.
Use caution when giving beta-adrenergic blockers with dopamine because these drugs may antagonize cardiac effects.
Use caution when giving phenytoin (Dilantin) with dopamine because it may cause hypotension and bradycardia.
Dopamine is incompatible with alkaline solutions (sodium bicarbonate).
Tissue necrosis medication may occur if the I.V. medication leaks into surrounding tissue.
Epinephrine
Epinephrine is a naturally occurring catecholamine used for its bronchodilator, vasopressor, and cardiac stimulant effects. It’s used to treat cardiac arrest (VF, pulseless ventricular tachycardia [VT], asystole, and pulseless electrical activity [PEA]), symptomatic bradycardia (after atropine), severe hypotension, and severe allergic reactions (when combined with large fluid volumes, corticosteroids, or antihistamines).
|
Epinephrine acts directly by stimulating alpha- and betaadrenergic receptors in the SNS. Its main therapeutic effects include relaxation of bronchial smooth muscle, cardiac stimulation, and the dilation of skeletal muscle vasculature.
Relax…
Epinephrine relaxes bronchial smooth muscle by stimulating beta2-adrenergic receptors and constricts bronchial arterioles by stimulating alpha-adrenergic receptors, resulting in relief of bronchospasm, reduced congestion and edema, and increased tidal volume and vital capacity. By inhibiting histamine release, it may reverse bronchiolar constriction, vasodilation, and edema.
…Stimulate
As a cardiac stimulant, epinephrine produces positive chronotropic and inotropic effects by acting on beta1 receptors in the heart and increasing cardiac output, myocardial oxygen consumption, and the force of contraction.
|
How to give it
Here’s how to administer epinephrine:
During resuscitation—Give 1 mg (10 mL of 1:10,000 solution) I.V. push or I.O. every 3 to 5 minutes; follow each dose with a 20-mL I.V. flush and elevate the arm for 10 to 20 seconds if administering via a peripheral I.V. line in the arm. Dosages of up to 0.2 mg/kg may be considered and used with caution.
For continuous infusion—Add a 1-mg dose (1 mL of 1:1,000 solution) to 500 mL of normal saline solution or D5W; use an initial I.V. infusion rate of 1 mcg/minute; increase to 2 to 10 mcg/minute.
For profound bradycardia or hypotension—Add 1 mg of 1:1,000 solution to 500 mL of normal saline solution and infuse at a titrated dosage of 2 to 10 mcg/minute.
You can also give epinephrine via an ET tube with confirmed placement by administering 2 to 2.5 mg diluted in 10 mL of normal saline solution followed by several positive pressure ventilations.
What can happen
Adverse reactions to epinephrine include anxiety, excitability, angina, cardiac arrhythmias, palpitations, hyperglycemia, hypertension, hypertensive crisis, and cerebral hemorrhage.
Key points
Epinephrine
Produces positive chronotropic and inotropic effects by action on beta1-receptors in the heart
Indications: cardiac arrest, symptomatic bradycardia, severe hypotension, severe allergic reaction
Administer 1 mg (10 mL of 1:10,000 solution) I.V. every 3 to 5 minutes during resuscitation
May be given via endotracheal tube: 2 to 2.5 mg in 10 mL normal saline solution
When epinephrine is given with antihistamines or tricyclic antidepressants, adverse cardiac effects may be potentiated; avoid concomitant use. When used with beta-adrenergic blockers, the cardiac and bronchodilating effects of epinephrine may be antagonized. Additionally, cardiac glycosides may sensitize the myocardium to the effects of epinephrine, causing arrhythmias.
What to consider
Monitor the patient’s heart rate and rhythm and blood pressure response to the drug. Increased heart rate and blood pressure may cause myocardial ischemia.
Use with caution in patients with myocardial ischemia and hypoxia because epinephrine increases myocardial oxygen demand.
Don’t administer epinephrine with alpha-adrenergic blockers because its vasoconstriction and hypertensive effects may be counteracted.
Dosage adjustments may be necessary if the patient is taking antidiabetics because the effect of epinephrine may be decreased.
Monitor the patient’s serum glucose levels because epinephrine may cause hyperglycemia.
Higher doses of epinephrine (up to 0.2 mg/kg) may result in postresuscitation myocardial dysfunction.
Epinephrine is incompatible with alkaline solutions (sodium bicarbonate).
Tissue necrosis and sloughing may occur if the I.V. medication leaks into surrounding tissue.
|
Isoproterenol
Isoproterenol (Isuprel) is used cautiously as a temporary measure for treating symptomatic bradycardia if atropine is ineffective and an external pacemaker isn’t available. It’s also used to treat torsades de pointes that doesn’t respond to magnesium sulfate, for temporary control of bradycardia in heart transplant patients, and for counteracting beta-adrenergic blocker poisoning. Isoproterenol is contraindicated in cardiac arrest.
Quite an actor
Isoproterenol acts on beta1 adrenergic receptors in the heart, producing a positive chronotropic and inotropic effect. It usually increases cardiac output. In patients with AV block, isoproterenol
shortens conduction time and the refractory period of the AV node and increases the rate and strength of ventricular contraction.
shortens conduction time and the refractory period of the AV node and increases the rate and strength of ventricular contraction.
How to give it
For continuous infusion, add a 1-mg dose to 250 mL of D5W and give an I.V. infusion rate of 2 to 10 mcg/minute; titrate to an adequate heart rate. For torsades de pointes, titrate until the rhythm is suppressed. Always use an infusion pump.
Because of the danger of arrhythmias, the infusion rate is usually decreased or temporarily stopped if the patient’s heart rate exceeds 110 beats/minute. The order for the I.V. infusion rate should include specific guidelines for regulating the flow or terminating the infusion in relation to heart rate, premature beats, electrocardiogram (ECG) changes, myocardial ischemia, blood pressure, and urine output.
|
What can happen
Adverse reactions to isoproterenol include anxiety, excitability, angina, cardiac arrhythmias, palpitations, and hypertension.
What to consider
Remember that isoproterenol doesn’t replace the administration of blood, plasma, fluids, or electrolytes in patients with blood volume depletion.
Monitor the patient’s heart rate and rhythm and blood pressure response to the drug. Increased heart rate and blood pressure may cause myocardial ischemia.
Don’t give isoproterenol to patients with tachycardia caused by digoxin toxicity, preexisting arrhythmias (other than those that may respond to treatment with isoproterenol), and angina pectoris.
Giving isoproterenol with epinephrine or another adrenergic may cause additive reactions and result in VT and VF; allow for at least 4 hours to elapse between administrating the two drugs.
The patient is at increased risk for arrhythmias when isoproterenol is used with cardiac glycosides, potassium-depleting drugs, and other drugs that affect cardiac rhythm. Additionally, betaadrenergic blockers antagonize the effects of isoproterenol.
Norepinephrine
Norepinephrine (Levophed) is used to treat severe cardiogenic shock and significant hypotension with low total peripheral resistance. It’s the medication of last resort for the management of ischemic heart disease and shock but hasn’t been proven
to increase neurologically intact survival when compared to epinephrine in cardiac arrest.
to increase neurologically intact survival when compared to epinephrine in cardiac arrest.
|
Norepinephrine stimulates alpha- and beta-1 receptors within the SNS. It primarily produces vasoconstriction and cardiac stimulation.
How to give it
For continuous infusion, add a 4-mg dose to 250 mL of D5W or dextrose 5% in normal saline solution titrated to the desired effect; 0.5 to 1 mcg/minute I.V. infusion rate is usually titrated to improve blood pressure. Maintenance dosage is 2 to 4 mcg/minute. You may need to give a higher dosage to achieve adequate perfusion in patients with poison-induced hypotension.
Centrally speaking
Remember to administer norepinephrine via a central venous catheter using an infusion pump to minimize the risk of extravasation. (Phentolamine 5 to 10 mg in 10 to 15 mL of normal saline solution is used to infiltrate the area to minimize tissue necrosis if extravasation occurs in a peripheral site; must be done within 12 hours of extravasation.)
What can happen
Adverse reactions to norepinephrine include anxiety, excitability, angina, cardiac arrhythmias, palpitations, hypertension, hypertensive crisis, and cerebral hemorrhage.
Key points
Norepinephrine
Primarily produces vasoconstriction and cardiac stimulation
Indications: severe cardiogenic shock, significant hypotension, ischemic heart disease, and shock
Continuous infusion: 0.5 to 1 mcg/minute titrated to desired blood pressure (to maximum rate of 30 mcg/minute)
What to consider
Administering norepinephrine isn’t a substitute for blood or fluid replacement therapy. If the patient has a volume deficit, replace fluid before administering vasopressors.
Monitor the patient’s heart rate and rhythm and blood pressure response to the drug.
Monitor the patient’s extremities for color and temperature.
Don’t give alpha-adrenergic blockers with norepinephrine because these drugs may antagonize its effects.
Severe hypotension may occur when norepinephrine is used with monoamine oxidase inhibitors, methyldopa, or tricyclic antidepressants.
Norepinephrine is incompatible with alkaline solutions (sodium bicarbonate).
Tissue necrosis and sloughing may occur if the I.V. medication leaks into surrounding tissue.
Vasopressin
Vasopressin (antidiuretic hormone) is a nonadrenergic peripheral vasoconstrictor that also causes coronary and renal vasoconstriction. It’s used to treat adult shock-refractory VF as an alternative to epinephrine. It may be useful as an alternative to epinephrine for asystole or PEA. Vasopressin may also provide hemodynamic support in vasodilatory shock by maintaining coronary perfusion pressure. When given at high doses, vasopressin is a powerful vasoconstrictor of capillaries and small arterioles.
Key points
Vasopressin
In the large dose used for advanced cardiac life support, vasopressin is a powerful vasoconstrictor
Indications: adult shock-refractory ventricular fibrillation, vasodilatory shock
Cardiac arrest: 40 units I.V. push or I.O. only once
Totally tubular
Vasopressin acts at the renal tubular level to increase cyclic adenosine monophosphate (cAMP), which, in turn, increases water permeability at the renal tubule and collecting duct. This results in increased urine osmolality and a decreased urine flow rate.
How to give it
Give 40 units by I.V. push or I.O. to replace the first or second dose of epinephrine during cardiac arrest. Although vasopressin can be given endotracheally, the I.V. or I.O. route is preferred because the pharmacologic effects are more predictable. Because of the risk of necrosis and gangrene, remember to use extreme caution to avoid extravasation.
|
What can happen
Adverse reactions to vasopressin include cardiac ischemia, angina, bronchoconstriction, and water intoxication.
What to consider
Monitor the patient’s heart rate and rhythm and blood pressure response to the drug. Potent vasoconstrictor drug effects may cause myocardial ischemia.
Assess for hypersensitivity reactions, including urticaria, angioedema, bronchoconstriction, and anaphylaxis.
Analgesics
Morphine sulfate is the analgesic used in patients with ST-elevation myocardial infarction (STEMI) to help alleviate chest pain unrelieved by nitrates. It should be used with caution in patients with unstable angina and non-STEMI. It’s also used to promote relaxation.
Morphine sulfate
The most commonly used analgesic in ACLS, morphine is an opioid agonist. It’s a schedule II controlled substance indicated for chest pain that doesn’t respond to nitrates. Morphine is also given to patients with acute pulmonary edema (if blood pressure is adequate) because it dilates peripheral blood vessels and decreases preload, thus reducing pulmonary congestion and relieving shortness of breath.
Key points
Morphine sulfate
Opioid agonist that alters the perception of pain
Indications: pain, acute pulmonary edema
2 to 4 mg I.V. over 1 to 5 minutes; repeat every 5 to 30 minutes and titrate to effect
The doors of perception
As an opium alkaloid, morphine is thought to work through opiate receptors, altering the patient’s perception of pain. It also has a central depressant effect on respiration and the cough reflex center.
How to give it
Give 2 to 4 mg I.V. over 1 to 5 minutes; repeat every 5 to 30 minutes and titrate to the desired effect. Rapid I.V. administration of morphine may result in overdose because of the delay in maximum central nervous system (CNS) effect (30 minutes).
|
What can happen
Adverse reactions to morphine include respiratory depression, hypotension, bradycardia, shock, cardiac arrest, tachycardia, and hypertension. Apnea and respiratory arrest may also occur. Additionally, morphine may cause hypotension in volume-depleted patients. Correct hypovolemia before giving morphine.
What to consider
Use morphine with caution in patients with a compromised respiratory state because it may compromise respirations.
Don’t give CNS depressants with morphine because these drugs may potentiate its respiratory, sedative, and hypotensive effects.
If needed, reverse the effects of morphine with naloxone.
Antiarrhythmics
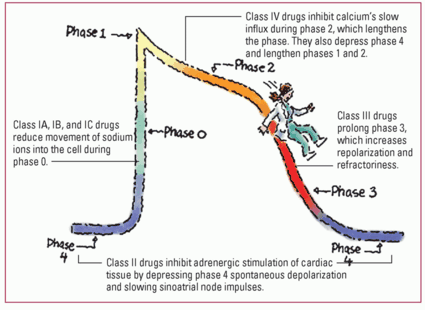
In general, antiarrhythmics are used to treat, suppress, or prevent three major mechanisms of arrhythmias: increased automaticity, decreased conductivity, and reentry. (See Antiarrhythmic drugs and the action potential, page 138.)
 Now I get it!
Now I get it!Antiarrhythmic drugs and the action potential
Each class of antiarrhythmic drugs acts on a different phase of the action potential and alters the heart’s electrophysiology. Here’s a summary of the four classes of antiarrhythmics and how each class affects the action potential.
|
 Memory jogger
Memory joggerTo remember the main differences among class IA, class IB, and class IC antiarrhythmics, just think of their names:
Class IA: Alters the myocardial cell membrane
Class IB: Blocks the rapid influx of sodium ions
Class IC: Slows Conduction.
Class is in session
Four classes of antiarrhythmic drugs exist: I, II, III, and IV. Class I is further subdivided into class IA, IB, and IC. Class IA alters the myocardial cell membrane; class IB blocks the rapid influx of sodium ions; and class IC slows conduction. (See “Guide to common antiarrhythmic drugs,” pages 327 to 328.) Several antiarrhythmic drugs aren’t included in the four classes. These drugs include adenosine and atropine. Epinephrine and vasopressin are also considered antiarrhythmic drugs. For class II antiarrhythmics, see “Beta-adrenergic blockers,” page 155. For class IV antiarrhythmics, see “Calcium channel blockers,” page 161.
Adenosine
Adenosine (Adenocard) is classified as a miscellaneous antiarrhythmic. A naturally occurring nucleoside, it’s used to diagnose and treat paroxysmal supraventricular tachyarrhythmia (PSVT). Adenosine may also be considered for use with regular, monomorphic wide-complex tachycardia (with a pulse) as a diagnostic maneuver. It acts on the AV node to slow conduction and inhibit reentry pathways.
How to give it
Give 6 mg I.V. by rapid bolus injection (over 1 to 3 seconds), followed by a rapid flush with 20 mL of normal saline solution. If the arrhythmia isn’t disrupted in 1 to 2 minutes, give 12 mg I.V. If necessary, you may give a third dose of 12 mg I.V. Remember, transient arrhythmias or asystole may occur after a rapid I.V. push.
What can happen
Adverse reactions to adenosine include hypotension, transient bradycardia, ventricular arrhythmias, flushing, chest pain, lightheadedness, nausea, and a metallic taste. However, because the half-life of adenosine is less than 10 seconds, adverse effects usually dissipate rapidly and are self-limiting.
Key points
Adenosine
Acts on the atrioventricular node to slow conduction and inhibit reentry pathways
Indications: first-line drug for paroxysmal supraventricular tachyarrhythmia
6 mg I.V. by rapid bolus injection (over 1 to 3 seconds)
12 mg I.V. if arrhythmia isn’t eliminated in 1 to 2 minutes (a third dose of 12 mg I.V. may be given if necessary)
Has a short half-life: Must be given as a very rapid I.V. push
What to consider
Monitor the patient’s heart rate and rhythm and blood pressure response to the drug.
Don’t give adenosine to patients with second- or third-degree heart block unless the patient has a pacemaker.
Don’t give to patients with asthma.
Use adenosine cautiously with other medications:
with carbamazepine (Tegretol)—Higher degrees of heart block may occur with concurrent use
with dipyridamole—A smaller dosage may be needed because the drug may potentiate the effects of adenosine
with methylxanthines: These drugs antagonize the effects of adenosine.
Caffeine may antagonize the effects of adenosine; a higher dosage may be needed or the patient may not respond at all.
Amiodarone hydrochloride
Amiodarone (Nexterone) is a ventricular and supraventricular antiarrhythmic used to treat recurrent VF, unstable VT, supraventricular arrhythmias, or rapid atrial fibrillation. It’s recommended as the first-line drug for shock-refractory VF or pulseless VT.
|
Take a load off
Amiodarone has mixed class IC and III antiarrhythmic effects, but it’s considered a class III drug. It increases the action potential duration (repolarization inhibition) and has alpha- and beta-adrenergic blocking properties. With prolonged therapy, amiodarone slows conduction through the AV node and prolongs the refractory period. Its vasodilating effect decreases cardiac workload and myocardial oxygen consumption. It also affects sodium, potassium, and calcium channels.
How to give it
Here’s how to administer amiodarone:
For cardiac arrest—Give 300 mg by I.V. push or I.O.; repeat with 150 mg I.V. push or I.O. in 3 to 5 minutes; dilute in 20 to 30 mL D5W.
For wide complex tachycardia (life-threatening ventricular arrhythmias)—Give a rapid I.V. infusion of 150 mg over the first 10 minutes (15 mg/minute) and repeat every 10 minutes as needed; follow with a slow infusion of 360 mg I.V. over 6 hours (1 mg/minute).
Maintenance infusion—Give 540 mg I.V. over 18 hours (0.5 mg/minute).
Maximum cumulative dose—Give 2.2 g I.V. over 24 hours.
Remember that amiodarone I.V. infusions exceeding 2 hours must be administered in glass or polyolefin bottles containing D5W.
Key points
Amidarone hydrochloride
First-line drug for shock refractory ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT)
Antiarrhythmic that increases the action potential duration
Indications: recurrent VF, unstable VT, supraventricular arrhythmias, atrial fibrillation, angina, and hypertrophic cardiomyopathy
For cardiac arrest give 300 mg I.V. push or I.O.; repeat with 150 mg I.V. push or I.O. in 3 to 5 minutes
For wide complex tachycardia (stable): give rapid infusion of 150 mg I.V. over first 10 minutes (15 mg/minute) and repeat every 10 minutes as needed; slow infusion of 360 mg I.V. over 6 hours (1 mg/minute) may be given
Maintenance infusion is 540 mg I.V. over 18 hours (0.5 mg/minute)
Maximum cumulative dose is 2.2 g I.V. per 24 hours
Drug half-life is up to 40 days
What can happen
Adverse reactions to amiodarone include bradycardia, hypotension, heart failure, arrhythmias, heart block, or sinus arrest. Such adverse reactions are more prevalent with high doses but usually resolve within about 4 months after drug therapy stops. Additional adverse reactions include pulmonary fibrosis, hepatotoxicity, hyperthyroidism, photosensitivity and skin discoloration, and corneal microdeposits.
What to consider
Watch the patient for hypersensitivity reactions to amiodarone.
Monitor the patient’s heart rate and rhythm and blood pressure response to the drug and monitor the ECG for QT prolongation.
Don’t give amiodarone to patients with severe sinoatrial (SA) node disease resulting in preexisting bradycardia, syncope caused by bradycardia or, unless a pacemaker is present, second- or thirddegree AV block.
When used with beta-adrenergic blockers or calcium channel blockers, amiodarone may cause sinus bradycardia, sinus arrest, and AV block; use together cautiously.
Remember that amiodarone can’t be removed by dialysis.
The half-life of amiodarone is up to 40 days.
Atropine sulfate
Atropine is classified as a miscellaneous antiarrhythmic. It’s used to treat symptomatic bradycardia and bradyarrhythmia (junctional or escape rhythm). It’s no longer recommended to treat asystole or bradycardic PEA.
Rate increase
Atropine is an anticholinergic (parasympatholytic) that blocks the effects of acetylcholine on the SA and AV nodes, thereby increasing SA and AV node conduction velocity. It also increases the sinus node discharge rate and decreases the effective refractory period of the AV node. The result is increased heart rate. (See How atropine speeds the heart rate, page 142.)
|
How to give it
Here’s how to administer atropine:
To treat bradycardia—Give 0.5 mg I.V. every 3 to 5 minutes as needed, not to exceed a total dose of 3 mg. Shorter dosing interval of 3 minutes and a higher dose may be used in severe clinical condition.
Remember that effects on the patient’s heart rate peak within 2 to 4 minutes after I.V. administration.
What can happen
Tachycardia may occur after higher doses of atropine. Signs of atropine overdose reflect excessive cardiovascular and CNS stimulation; treat with physostigmine (Antilirium).
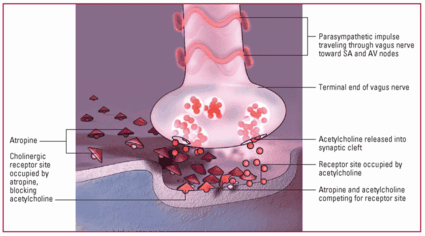
 Now I get it!
Now I get it!How atropine speeds the heart rate
When acetylcholine is released, the vagus nerve stimulates the sinoatrial (SA) and atrioventricular (AV) nodes, which inhibits electrical conduction. This slows the heart rate. The cholinergic blocker atropine competes with acetylcholine for binding with cholinergic receptors on SA and AV nodal cells. By blocking the effects of acetylcholine, atropine speeds the heart rate.
|
What to consider
Transplanted hearts lack vagal nerve innervation so atropine won’t be effective.
Monitor the patient’s heart rate and rhythm with drug administration.
Avoid using atropine for hypothermic bradycardia.
I.V. administration of less than 0.5 mg may cause paradoxical slowing of the heart rate.
Use atropine with caution in patients with myocardial ischemia and hypoxia because it increases myocardial oxygen demand.
Don’t give atropine with other anticholinergics or with drugs that have anticholinergic effects.
Atropine is ineffective for infranodal (type II) AV block and new third-degree AV block with wide QRS complexes because paradoxical slowing may occur.
Key points
Atropine sulfate
Blocks the effects of acetylcholine on the sinoatrial (SA) and atrioventricular (AV) nodes, thereby increasing SA and AV node conduction velocity
Indications: symptomatic bradycardia, bradyarrhythmia (junctional or escape rhythm.
For bradycardia: 0.5 mg I.V. every 3 to 5 minutes as needed, not to exceed total dose of 3 mg; shorter dosing interval of 3 minutes and a higher dose may be used with severe clinical condition
Ibutilide fumarate
Ibutilide (Corvert) is used for supraventricular arrhythmias. It’s most effective for the conversion of new-onset atrial fibrillation or atrial flutter. Ibutilide prolongs the action potential in isolated cardiac myocytes and increases atrial and ventricular refractoriness, namely class III electrophysiologic effects.
How to give it
Here’s how to administer ibutilide:
For adults weighing 132 lb (60 kg) or more—Give a 1 mg I.V. infusion over 10 minutes, diluted or undiluted; a second dose may be repeated after 10 minutes.
For adults weighing less than 132 lb—Give a 0.01-mg/kg I.V. infusion over 10 minutes; a second dose may be given after 10 minutes.
What can happen
Adverse reactions to ibutilide include AV block, bradycardia, bundle-branch block, hypotension, monomorphic and polymorphic VT, palpitations, prolonged QT interval, and ventricular extrasystoles. Polymorphic VT, including torsades de pointes, develops in 2% to 5% of patients after ibutilide is administered. Additionally, ibutilide may worsen ventricular arrhythmias.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree