Cardiovascular Manifestations of Systemic Disease
Sachin S. Goel
Several systemic diseases involve the cardiovascular system, with important therapeutic and prognostic implications. It is vital for cardiologists to recognize, manage, and prevent cardiovascular involvement in various systemic diseases. This chapter reviews the cardiovascular manifestations of various systemic disorders.
I. RHEUMATOLOGIC DISORDERS
A. Rheumatoid arthritis (RA) is one of the commonest forms of chronic inflammatory polyarthritis resulting in joint destruction and deformation. It affects 1% to 3% of the population and is more common in women. It is characterized by chronic symmetrical polyarthritis that typically affects small joints of the hand, such as metacarpophalangeal and proximal interphalangeal joints, in addition to wrists and knees, and spares the thoracolumbar spine and distal interphalangeal joints. The most common cardiovascular manifestations of RA are as follows:
1. Pericarditis is very common and can be present in nearly 50% of patients with RA. It can vary from acute pericarditis and chronic asymptomatic effusive pericarditis to cardiac tamponade or chronic constrictive pericarditis, with significant hemodynamic consequences. Most cases with uncomplicated acute pericarditis will respond to nonsteroidal anti-inflammatory drugs (NSAIDs). Corticosteroid therapy may be needed for patients with severe pericarditis. Pericardiocentesis or surgical drainage may be required in cases of tamponade.
2. Coronary artery disease (CAD). Patients with RA have increased mortality compared with the general population and the leading cause of death is cardiovascular disease. Patients with RA have accelerated atherosclerosis, likely a result of chronic systemic inflammation and use of corticosteroids. After controlling for traditional risk factors of atherosclerosis, patients with RA have been shown to have two to three times greater risk of CAD compared with controls. In the large prospective Nurses’ Health Study, women with RA were found to have a twofold higher risk of myocardial infarction compared with controls. In addition to disease-modifying drugs to reduce systemic inflammation, aggressive lifestyle modification, including tight control of blood pressure and low-density lipoprotein cholesterol, seems warranted.
3. Cardiomyopathy. RA can cause granulomatous inflammation of the myocardium leading to cardiomyopathy or involve the conduction system resulting in varying degrees of heart block. Rarely, secondary amyloidosis can occur in RA, leading to an infiltrating cardiomyopathy.
4. Valvular disease. A small proportion of patients with RA can have valvular involvement in the form of rheumatoid nodules; however, clinically significant valve disease is very rare.
B. Systemic lupus erythematosus (SLE) is a systemic autoimmune disease that occurs more commonly in women and is characterized by a wide range of organ involvement, including arthritis, dermatitis, glomerulonephritis, serositis, and hematologic abnormalities. Drug-induced lupus can occur with various cardiac medications, including procainamide, quinidine, and hydralazine, and this is associated with the development of anti-histone antibodies. SLE can affect the cardiovascular system in various ways:
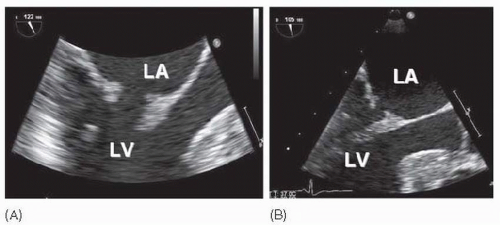
1. Valvular disease is the most common type of cardiac involvement in SLE. The characteristic valvular lesions in SLE are nonmobile, noninfectious vegetations on the atrial aspect of the mitral valve or the arterial aspect of the aortic valve, referred to as Libman-Sacks endocarditis (Fig. 39.1). Studies have shown that valvular involvement is very common in SLE and occurs in > 50% of patients. The most common valvular abnormality is valvular thickening, followed by vegetations and valvular regurgitation or stenosis. Serial echocardiography should be performed to monitor for progression of valve disease. The vegetations can embolize and cause stroke or myocardial infarction in rare cases.
2. Pericarditis is very common in SLE and has been shown to occur in > 50% to 60% of patients. Associated pericardial effusion is usually exudative, with elevated protein and low glucose concentration, and infection must be ruled out in the setting of concomitant immunosuppressive therapy. Cardiac tamponade and chronic constrictive pericarditis can also occur.
3. Coronary artery disease. Premature coronary atherosclerosis has been shown to occur commonly in patients with SLE compared with age-matched controls. CAD can also manifest as coronary arteritis, thrombosis in the presence of antiphospholipid antibody syndrome (APLA—see Section I.C) or, rarely, embolism from Libman-Sacks endocarditis.
4. Myocardial dysfunction in patients with SLE can result from ischemia, valve disease, or long-standing hypertension. Patients with peripheral skeletal myositis have an increased risk of lupus myocarditis.
5. Conduction system disease with complete heart block can occur in infants born to mothers with SLE, particularly those with anti-Ro and anti-La antibodies. Women with SLE contemplating pregnancy should undergo screening for these antibodies prior to pregnancy and, if present, should undergo fetal echocardiography to screen for conduction abnormalities and myocardial dysfunction. There is some evidence suggesting a role for intrauterine dexamethasone in reversing fetal myocarditis and slowing conduction disease.
C. Antiphospholipid antibody syndrome is characterized by the presence of antiphospholipid antibodies or lupus anticoagulant, recurrent venous or arterial thrombosis, and miscarriages. APLAs can occur independently, referred to as primary APLAs, or can be associated with other autoimmune diseases such as SLE (10% to 30%) and are then referred to as secondary APLAs. Valvular disease is common in APLAs and is characterized by noninfectious vegetations similar to those seen in SLE (Libman-Sacks endocarditis). Management of arterial or venous thrombosis or significant valvular vegetations includes anticoagulation therapy with warfarin. Monitoring anticoagulant effect while on heparin or warfarin may be difficult, as these patients can have prolonged partial thromboplastin time or international normalized ratio at baseline, in which case monitoring of anticoagulant effect can be done using activity levels of factors II and X.
D. Scleroderma or systemic sclerosis is a rare autoimmune disorder, characterized by vasospasm, microvascular occlusion, and fibrosis of skin and multiple organs. Diffuse or progressive systemic sclerosis (PSS) results in widespread cutaneous and visceral involvement. Limited scleroderma, also known as CREST syndrome, is characterized by calcinosis cutis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia. Cardiovascular involvement can occur in progressive as well as limited scleroderma.
1. Pericardial disease in the form of fibrinous pericarditis is present in over 70% of patients on autopsy studies, though it is clinically manifest as symptomatic pericarditis in only about 15% to 30% of patients. Small pericardial effusions can be detected in about 40% of patients by echocardiography, but are rarely significant. Acute pericarditis may be treated with NSAIDs, with close monitoring of renal function. Corticosteroids carry the risk of inducing scleroderma renal crisis.
2. Pulmonary hypertension (PH) is responsible for significant morbidity and mortality in patients with scleroderma and is more common in the limited type. Autopsy studies have shown histopathological changes consistent with PH in 65% to 80% of patients with scleroderma; however, < 10% of patients manifest PH clinically. Patients with scleroderma and PH appear to have a worse prognosis compared with those with primary PH, with a 2-year survival of < 50%. Drugs for PH, such as prostacyclins (epoprostenol, treprostinil, and iloprost), endothelin receptor antagonists (bosentan and ambrisentan), and phosphodiesterase inhibitors (sildenafil and tadalafil), have been studied in patients with scleroderma and PH. Some of these studies have demonstrated improvement in the 6-minute walk test, exercise capacity, and cardiopulmonary hemodynamics; however, no improvement in mortality has been demonstrated. Echocardiography should be used to screen for asymptomatic PH.
3. Scleroderma renal crisis is defined as the new onset of accelerated hypertension or rapidly progressive oliguric renal failure during the course of systemic sclerosis. It is usually associated with rising creatinine, thrombocytopenia, microangiopathy, and signs and symptoms of congestive heart failure. Scleroderma renal crisis occurs in about 10% of patients with scleroderma and is more common in the diffuse form of the disease. Angiotensin-converting enzyme inhibitors are the mainstay of therapy.
4. Myocardial involvement with patchy fibrosis can occur in patients with scleroderma. Epicardial coronary arteries are usually normal on angiography; however, ischemia can occur secondary to microvascular vasospasm. Diastolic dysfunction has been commonly found in these patients. Electrical abnormalities such as frequent ectopy, supraventricular arrhythmias, and nonsustained ventricular tachycardia (VT) can occur in patients with PSS. The risk of sudden cardiac death is higher in those with a history of syncope.
E. Seronegative spondyloarthropathies include HLA-B27 antigen—associated arthropathies such as ankylosing spondylitis, reactive arthritis, psoriatic arthritis, and inflammatory bowel disease—associated arthritis. These disorders are characterized by
involvement of the spine and sacroiliac joints and inflammation of tendons, ligaments, and their insertion points into bones (enthesitis). In contrast to RA and SLE, these disorders occur more commonly in males. Ankylosing spondylitis results in ankylosis, sacroilitis, and asymmetric peripheral arthritis. Reactive arthritis is characterized by conjunctivitis, genital ulcers, and asymmetric peripheral arthritis. Proximal aortitis with or without aortic regurgitation and conduction disturbances are most commonly associated with ankylosing spondylitis and reactive arthritis. Proximal aortitis can lead to thickening, stiffness, and dilatation of the aortic root with aortic regurgitation. Aortic or mitral valve thickening with nodularities of the aortic cusps and thickening of the anterior mitral valve leaflet resulting in a characteristic subaortic bump are commonly observed valvular abnormalities in patients with ankylosing spondylitis. Extension of the subaortic inflammation and fibrotic process into the basal septum can result in conduction abnormalities such as heart block, which is usually at the level of the atrioventricular (AV) node. Other less common cardiac abnormalities include pericarditis, diastolic dysfunction, and supraventricular arrhythmias. F. Dermatomyositis (DM) and polymyositis (PM) are idiopathic inflammatory myopathies characterized by proximal skeletal muscle weakness and elevated levels of muscle enzymes, such as creatine kinase and aldolase. DM is characterized, in addition, by skin involvement such as erythematous scales on the knuckles (Gottron’s papules), knees, and elbows, and periorbital swelling and violaceous rash around the eyelids (heliotrope rash). DM can be part of a paraneoplastic syndrome, particularly in the elderly. Cardiovascular manifestations of DM and PM include pericarditis, conduction abnormalities, and congestive heart failure secondary to myocarditis that can be focal or generalized and may be steroid responsive. Cardiac magnetic resonance imaging (MRI) with delayed gadolinium enhancement may be useful in monitoring response to therapy. Coronary vasculitis is a rare manifestation. The differentials for muscle weakness include the following: corticosteroid myopathy, which generally affects skeletal muscle but not cardiac or respiratory muscle and is associated with a normal creatine kinase, and statin myopathy, which can be differentiated based on history of statin use and myalgias or with electromyography and biopsy if needed. Management of DM and PM includes corticosteroids, and adjunctive therapies include methotrexate, azathioprine, and intravenous immunoglobulin (IVIg).
involvement of the spine and sacroiliac joints and inflammation of tendons, ligaments, and their insertion points into bones (enthesitis). In contrast to RA and SLE, these disorders occur more commonly in males. Ankylosing spondylitis results in ankylosis, sacroilitis, and asymmetric peripheral arthritis. Reactive arthritis is characterized by conjunctivitis, genital ulcers, and asymmetric peripheral arthritis. Proximal aortitis with or without aortic regurgitation and conduction disturbances are most commonly associated with ankylosing spondylitis and reactive arthritis. Proximal aortitis can lead to thickening, stiffness, and dilatation of the aortic root with aortic regurgitation. Aortic or mitral valve thickening with nodularities of the aortic cusps and thickening of the anterior mitral valve leaflet resulting in a characteristic subaortic bump are commonly observed valvular abnormalities in patients with ankylosing spondylitis. Extension of the subaortic inflammation and fibrotic process into the basal septum can result in conduction abnormalities such as heart block, which is usually at the level of the atrioventricular (AV) node. Other less common cardiac abnormalities include pericarditis, diastolic dysfunction, and supraventricular arrhythmias. F. Dermatomyositis (DM) and polymyositis (PM) are idiopathic inflammatory myopathies characterized by proximal skeletal muscle weakness and elevated levels of muscle enzymes, such as creatine kinase and aldolase. DM is characterized, in addition, by skin involvement such as erythematous scales on the knuckles (Gottron’s papules), knees, and elbows, and periorbital swelling and violaceous rash around the eyelids (heliotrope rash). DM can be part of a paraneoplastic syndrome, particularly in the elderly. Cardiovascular manifestations of DM and PM include pericarditis, conduction abnormalities, and congestive heart failure secondary to myocarditis that can be focal or generalized and may be steroid responsive. Cardiac magnetic resonance imaging (MRI) with delayed gadolinium enhancement may be useful in monitoring response to therapy. Coronary vasculitis is a rare manifestation. The differentials for muscle weakness include the following: corticosteroid myopathy, which generally affects skeletal muscle but not cardiac or respiratory muscle and is associated with a normal creatine kinase, and statin myopathy, which can be differentiated based on history of statin use and myalgias or with electromyography and biopsy if needed. Management of DM and PM includes corticosteroids, and adjunctive therapies include methotrexate, azathioprine, and intravenous immunoglobulin (IVIg).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree