Cardiovascular investigations In A Heartbeat
Blood tests
Cardiac catheterisation involves passing a catheter into the heart for diagnostic and therapeutic intervention. CXR is useful in suspected heart failure and can detect many intra-thoracic pathologies. CT can be used to stratify cardiovascular risk with calcium scoring. CT angiography allows the visualisation of vessels using contrast. CMR is a non-invasive technique that allows for the anatomical and functional assessment of the myocardium. It is superior to CT for soft tissue visualisation but unlike CT, is unable to detect and quantify calcium. MPS assesses the blood supply of the myocardium and has a role in the diagnosis and management of coronary artery disease. Echocardiography is a non-invasive technique that provides dynamic images of the heart. It is extremely useful in valvular heart disease and heart failure. Stress testing involves exerting the myocardium by exercise or a dobutamine infusion. It is used in suspected or known coronary artery disease. |
3.2 Blood tests
Cardiac biomarkers are widely available, relatively non-invasive and cost-effective. When interpreted appropriately, they provide a means to assist decision making.
3.2.1 Cardiac troponin (T and I)
Troponin is a component of skeletal and cardiac muscle which facilitates muscle contraction. It is a protein complex made up of three protein subunits: Troponin T (TnT), Troponin C (TnC) and Troponin I (TnI). Troponin T and I are cardio-specific and, if detected in the blood beyond the normal range, act as strong indicators of myocardial damage and necrosis. They are released into the bloodstream in response to myocardial ischaemia and necrosis and are currently the most sensitive (84–90%) and specific (81–95%) biomarkers in the detection of myocardial infarction. Troponin can also be elevated in several other circumstances including sepsis, pulmonary embolism, acute pulmonary oedema, aortic dissection, myocarditis and chronic kidney disease.
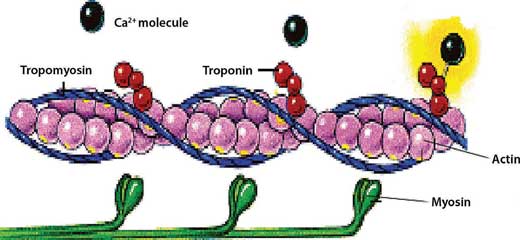
Figure 3.1 – Myofilament structure.
In an acute MI:
- Serum levels are elevated as early as 2 hours of chest pain, peak at 12–18 hours and remain elevated for approximately 14 days
- Different hospitals use different assays and therefore the normal range is variable
- Measure troponin levels at time of presentation and again at 10–12 hours after onset of symptoms. Levels may be normal if taken very early after onset
- The level of troponin is directly related to risk of death from acute coronary syndrome (ACS)
- A normal troponin 6 hours after the onset of chest pain does not exclude the diagnosis of MI.
3.2.2 Creatine kinase (CK)
CK-MB isoenzyme is a relatively cardiospecific biomarker (compared to CK-BB and CK-MM, which are also found in the brain and skeletal muscle respectively); however, since the advent of troponin, its use in clinical practice is limited.
It may still play a role in suspected re-infarction after MI:
- CK-MB falls after 36 to 48 hours; therefore an elevated level after 5 days, for example, could point towards re-infarction
- Troponin levels, however, rise rapidly even on abnormal baselines in re-infarction and remain the mainstay in the diagnosis of an acute myocardial infarction, including re-infarction.
3.2.3 Brain natriuretic peptide (BNP)
BNP and ANP (atrial natriuretic peptide) are polypeptides that are secreted by the heart in response to excessive stretching (ventricles secrete BNP and atria secrete ANP). They decrease systemic vascular resistance and central venous pressure as well as increase salt and water excretion by the kidney.
- High levels, therefore, reflect a high blood volume and possible volume overload (i.e. heart failure)
- In clinical practice, BNP is used because it has a greater half-life than ANP.
- BNP is secreted with an inactive N-terminal fragment (NT-proBNP) – this is actually more useful than BNP as it has an even longer half-life
- It has a high sensitivity (93%) and specificity (98%) for congestive heart failure although increasing age as well as a multitude of other conditions, such as renal failure, sepsis, COPD, and pulmonary hypertension, are also associated with increased BNP levels. Likewise, BNP levels can remain within the normal range in treated heart failure.
EXAM | In Figure 3.2, notice that in the early hours after an MI, troponin and CK-MB levels can be normal, giving a falsely negative result. Also note that at 48 hours, CK-MB falls to normal so an MI may go undetected, whereas troponin remains elevated. |
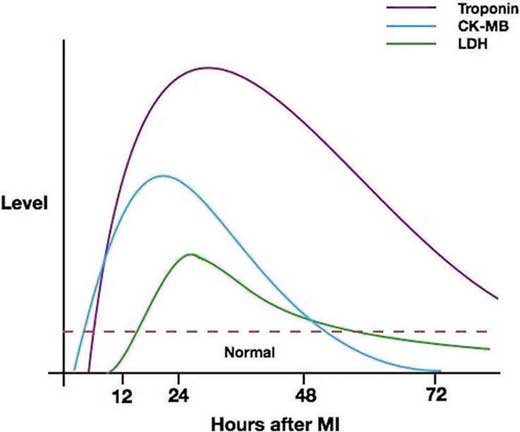
Figure 3.2 – Cardiac biomarker levels following a myocardial infarction.
3.3 Electrocardiography (ECG)
The ECG is the most widely used investigation in cardiology and is addressed in Chapter 4. Exercise ECG is covered at the end of this chapter.
3.4 Cardiac catheterisation
Cardiac catheterisation involves the passage of catheters into the heart under radiographic guidance in order to visualise the structures of the heart including the coronary blood vessels, the chambers and the valves. It may be performed for diagnostic or therapeutic purposes, often as a day case procedure – made possible by its minimally invasive nature.
The procedure is performed initially by identifying a site of entry, usually a peripheral artery or vein. The site is cleaned and a local anaesthetic is injected. Access to the vessel is secured using the Seldinger technique, allowing an introducer sheath to be situated within the vessel, with the port sited externally through which guide wires are passed up into the aorta and/or heart. The location of the wire is confirmed by the use of a portable X-ray generator with real-time feedback. A catheter is then advanced over the guide wire and the guide wire removed once the catheter is in the correct position. A variety of procedures may then be performed at this stage and can be categorised according to the side of the heart investigated.
3.4.1 Left heart catheterisation
Catheterisation of the left heart is primarily performed to delineate the anatomy of the coronary arteries, where it is termed coronary angiography. Access is typically via the radial artery. Alternatively, the femoral artery may be utilised. Left heart catheterisation may be used as a purely diagnostic procedure, but often incorporates therapeutic intervention. Its indications include:
- Assessment of coronary vessel anatomy: angiography is utilised to visualise coronary blood flow and identify pathology such as stenosis. Identification of vessel stenosis in suspected acute coronary syndrome (i.e. primary PCI (pPCI)) or stable angina is the most common indication. Percutaneous coronary intervention (e.g. POBA (plain old balloon angioplasty: where the luminal stenosis has been treated by the inflation of a balloon only, without application of stents) or coronary artery stenting) may then be performed to relieve stenosis.
- Assessment of heart valves: pressure gradients across valves can be accurately measured to evaluate patients with valvular heart disease, particularly if echocardiography is non-diagnostic or prior to valve surgery.
- Transcatheter valve replacement (TVR): a collapsible aortic or mitral valve is introduced via a catheter and implanted using radiographic guidance. This is discussed further in Chapter 12.
- Assessment of haemodynamics: various components of haemodynamic status can be accurately measured, including pressure and waveform analysis of the left ventricle and aorta. Haemodynamic monitoring plays an important role in cardiovascular observation.
3.4.2 Right heart catheterisation
This is usually performed to assess intra-cardiac and pulmonary pressures, cardiac output and oxygen saturations. Access is usually via large veins (femoral, internal jugular or subclavian) under local anaesthetic.
Common indications for right heart catheterisation include:
- Assessment of pulmonary vessel pressures: The pulmonary capillary wedge pressure (PCWP) reflects left atrial pressure and is a sensitive means of assessing ventricular output. It is used to delineate causes of acute pulmonary oedema, in guiding fluid resuscitation in the haemodynamically compromised, and in the assessment of patients with mitral valve stenosis. It is also used in patients with suspected pulmonary hypertension.
- Assessment of right atrial and ventricular pressures.
- Pre-operative assessment prior to cardiac and non-cardiac surgery.
- Evaluation of structural heart disease such as atrial septal defects and other congenital heart disease.
3.4.3 Complications and contraindications
Cardiac catheterisation is a relatively safe procedure with a mortality rate of less than 0.1%. Serious complications are rare but can occur. They include myocardial infarction (<0.1%), stroke, false aneurysm, arrhythmias, death, contrast reaction and contrast-induced acute kidney injury. Radial artery puncture can result in compartment syndrome if bleeding post-catheterisation is not stemmed adequately. Femoral artery bleeding post-procedure is potentially more risky with the potential for retroperitoneal haemorrhage which can, rarely, result in death. Therefore, decisions to undertake invasive procedures should be on an individual patient basis and require careful consideration of risks and benefits. In the context of acute ST-elevation myocardial infarction, coronary angioplasty may offer potentially life-saving treatment. Alternative investigations may be required in patients with suspected angina who are considered high risk for coronary angiography.
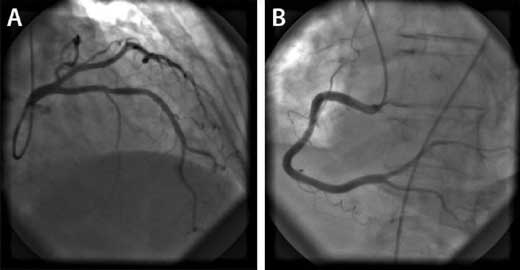
Figure 3.3 – (A) Left coronary artery and (B) Right coronary artery seen on coronary angiography.
3.5 Chest radiography (CXR)
A chest radiograph should be performed in all breathless patients as it provides useful information regarding the shape and size of the heart, the pulmonary vessels and the lung fields. It may help distinguish between suspected cardiac disease and pulmonary disease. A CXR is ideally performed in full inspiration, postero-anteriorly (PA); however, an antero-posterior (AP) projection may be used in acutely ill patients or those with restricted mobility.
As there is exposure to radiation (equivalent to 2.5 days of background radiation), it should be avoided in pregnancy; however, this is not an absolute contraindication.
3.5.1 Interpretation of a radiograph
- Heart
- cardiothoracic ratio (cardiac width:thoracic width) – if it is greater than 1:2 (50%) in a PA film, there may be cardiomegaly. As AP films over-estimate the size of the heart, they are not reliable in assessing cardiomegaly.
- Lung fields
- interstitial or alveolar airspace shadowing can indicate pulmonary congestion
- Kerley B lines (horizontal lines at the lung edge) may indicate pulmonary oedema
- effusions (blunted costophrenic angles).
- interstitial or alveolar airspace shadowing can indicate pulmonary congestion
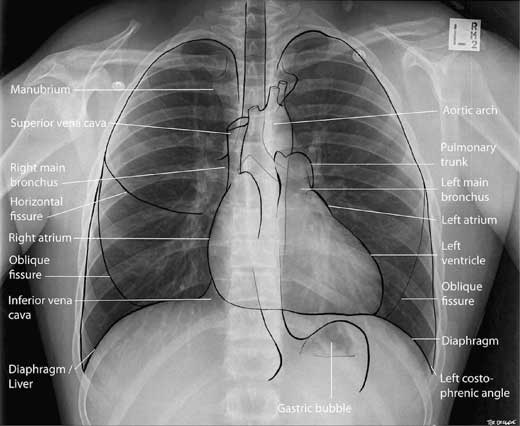
Figure 3.4 – Normal chest radiograph (PA).
3.6 Computerised tomography (CT)
Cardiac CT scanning utilises computerised tomography technology and radio-contrast to generate accurate images of the heart and coronary vessels. Its use is not yet routine in clinical practice but plays an important role in the assessment of heart disease. Although CT technology typically employs 2-dimensional imaging, the advent of multi-detector row CT (MDCT) with its substantially superior spatial and temporal resolutions, in conjunction with reconstruction software, allows the 3-dimensional representation of cardiac structures such as the chambers, the coronary vessels and the great vessels.
3.6.1 Indications
- Evaluation of coronary anatomy
- detecting atherosclerosis: cardiac CT scanning allows the detection and quantification of coronary calcium. Total plaque burden and degree of atherosclerosis can consequently be determined (see Guidelines).
- CT angiography: utilises contrast to provide detailed images of the coronary arteries. Although coronary angiography remains the gold standard in the evaluation of coronary artery anatomy, CT angiography provides a non-invasive alternative (see Guidelines).
- detecting atherosclerosis: cardiac CT scanning allows the detection and quantification of coronary calcium. Total plaque burden and degree of atherosclerosis can consequently be determined (see Guidelines).
- Structure and function of the heart
- assessment of cardiac masses: thrombus, tumours
- assessment of pericardial disease: constrictive pericarditis, pericardial masses
- contrast-enhanced studies can define ventricular volumes, ejection fractions, wall thickening and wall motion with high accuracy
- assessment of cardiac masses: thrombus, tumours
- Evaluation of the pulmonary vein anatomy in the management of atrial fibrillation radiofrequency ablation
- Evaluation of suspected pulmonary embolism
- evaluation of suspected thoracic aortic aneurysm and aortic dissection.
GUIDELINES: The use of CT calcium scoring in coronary artery disease (NICE, 2010)
NICE currently recommends CT calcium scoring in patients where stable angina cannot be diagnosed or excluded based on clinical assessment alone, and where the estimated likelihood of coronary artery disease is 10–29%.
GUIDELINES: The use of CT angiography (European Society of Cardiology, 2013)
The European Society of Cardiology currently recommends the use of CT angiography in patients with intermediate pre-test likelihood of coronary artery disease with equivocal stress test results or uninterpretable ECGs. Its high negative predictive value may effectively rule out coronary stenosis in these patients.
3.6.2 Contraindications
CT is a relatively safe and non-invasive investigation, but since it involves significant radiation exposure and often the use of contrast, it must be used cautiously in patients with renal impairment and is contraindicated in pregnant women.
3.7 Cardiac MRI
CMR is a non-invasive imaging technique that obtains images of the heart by pulse sequencing. Controlled magnetic field pulses disturb the alignment of hydrogen nuclei in the body and signals received can be analysed to produce an image. By this process, CMR is able to accurately define various structures and functions of the heart.
The advantages of CMR give it a unique role in the evaluation of many cardiac conditions:
- Its use is not limited by body habitus, allowing evaluation in patients with limited acoustic windows during echocardiography.
- Utilises high spatial and temporal resolutions to allow accurate assessment of cardiovascular function and structure. Facilitates visualisation of the heart and thoracic structures in several planes.
- CMR is excellent for visualising anomalous arterial or venous connections commonly seen in congenital heart disease.
- It offers much better visualisation of right heart size and function than echocardiography.
3.7.1 Indications
- Ischaemic heart disease: CMR may be utilised during the diagnostic period in patients with intermediate pretest probability of IHD who are unsuitable for stress testing or have uninterpretable ECGs, to assist in making a diagnosis of ischaemic heart disease, and identifying patients who may be suitable for interventional procedures (see Myocardial perfusion scanning)
- Myocardial infarction and scarring: CMR is able to accurately define areas of myocardial necrosis and scarring. This may be used in the assessment of patients post-ACS and in identifying patients likely to improve after revascularisation. CMR is also the gold standard for the detection of left ventricular thrombus.
- Heart failure: CMR is one of the most accurate imaging modalities in assessing functional and structural abnormalities of the ventricles, underscoring its benefit in the evaluation of patients with chronic heart failure. It may also be used to distinguish the underlying aetiology, as well as provide prognostic information in these patients. Guidelines currently recommend that CMR be considered in patients with heart failure to evaluate LV function and in those with limited echocardiographic studies.
- Cardiomyopathies: CMR is highly important in the diagnosis and management of cardiomyopathies. In hypertrophic cardiomyopathy, it facilitates accurate measurement of the interventricular septum which can be challenging with echocardiography.
- valve disease: CMR is particularly useful in monitoring changes in LV volumes in patients with valvular disease, especially where echocardiographic studies are technically limited or unsuitable
- congenital heart disease: CMR is very useful in the diagnosis and management of congenital heart disease. It is excellent at detecting anomalous arterial and venous connections commonly associated with congenital heart disease. It also facilitates accurate serial assessment of ventricular size and function in young patients whilst avoiding repeated exposure to radiation.
- valve disease: CMR is particularly useful in monitoring changes in LV volumes in patients with valvular disease, especially where echocardiographic studies are technically limited or unsuitable
Myocardial perfusion scanning (MPS) is a form of nuclear stress testing performed using T1-weighted sequencing to observe the passage of gadolinium contrast through the heart. The contrast is taken up by the myocardium and the resultant signal intensity correlates with contrast concentration in the tissue. Low signal in a particular area indicates hypoperfusion of that myocardium. It may be used in the assessment of coronary artery disease (see Guidelines) as well as myocardial perfusion in the context of ACS and revascularisation.
GUIDELINES: Use of myocardial perfusion scanning in stable angina (NICE, 2010)
NICE currently recommends ‘non-invasive functional imaging’ in patients where stable angina cannot be diagnosed or excluded based on clinical assessment alone, and where the estimated likelihood of coronary artery disease is 30–60%. This includes the use of myocardial perfusion scintigraphy with single photon emission computed tomography (MPS with SPECT).
3.7.2 Contraindications
The strong magnetic field of CMR creates potential dangers for patients with implantable metal objects. Therefore great care and careful consideration must be exercised in patients with permanent pacemakers, implantable cardioverter defibrillators (ICDs), jewellery, aneurysm clips, cochlear implants, joint prostheses, etc. Sedation may be required in paediatric patients and those where claustrophobia is problematic. Furthermore, the use of contrast in MPS requires careful consideration in patients with renal impairment and in pregnant patients.
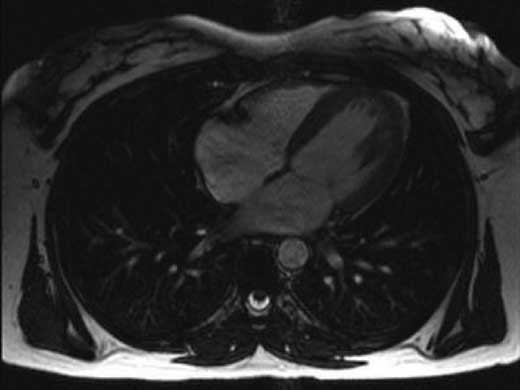
Figure 3.5 – Cardiac MRI.
3.8 Echocardiography
Echocardiography uses ultrasound technology to visualise the heart and underlying structures. It allows dynamic visualisation of the heart in both two and three dimensions (2D and 3D). Echocardiography is an extremely valuable investigation and handheld devices are now in use in clinical practice.
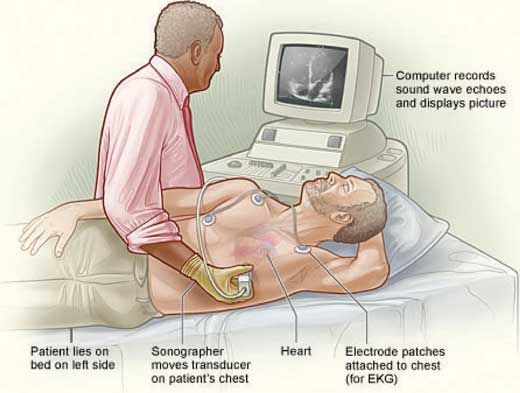
Figure 3.6 – Echocardiography.
Echocardiography can be performed using two different methods:
- Transthoracic echocardiography (TTE) is the standard procedure and involves placing the ultrasound probe on the chest and imaging the heart through the chest wall. This technique is non-invasive and provides an accurate and fast assessment of the heart chambers, valves, aorta and pericardium. It can, however, yield poor quality images in, for example, overweight patients or in patients with obstructive airways disease. Common views obtained from a TTE include the parasternal long axis view, parasternal short axis view, apical 5-, 4-, and 3-chamber views, and the subcostal view.
- Transoesophageal echocardiography (TOE) is an alternative method that is invasive and requires sedation. The ultrasound probe is passed down the oesophagus and positioned behind the left atrium. This method has greater sensitivity than TTE and produces high resolution images. It is particularly useful for visualising posterior structures of the heart (left atrium) and the surrounding vessels (pulmonary veins and thoracic aorta). It is the investigation of choice for the diagnosis of infective endocarditis.
Various modes can be utilised to perform anatomical and functional assessment of the heart.
- Two-dimensional (2D) echocardiography provides cross-sectional images of the heart and allows visual assessment of left ventricular wall thickness and estimation of ejection fraction.
- Three-dimensional (3D) echocardiography uses multiple two-dimensional ‘slices’ to create a three-dimensional image. It can be used to accurately calculate LV volume and function.
- Doppler echocardiography uses the Doppler principle to measure the velocity and direction of blood in the heart and blood vessels. This is useful in the assessment of flow and severity of valvular disease.
- Colour Doppler represents velocity and direction of blood flow as colours on a display: movement towards the transducer is red, away is blue, and turbulent flow is represented by a mosaic pattern. Applied clinically, stenotic valves demonstrate an increase in velocity with a high pressure gradient while valvular regurgitation shows a reversal of blood flow and turbulence.
- Stress echocardiography is discussed in the next section.
3.8.1 Indications
- Murmur with clinical suspicion of heart disease
- Valvular disease: diagnosis and assessment of severity of stenosis and/or regurgitation or presence of vegetations
- Assessment of left ventricular size and function
- Diagnosis and management of infective endocarditis
- Cardiomyopathy, congenital heart disease
- Pericardial disease, particularly pericardial effusion and cardiac tamponade.

Figure 3.7 – Echocardiography of the heart. Four-chamber view, left side of the heart to the right, apex down.
3.9 Stress testing
Cardiac stress testing is a useful tool in the assessment and management of coronary artery disease. It can provide important diagnostic and prognostic information. The heart is investigated while under stress – induced either by exercise (usually using a treadmill) or pharmacologically (usually dobutamine). The Bruce Protocol is the most widely used protocol and aims to increase workload on the heart gradually in stages (up to 7 stages, each lasting 3 minutes). The Modified Bruce Protocol is more appropriate in patients with limited exercise capacity, because it starts at a lower workload: it may be used within one week of myocardial infarction. Pharmacological stress may be used in situations where exercise is not possible – e.g. if the patient is unable to mobilise or cannot exercise to an adequate cardiac workload.
Stress testing is generally a safe procedure; however, there have been reports of ventricular arrhythmia, myocardial infarction and death during testing, so it is important to use these tests judiciously. Absolute contraindications include acute MI (within 2 days), unstable angina, aortic dissection, severe aortic stenosis, uncontrolled arrhythmias, acute pulmonary embolism (PE) and uncontrolled symptomatic heart failure. It is also important that an emergency crash trolley is nearby and accessible, as there is a risk of collapse during the test. Operators and nurses should be equipped with resuscitation skills.
// Why? //
Why dobutamine?
Dobutamine is a synthetic catecholamine which stimulates beta-1 receptors on the heart to act as both a chronotrope (increases heart rate) and inotrope (increases myocardial contractility). It is superior to exercise in detecting myocardial ischaemia using echocardiography.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


